Burden of chronic kidney disease
Page highlights:
- In 2023, chronic kidney disease accounted for 1.1% of the total burden of disease in Australia.
- In 2018, chronic kidney disease accounted for 2.5% of total burden in First Nations people.
What is burden of disease?
Burden of disease is a measure of the years of healthy life lost from living with or dying from disease and injury.
The measure used is the ‘disability adjusted life year’ (DALY). This measure combines health loss from living with illness and injury (non-fatal burden, or years of life lost due to disability – YLD) and dying prematurely (fatal burden, or years of life lost – YLL) to estimate total health loss (total burden, or DALY).
Burden of disease estimates seek to capture both the quantity and health-related quality of life, and to reflect the magnitude, severity and impact of disease and injury within a population. Burden of disease does not quantify the social or financial consequences of disease and injury.
The Australian Burden of Disease Study provides estimates for over 200 diseases and injuries in Australia, including chronic kidney disease (CKD), which is included as part of the Kidney and Urinary Disease group. Note that the definitions of CKD in this study are different from those used to define CKD in other sections of this report.
Further information can be found in Australian Burden of Disease Study 2023.
Note: The Australian Burden of Disease Study 2023 does not include estimates by Remoteness areas, Socioeconomic groups or risk factors. The most recent estimates are presented in the Australian Burden of Disease Study: Impact and causes of illness and death in Australia 2018 and Australian Burden of Disease Study 2018: Interactive data on risk factor burden reports.
In 2023, Australians lost an estimated 63,400 years of healthy life (DALY) due to CKD, equivalent to 2.4 DALY per 1,000 population (AIHW 2023).
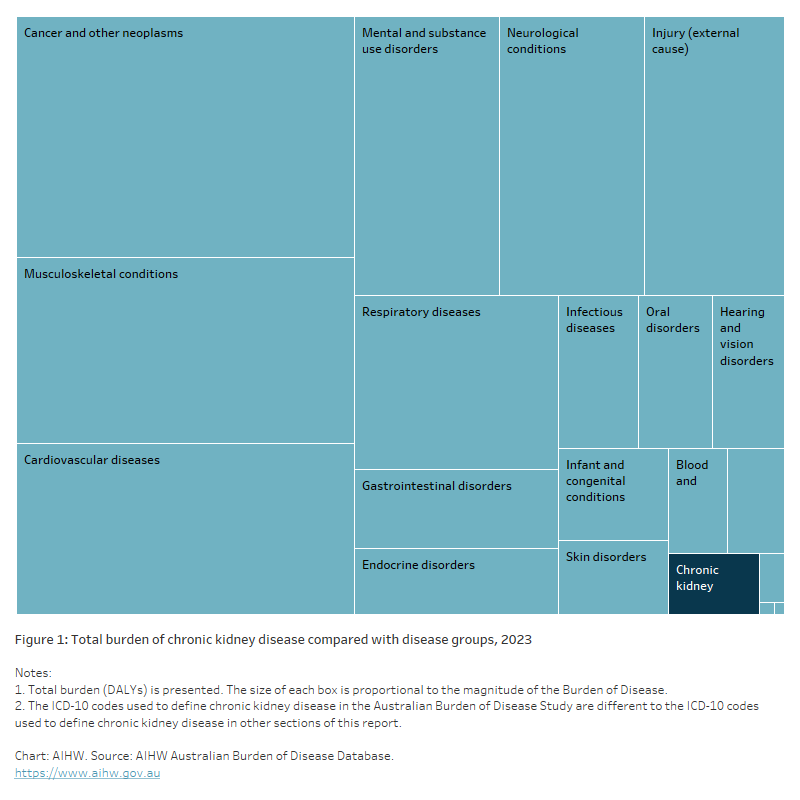
CKD accounted for 1.1% of the total burden of disease in Australia in 2023 (1.2% males, 1.1% females) (Figure 1).
Most of the burden from CKD (72%) came from years of life lost to premature death (YLL), with the remainder (28%) from years lived with illness (YLD).
