Hospital care for First Nations people with dementia
In 2021–22, there were 382 hospitalisations due to dementia (where dementia was the principal diagnosis or the main reason for the hospital admission) where the patient identified as a First Nations person.
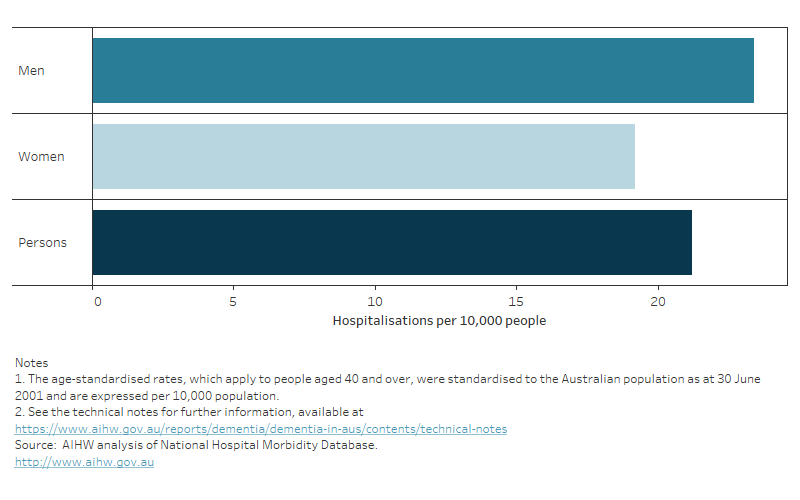
First Nations men were more likely to be hospitalised due to dementia (23 hospitalisations per 10,000 First Nations men) than First Nations women (19 hospitalisations per 10,000 First Nations women) (Figure 12.9).
Refer to Hospital care for more information on overall hospitalisations for dementia in Australia and see the Technical notes for further information on hospitals data. For information about the quality of First Nations identification in hospitals data, see Indigenous identification in hospital separations data: quality report.
Figure 12.9: Hospitalisations for First Nations people due to dementia in 2021–22: age-standardised rate,
by sex
A bar graph showing the age standardised rate of hospitalisations due to dementia for male and female First Nations people in 2021–22.
The average length of stay among First Nations people for hospitalisations due to dementia was 15.5 days, slightly longer than the average length of stay for all hospitalisations due to dementia in 2021–22 for non-Indigenous Australians (14.8 days).
There are many reasons why First Nations people may not want to use hospital services, such as: competing family and cultural obligations; distrust in the health system due to negative past and present experiences; a lack of culturally safe care options; communication barriers with medical staff, including barriers for First Nations people for whom English is a second language; limited access to health services in regional and remote locations requiring patients to receive care away from their community; high travel and other out-of-pocket costs, especially for people living in regional and remote locations (AHMAC 2017; Shaw 2016).
How did hospitalisations due to dementia end for First Nations people?
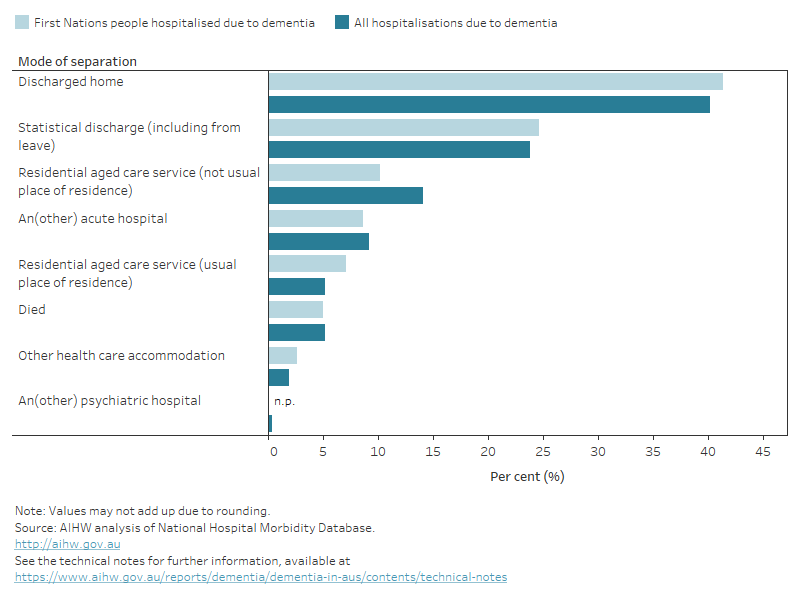
In 2021–22 about 40% of hospitalisations of First Nations people due to dementia ended with the patient being discharged home, 7% were discharged to residential aged care which was their usual place of residence and 10% discharged to residential aged care that was not their usual place of residence (Figure 12.10). This trend is similar across all hospitalisations due to dementia.
Figure 12.10 First Nations hospitalisations due to dementia in 2021–22: percentage by mode of separation
Figure shows a bar chart comparing the method of discharge between First Nations hospitalisations due to dementia with all hospitalisations due to dementia. First Nations hospitalisations due to dementia and all hospitalisations due to dementia follow similar trends with hospitalisation most likely to end due to being discharged home (41%), then statistical discharge (25%) entering residential aged care, not the usual place of residence (10%).
