Antipsychotics and other medications dispensed to people with dementia
What other medications were dispensed to people who were dispensed scripts for dementia-specific medications?
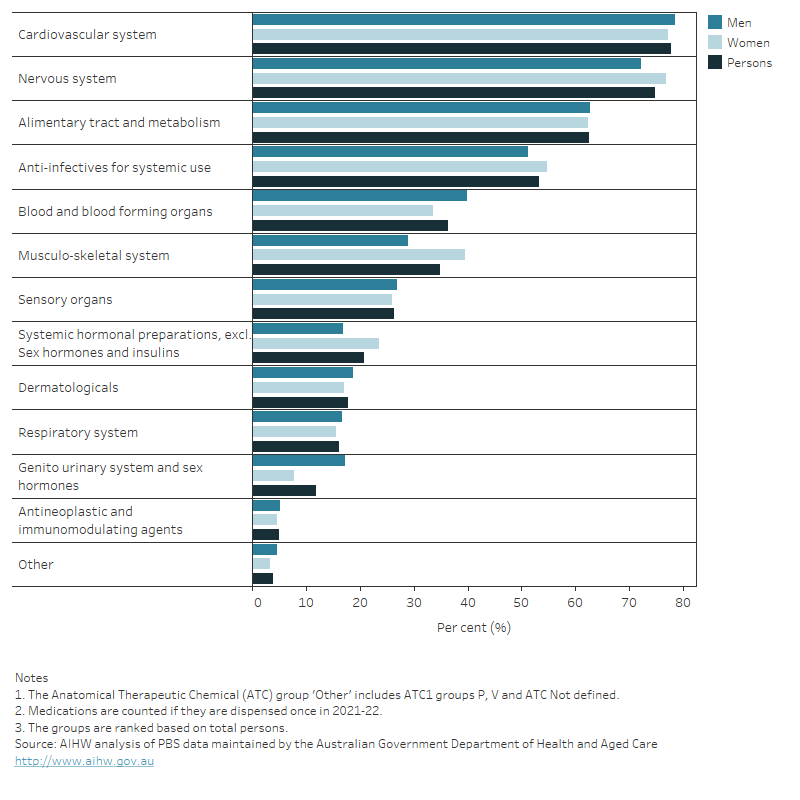
As people with dementia often have other co-existing conditions, they are likely to be prescribed a range of other medicines. Figure 8.6 shows the types of other medications dispensed to people who were dispensed dementia-specific medications in 2021–22, grouped at the highest level (Anatomical Therapeutic Chemical classification 1 (ATC1)). Refer to the Technical notes for further detail on the Anatomical Therapeutic Chemical classification and the grouping of medications by level.
The most common group of other medications dispensed was for cardiovascular system medications (dispensed at least once to 79% of men and 77% of women who were dispensed dementia-specific medication). This was followed by nervous system medications (72% of men and 77% of women) and, alimentary tract and metabolism medications (63% of men and 62% of women).
Figure 8.6: People who were dispensed scripts for dementia-specific medications in 2021–22: percentage who were dispensed scripts for other medications at least once, by sex and medications’ Anatomical Therapeutic Chemical (ATC) group
Figure 8.6 is a bar graph showing the percentage of people dispensed dementia-specific medications who were also dispensed other medications in 2021-22, by medication type and sex. The medications are grouped at the highest Anatomical Therapeutic Chemical classification level. Around three-quarters of men and women who were dispensed scripts for dementia-specific medications were also dispensed medications for the cardiovascular system, and nervous system. Men were less likely than women to be dispensed nervous system medications, anti-infectives for systemic use, musculoskeletal system medications, and systemic hormonal preparations. However, men were more likely than women to be dispensed medications for the cardiovascular system, alimentary tract and metabolic, blood and blood forming organs, sensory organs, dermatologicals, respiratory system, genitourinary system and sex hormones and for antineoplastic and immunomodulating agents.