Figure 1: Total burden of chronic kidney disease compared with disease groups, 2023
The tree chart shows the burden of disease groups (such as cancer and other neoplasms, cardiovascular diseases and musculoskeletal conditions) compared with the burden of CKD. In 2023, CKD accounted for 63,448 DALY. In contrast, the largest burden of disease group – Cancer and other neoplasms – accounted for 934,551 DALY.
Variation by age and sex
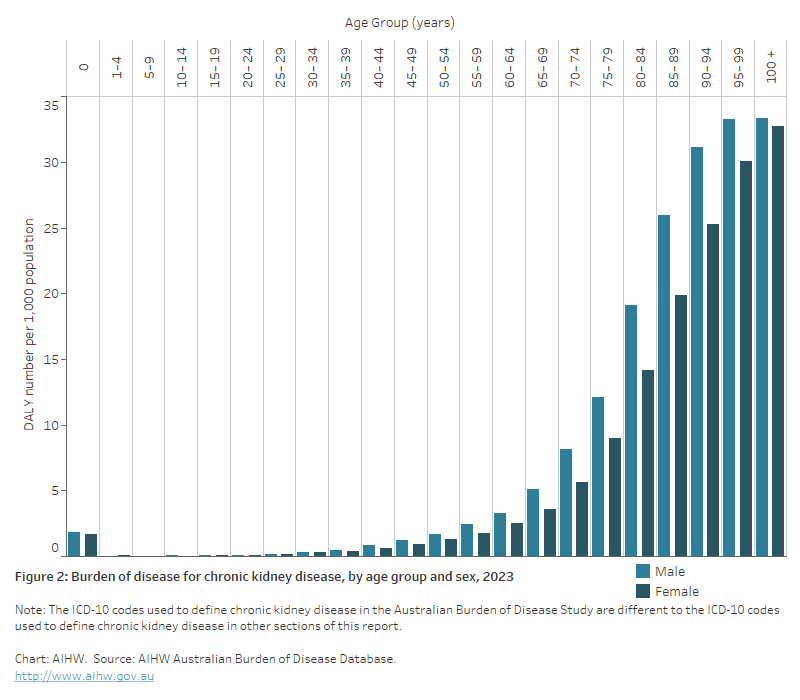
In 2023, the burden from CKD was:
- low until age 50 and increased with age (Figure 2)
- 1.3 times as high for males as females, after adjusting for age (AIHW 2023).
Figure 2: Burden of disease for chronic kidney disease, by age and sex, 2023
The bar chart shows the total burden of disease (DALY) for CKD for males and females across 22 age groups, from 0 to age 100. From age 20 burden begins to increase with increasing age, peaking at age 100 and over for both males and females.
Variation between population groups
In 2018, the burden from CKD for people living in:
- the lowest socioeconomic areas was 2.2 times as high as for people living in the highest socioeconomic areas (AIHW 2021a)
- Remote and very remote areas was 3.1 times as high as for people living in Major cities.
Trends over time
- The rate of burden from CKD was similar in 2003 and 2023 – age-standardised rates of 1.7 and 1.8 DALY per 1,000 population, respectively (AIHW 2023).
- The 49% increase in DALY from CKD between 2003 and 2018 (+16,200 DALY) was estimated to be driven by population growth (29% or 9,600 DALY) and population ageing (20% or 6,500 DALY) (AIHW 2021a).
First Nations people
Burden of disease estimates for First Nations people for 2018 (AIHW 2022a,b) show that:
- CKD accounted for 2.5% (6,100 DALY) of total burden in First Nations people in 2018 (2.0% males, 3.1% females)
- 73% of the burden from CKD among First Nations people was fatal, and 27% was non-fatal
- the burden from CKD was greater in females (58%, 3,500 DALY) than in males (42%, 2,600 DALY)
- the burden from CKD rose rapidly in First Nations people from age 40–44, peaking at ages 50–54. Overall, over 80% of the burden from CKD (4,900 DALY) occurred in people aged 40–74
- the rate of burden from CKD was 7.8 times as high for First Nations people as for non-Indigenous Australians
- CKD was responsible for 4.0% of the total male health gap and 6.5% of the total female health gap between First Nations and non-Indigenous Australians.
