Impact of COVID-19
The onset of the COVID-19 pandemic has had an impact on Australia’s population and health care system in multiple ways, including on economic expenditure, mortality, disability, health workforce and disease surveillance. The next web page explores the impact of COVID-19 in Australia for people living with chronic kidney disease (CKD).
Data available on CKD across the COVID period are limited by the availability of data on the continuing pandemic period, as well as the lack of longer term data.
There will likely be long-term impacts of the COVID-19 pandemic on people with CKD, even on those who do not become infected with COVID-19, due to delays in care for chronic conditions such as CKD, diabetes and cardiovascular disease (Yende and Parikh, 2021).
Kidney transplants in Australia
Organ donation numbers and transplants have declined as a result of the COVID-19 pandemic (OTA 2021). In response to COVID-19, adult kidney transplant programs were suspended from 24 March 2020 to mid-May 2020.
Pauses in transplant surgery particularly affected those with CKD, as more than half of transplanted organs are kidneys. In 2020, there was an 18% drop in the number of kidney transplants from deceased donors compared with 2019 (704 and 857 transplants, respectively). 2021 saw a decrease of 6.8% compared with 2020 (656 transplants) (OTA 2020, 2021).
Donations from living donors are classified as elective surgery; therefore, pauses in elective surgery affected the number of transplants from living donors. There was a 24% drop in living kidney donors in 2020; in 2021, the number of living kidney donors rose by 12% compared with 2020 (202 and 182 donors) (OTA 2021).
Chronic kidney disease hospitalisations
In 2020–21, there were over 4,700 hospitalisations involving a diagnosis of COVID-19 in Australia. Of these, 394 (8.4%) had CKD recorded on their hospital admission; 64 (16%) of these required a stay in the intensive care unit, 48 (12%) required continuous ventilatory support and 113 (29%) died in hospital, the third-highest death rate for comorbid conditions after chronic obstructive pulmonary disease and dementia. This includes type 2 diabetes (19%, 188 deaths) and cardiovascular disease (20%, 189 deaths), which are often comorbid with CKD. The death rate for people with CKD and COVID-19 was also higher than for people with multiple comorbid conditions who were hospitalised with COVID-19 (26%) and people with no comorbid conditions (4.7%) (AIHW 2022).
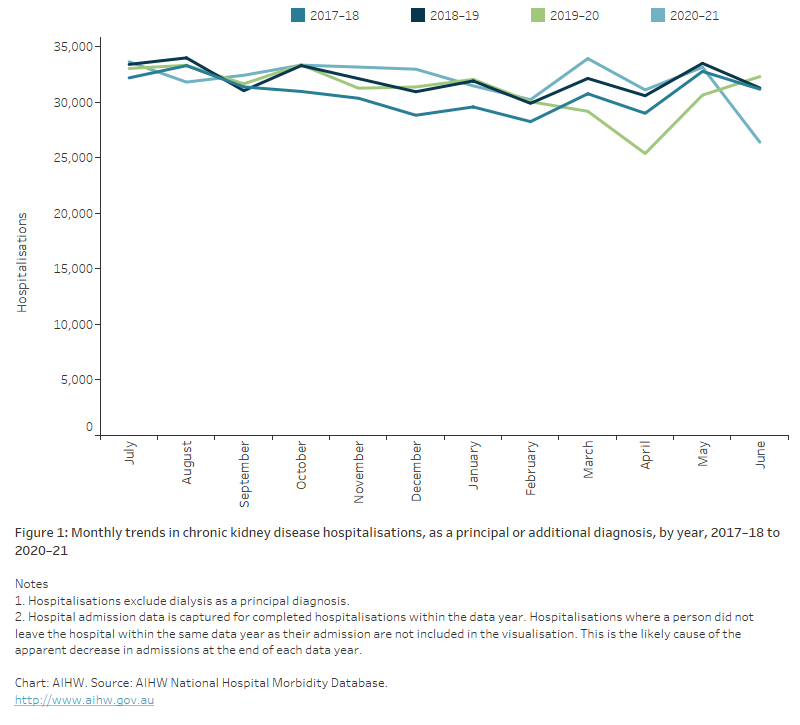
Hospital admissions for people with CKD fell sharply between March and April 2020, when lockdown measures were introduced nationwide by the Australian Government. In April 2020, CKD hospitalisations declined by 16% among males and by 18% among females, compared with figures for April 2019 (Figure 1(b)).