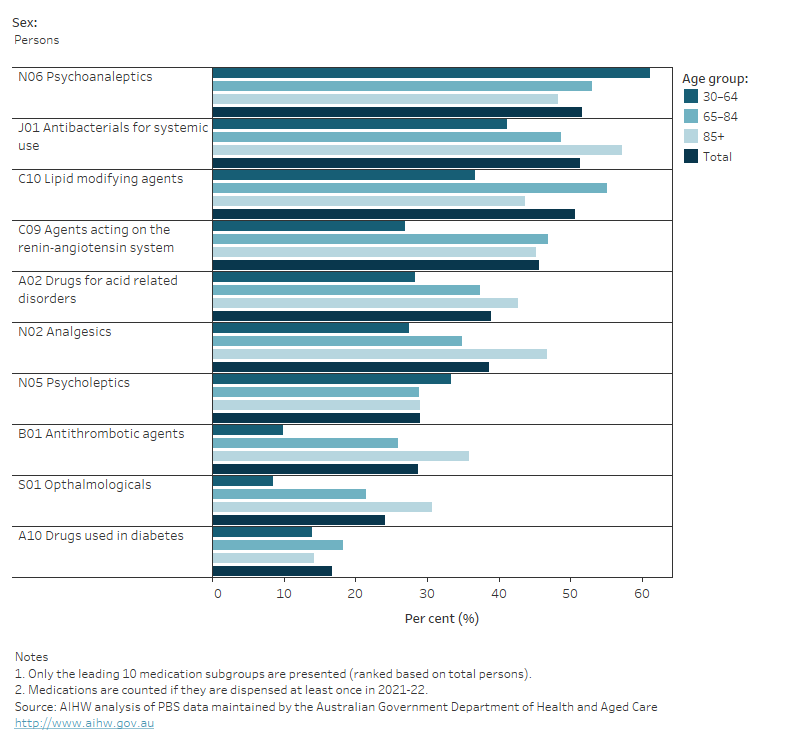
The most common subgroup of other medications was psychoanaleptics, dispensed at least once to 52% of people who were dispensed scripts for dementia-specific medications (Figure 8.7). These medications are used to treat depression and other neurological and mental disorders. The next most common subgroups were:
- antibacterials for systemic use (51%; used to treat a range of bacterial infections)
- lipid modifying agents (51%; used to lower high levels of fats in the blood, such as cholesterol)
- agents acting on the renin-angiotensin system (46%; used for hypertension)
- drugs for acid related disorders (39%; used to neutralise stomach acidity and relieve heartburn, indigestion or stomach upset).
There were notable differences by sex and age in the most common medications dispensed at least once to people who were dispensed scripts for dementia-specific medication.
Psychoanaleptics were dispensed to a larger proportion of those with younger onset dementia (aged under 65) compared with people aged 85 and over (61% compared with 48%). However, most other medications were dispensed to a greater proportion of those aged 85 and over, with the greatest differences seen with antithrombotic agents (36% compared with 9.8% of people aged 30–64) and opthalmologicals (31% compared with 8.5%).
Figure 8.7: People who were dispensed scripts for dementia-specific medications in 2021–22: percentage who were dispensed scripts for other medications, by Anatomical Therapeutic Chemical (ATC) sub-group, age and sex
Figure 8.7 is a bar graph showing the percentage of people dispensed dementia-specific medications who were also dispensed other medications in 2021-22, by medication type, age and sex. The medications are grouped at the second highest Anatomical Therapeutic Chemical classification level. Over half (52%) were dispensed scripts for psychoanaleptics, which are used for depression and other neurological and mental disorders. Half of people were dispensed scripts for antibacterials for systemic use, which are used to treat a range of bacterial infections. Men were more likely than women to be dispensed scripts for lipid modifying agents, agents acting on the renin-angiotensin system, psycholeptics, antithrombotic agents and drugs used in diabetes. However, women were more likely than men to be dispensed scripts for psychoanaleptics, antibacterials, drugs for acid related disorders, analgesics, and opthalmologicals. While the majority of medications were dispensed to greater proportions of older people who were dispensed dementia-specific medications, psychoanaleptics were dispensed to a larger proportion of those with younger onset dementia (aged under 65) compared with people aged 85 and over.
Dispensing of antipsychotics to people with dementia
People with dementia may experience changed behaviours, such as aggression, agitation and delusions, commonly known as behavioural and psychological symptoms of dementia (BPSD). To manage these symptoms, non-pharmacological interventions are recommended, but medical professionals may prescribe antipsychotic medicines to people with dementia with BPSD as a last resort. However, inappropriate prescribing of antipsychotic medicines is a major problem among people living in residential aged care and a key issue raised in the Royal Commission into Aged Care Quality and Safety (Royal Commission 2021) (see Box 8.2 for more information). Risperidone is the only antipsychotic that is currently listed on the PBS for BPSD.
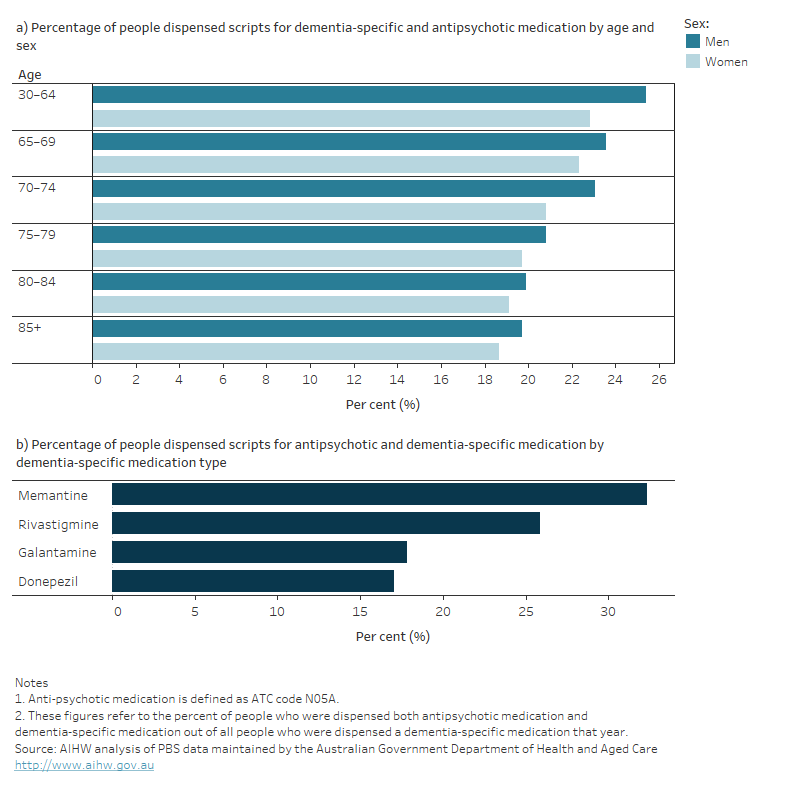
In 2021–22, antipsychotic medications (which are part of the psycholeptics group) were dispensed to about one-fifth (20%) of the 68,700 people who had scripts dispensed for dementia-specific medication (Figure 8.8). This includes all antipsychotic medications and not just Risperidone.