When First Nations people were hospitalised due to dementia, what other conditions did they have?
When First Nations people were admitted to hospital due to dementia, the most common diagnoses (additional and supplementary diagnoses), other than dementia were:
- hypertension
- ischaemic heart disease (also known as coronary heart disease)
- type 2 diabetes without complications
- constipation
- arthritis and osteoarthritis
Three of these diagnoses are closely related to the modifiable risk factors for dementia, hypertension, ischaemic heart disease and type 2 diabetes. For further information on the top 10 other diagnoses, see table S12.20.
How did hospitalisations due to dementia for First Nations people vary by geographic area?
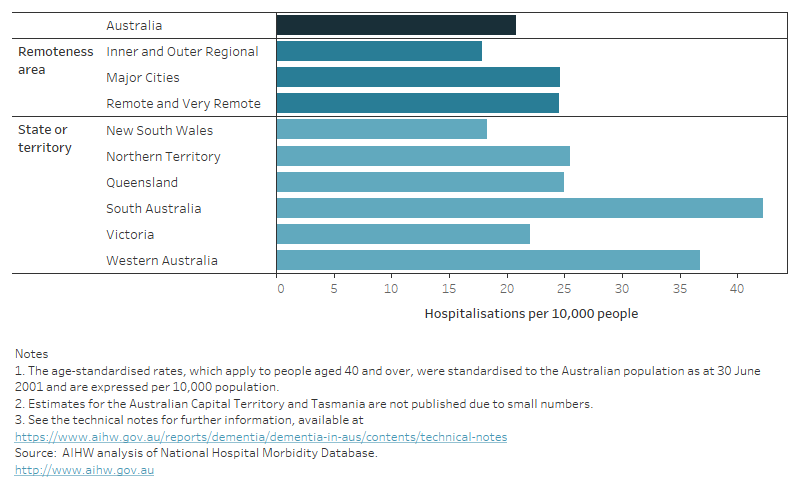
Given the small number of hospitalisations due to dementia for First Nations people in a given year, the rates of hospitalisations due to dementia presented in this analysis were aggregated over a 3-year period (2019–20, 2020–21 and 2021–22).
After adjusting for population differences, between 2019–20 and 2021–22, the age-standardised rate of hospitalisations due to dementia for First Nations people aged 40 years and over, was:
- highest in South Australia (42 hospitalisations per 10,000 First Nations people) followed by Western Australia (37 hospitalisations per 10,000) and was lowest in New South Wales (18 hospitalisations per 10,000)
- highest in Remote and Very Remote areas and Major Cities (25 hospitalisations per 10,000 First Nations people) and was lowest in Inner and Outer Regional areas (18 hospitalisations per 10,000) (Figure 12.11).
Figure 12.11: Hospitalisations for First Nations people due to dementia between 2019–20 and 2021–22: age-standardised rate, by state and territory and remoteness area
A bar graph showing the age standardised rate of hospitalisations due to dementia among First Nations people between 2019-20 and 2021–22 by remoteness area and state or territory.
First Nations hospitalisations with dementia
Previous sections have presented hospitalisations due to dementia (that is, when dementia was recorded as the principal diagnosis), but understanding hospitalisations with dementia (that is all hospitalisations with a record of dementia, whether as the principal and/or an additional diagnosis and/or a supplementary diagnosis) provides important insights on the wide-ranging conditions that can lead people living with dementia to use hospital services.
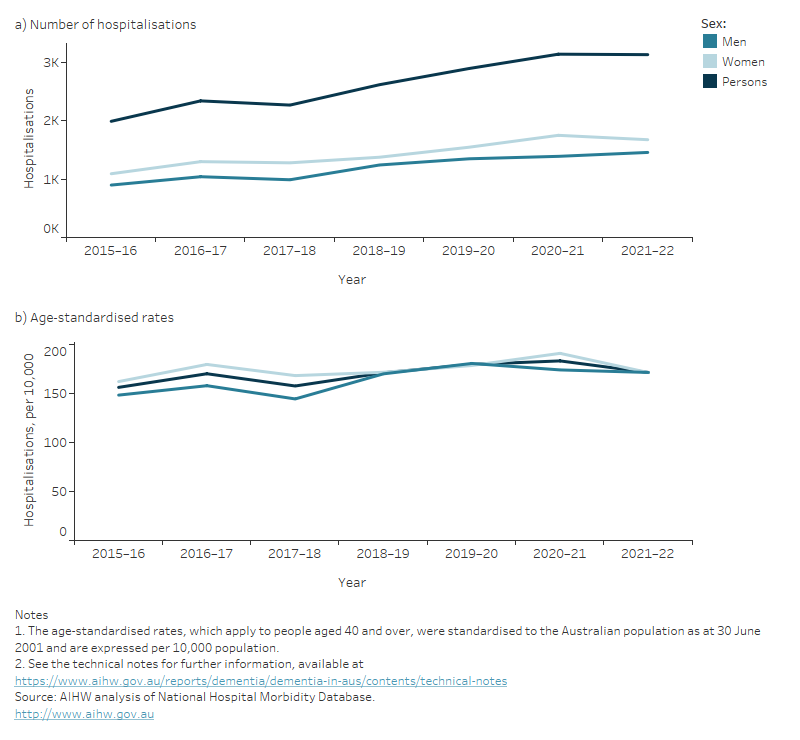
There were just over 3,100 First Nations people hospitalised in 2021–22 with dementia, a 57% rise from 2015–16. The age-standardised rate also rose during this time from about 155 to 170 per 10,000 First Nations people. This rise shows that this is a genuine increase in hospitalisations and not simply due to Australia having a growing and ageing population.