Contribution of risk factors
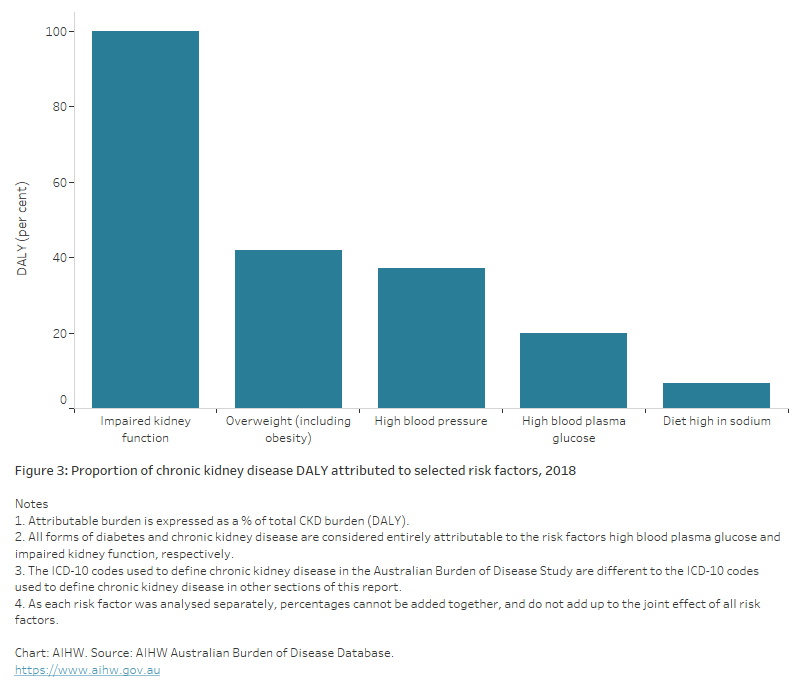
A portion of burden of disease is preventable, being due to modifiable health risk factors. The Australian Burden of Disease Study 2018 estimated the disease burden that can be attributed to these modifiable risk factors (AIHW 2021b).
This study provides estimates for burden due to impaired kidney function as a risk factor for other diseases, including coronary heart disease, dementia, stroke, gout and peripheral vascular disease. In 2018, 1.9% of the total disease burden in Australia was due to impaired kidney function (including CKD). Note that the study considers that impaired kidney function was responsible for the entire burden of CKD.
Of the total burden of CKD in Australia in 2018, 100% was attributable to all risk factors combined of those estimated in the study, including impaired kidney function.
The leading risk factors contributing to the total CKD burden in 2018 include impaired kidney function (100% male and female), overweight/obesity (43% male, 40% female), high blood pressure (38% male, 36% female), high blood plasma glucose (20% male and female), and a diet high in sodium (8% male, 5% female) (Figure 3).
Note that as each risk factor was analysed separately, percentages cannot be added together, and do not add up to the joint effect of all risk factors.
Figure 3: Proportion of chronic kidney disease DALY attributed to selected risk factors, 2018
The bar chart shows the proportion of CKD attributable to the following risk factors – impaired kidney function (100%), overweight (including obesity) (42%), high blood pressure (37%), high blood plasma glucose (19.8%) and diet high in sodium (6.6%).
AIHW (Australian Institute of Health and Welfare) (2021a) Australian Burden of Disease Study 2018: interactive data on disease burden, AIHW, Australian Government, accessed 1 February 2022.
AIHW (2021b) Australian Burden of Disease Study 2018: interactive data on risk factor burden. AIHW, Australian Government, accessed 1 February 2022.
AIHW (2022a) Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018, AIHW, Australian Government, accessed 10 March 2022.
AIHW (2022b) Australian Burden of Disease Study 2018: interactive data on disease burden among Aboriginal and Torres Strait Islander people, AIHW, Australian Government, accessed 10 March 2022.
AIHW (2023) Australian Burden of Disease Study 2023, AIHW, Australian Government, accessed 14 December 2023.