Figure 1 and 1(b): Monthly trends in chronic kidney disease hospitalisations, as a principal or additional diagnosis
Figure 1: The line chart shows the number of CKD hospitalisation admissions as a principal or additional diagnosis by month, for the years 2017-18, 2018-19 and 2019-20 and 2020–21. Between March and April in 2019-20, there was a large drop in the number of CKD hospitalisations not seen to the same extent in the previous 2 years, that coincided with the onset of restrictions brought in to address the COVID-19 pandemic. The number of hospital admissions for CKD in 2020–21 were comparable to years prior to 2019–20.
Figure 1b: The line chart shows the per cent change in the number of hospital admissions for CKD from January 2019 to June 2020 for males, females and persons. Compared to the previous year, hospital admissions decreased by 17% in April 2020. This affect was greater for females (declining 18%) than males (declining by 16%).
Chronic kidney disease emergency department presentations
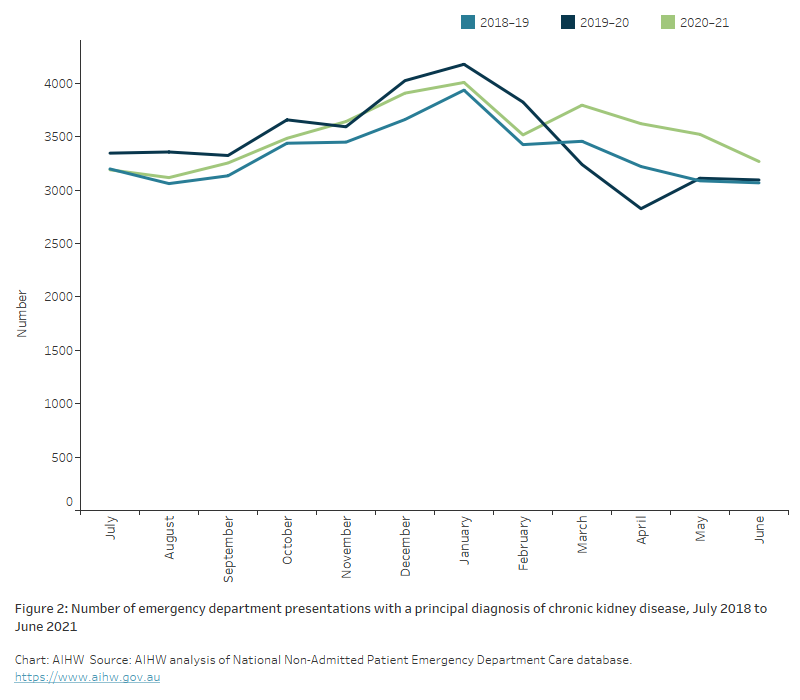
From July 2018 to June 2021, the average number of CKD-related ED presentations each month was around 3,400. The number of presentations ranged between 2,800 (April 2020) and 4,200 (January 2020) during this period.
Between January 2020 and April 2020, the rate of CKD-related ED presentations fell by about 32% (16 to 11 presentations per 100,000 population). This decline coincides with the implementation of COVID-19 restrictions in early 2020. The rate of ED presentations gradually increased between April 2020 and January 2021 (Figure 2).
Figure 2: Number of emergency department presentations with a principal diagnosis of chronic kidney disease, July 2018 to June 2021
The line chart shows the number of emergency department (ED) presentations with CKD as a principal diagnosis, by month, for the years 2018-19, 2019-20 and 2020-21. Between January and April 2019-20, there was a large drop in the number of ED presentations (from 4,200 to 2,800 presentations per month) which coincided with the implementation of restrictions associated with the COVID-19 pandemic. ED presentations gradually increased between July 2020 and December 2020.