Figure 12.12 First Nations hospitalisations with dementia between 2015–16 and 2021–22 by sex:
(a) number and (b) age-standardised rate
Figure shows two line graphs. The first showing the number of hospitalisations of First Nations people with dementia over time, increasing steadily from 2015–16 (1,990 hospitalisations) to 2021–22 (3,132 hospitalisations). The second graph shows the age-standardised rates of hospitalisations of First Nations people with dementia over time slightly increasing over time from 156 hospitalisations per 10,000 First Nations people to 171 hospitalisations per 10,000 First Nations people.
What were the most common principal diagnoses for First Nations people when dementia was an additional diagnosis?
In 2021–22 there were about 3,100 hospitalisations of First Nations people with dementia.
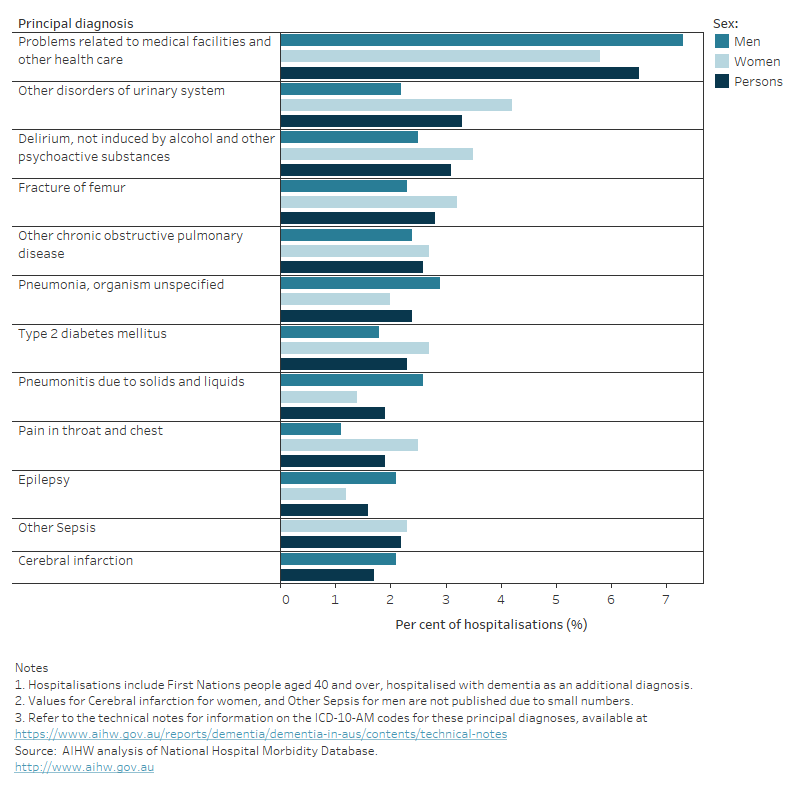
The most common principal diagnoses among hospitalisations for First Nations people aged 40 years and over, where dementia was an additional diagnosis, were:
- Problems related to medical facilities and other health care (6.5%)
- Other disorders of urinary system (3.3%)
- Delirium, not induced by alcohol and other psychoactive substances (3.1%)
Other common principal diagnoses recorded for these hospitalisations included pneumonia, sepsis, femur fractures and a number of chronic conditions such as chronic obstructive pulmonary disease, cardiovascular diseases, and diabetes (Figure 12.13).
Figure 12.13: Common principal diagnoses for hospitalisations of First Nations people where dementia was an additional diagnosis in 2021–22: percent of hospitalisations, by sex
A bar chart showing the age standardised rates of hospitalisations by common principal diagnoses and sex for First Nations people where dementia was an additional diagnosis in 2021–22.
AIHW (Australian Institute of Health and Welfare) (2023) Coronary heart disease, AIHW, Australian Government, accessed 25 January 2023.
Australian Health Ministers’ Advisory Council (2017) Aboriginal and Torres Strait Islander Health Performance Framework 2017 report, Australian Health Ministers’ Advisory Council, Australian Government, accessed 17 August 2022.
Shaw C (2016) An evidence‑based approach to reducing discharge against medical advice amongst Aboriginal and Torres Strait Islander patients, The Deeble Institute for Health Policy Research, Australian Healthcare and Hospitals Association, accessed 17 August 2022.