Around 55% or 7,600 of the people dispensed antipsychotic medications were women. The proportion of people within each age group who were prescribed scripts for antipsychotics decreased slightly with increasing age.
In each age group, men were relatively more likely to be dispensed scripts for antipsychotics at least once than women (Figure 8.8a). However, as more women have dementia, overall more women were dispensed antipsychotic medication than men.
Antipsychotics were more likely to be dispensed to people who were also taking Memantine (32% of people on Memantine) compared with other dementia-specific medicines (26% of people on Rivastigmine, 18% of people on Galantamine and 17% of people on Donepezil) (Figure 8.8b). This probably reflects the fact that Memantine is prescribed for moderately severe Alzheimer’s disease, whereas the other 3 dementia-specific medications are prescribed for mild to moderately severe Alzheimer’s disease.
Although Risperidone is the only antipsychotic listed on the PBS for BPSD, scripts for other antipsychotic medications were dispensed to people with dementia. Around 36% of all antipsychotic scripts that were dispensed to people also on dementia-specific medication were for Risperidone, followed by Quetiapine (30%) and Olanzapine (25%) (Table S8.11).
Figure 8.8: People who were dispensed dementia-specific medications in 2021–22: percentage who were dispensed antipsychotic medication (a) by age and sex and (b) by dementia-specific medication
Figure 8.8 shows two bar graphs depicting breakdowns of the percentage of people who were dispensed prescriptions for dementia-specific medications and also dispensed prescriptions for antipsychotic medications at least once in 2021-22. The first graph shows the percentage by age and sex and the second graph shows the percentage by the type of dementia-specific medication they were dispensed. Overall, around one-fifth of people who were dispensed prescriptions for dementia-specific medications were also dispensed antipsychotic medications. The proportion within each age group who were prescribed scripts for antipsychotics decreased slightly with age. Men were relatively more likely to be dispensed scripts for antipsychotics than women in each age group. Antipsychotics were more likely to be dispensed to people who were also taking Memantine, which is the only dementia-specific medication prescribed for moderately severe to severe Alzheimer’s disease.
Box 8.2: Antipsychotic medications for people with dementia and inappropriate prescribing of antipsychotics
Antipsychotic medicines should only be prescribed to people with dementia following the unsuccessful attempt of managing symptoms of dementia using non-pharmacological treatments, as the combined use of dementia-specific and antipsychotic medicine increases the risk of serious adverse effects, including death. This risk increases over longer periods of use (Dementia Australia 2016; Dyer et al. 2016). Risperidone, which is a type of antipsychotic medicine, is the only antipsychotic currently listed on the PBS that may be prescribed to a person with dementia who displays persistent behavioural disturbances such as psychotic symptoms, restlessness and aggression (known as either ‘changed behaviours’ or ‘behavioural and psychological symptoms of dementia’ (BPSD)). However, inappropriate prescribing of antipsychotics to people living in residential aged care (where over half of people have dementia) is a major issue in Australia.
To reduce inappropriate prescribing of antipsychotic medicines to people with dementia, changes were made to the PBS for prescribing of Risperidone for managing changed behaviours. As of January 2020, prescribers will need to request authority approval from Services Australia to prescribe ‘continuing’ PBS-subsidised Risperidone treatment (beyond 12 weeks of initial use) to people with dementia (Department of Health 2019).
Dyer SM, Laver K, Pond CD, Cumming RG, Whitehead C and Crotty M (2016) 'Clinical practice guidelines and principles of care for people with dementia in Australia', Australian Family Physician, 45(12):884-889.
Dementia Australia (2016) Drugs used to relieve behavioural and psychological symptoms of dementia, Dementia Australia, accessed 10 July 2023.
Department of Health (2019) Risperidone factsheet, PBS website, accessed 10 July 2023.
Royal Commission (Royal Commission into Aged Care Quality and Safety) (2021) Final report: Care, Dignity and Respect. Volume 1 Summary and recommendations, Royal Commission, Australian Government, accessed 10 July 2023.