Acute kidney injury hospitalisation in Australia
International data show that COVID-19 causes acute kidney injury (AKI) in some patients. In patients hospitalised with COVID-19, rates of AKI between 6% and 28% have been reported, increasing to around 50% in patients admitted to intensive care (Huang et al 2021; Nadim et al. 2020; Silver et al 2020). Additional research suggests that cases of AKI in COVID-19 patients may be much higher than this, if an extended definition of AKI is used to capture cases where the disease occurs before hospitalisation, or early in a hospital admission (Wainstein et al. 2022).
A meta-analysis of international data published up to October 2020 showed that 19% of AKI patients with COVID-19 who were in an intensive care unit started kidney replacement therapy (Silver et al. 2020).
Early reporting suggests that 6 months post-acute COVID-19 infection, around 35% of patients have an estimated glomerular filtration rate (eGFR) of <90 mL/min/1.73m2, including 13% who did not have AKI and had normal eGFR on discharge (Huang et al. 2021). The long-terms impacts of COVID-19 and its association with a decline in eGFR are not well understood; however, early evidence suggests that people who experienced COVID-19-associated AKI are at increased risk of developing CKD – with the severity of AKI associated with larger declines in eGFR 12 months post-acute COVID-19 infection (Gu et al. 2022; Hultström et al. 2021).
AIHW (2022) Admitted patient care 2020–21 separations with a COVID-19 diagnosis, AIHW, Australian Government, accessed 6 June 2022.
Gu X, Huang L, Cui D, Wang Y, Wang Y, Xu J et al. (2022) Association of acute kidney injury with 1-year outcome of kidney function in hospital survivors with COVID-19: a cohort study, eBioMedicine, 76:193817, doi:10.1016/j.ebiom.2022.103817.
Huang C, Huang L, Wang Y, Ren L, Gu X, Kang L et al. (2021) 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study, The Lancet, 397:220–232, doi:10.1016/S0140-6736(20)32656-8.
Hultström M, Lipcsey M, Wallin E, Larsson I, Larsson A and Fritihof R (2021) Severe acute kidney injury associated with progression of chronic kidney disease after critical COVID-19, Critical Care, 25:37, doi:10.1186/s13054-021-03461-4.
Nadim MK, Forni LG, Mehta RL, Connor Jr MJ, Liu KD, Ostermann M et al. (2020) Publisher correction: COVID-19-associated acute kidney injury: consensus report of the 25th Acute Disease Quality Initiative (ADQI) Workgroup, Nature Reviews Nephrology 16,765 doi:10.1038/s41581-020-00372-5.
OTA (Organ and Tissue Authority) (2020) 2020 Australian donation and transplantation activity report, OTA, Australian Government, accessed 16 March 2022.
OTA (2021) 2021 Australian donation and transplantation activity report, OTA, Australian Government, accessed 16 March 2022.
Silver SA, Beaubien-Souligny W, Shah PS, Harel S, Blum D, Kishibe T et al. (2020) &The prevalence of acute kidney injury in patients hospitalized with COVID-19 infection: a systematic review and meta-analysis, Kidney Medicine, 3(1) 83–98.e1, doi:10.1016/j.xkme.2020.11.008.
Wainstein M, MacDonald S, Fryer D, Young K, Balan V, Begum H et al. (2022) Use of an extended KDIGO definition to diagnose acute kidney injury in patients with COVID-19: a multinational study using the ISARIC-WHO clinical characterisation protocol, PLOS Medicine, 19(4):e1003969, doi:10.1371/journal.pmed.1003969.
Yende S and Parikh CR (2021) Long COVID and kidney disease, Nature Reviews Nephrology, doi:10.1038/s41581-021-00487-3.


