Mothers aged 35 and over and their babies
This section focuses on mothers who gave birth when they were aged 35 and over and their babies. With appropriate medical care, most older mothers have healthy pregnancies and babies. However, older mothers remain at higher risk of developing some conditions such as gestational diabetes mellitus or preeclampsia (Li et al. 2020; Marozio et al. 2017). Babies born to older mothers can have a higher risk of preterm birth, fetal distress or poor fetal growth (Cavazos-Rehg et al. 2015; Fuchs et al. 2018). In many cases, medical supervision and regular antenatal visits can safely manage or prevent these conditions (Dietl et al. 2015).
Mothers who gave birth aged 35 and over
In 2021, women who gave birth aged 35 and over accounted for 26% (81,871) of all mothers. This proportion has remained between 22% and 26% since 2011 (23% and 67,359 in 2011).
Figure 1 presents data for women who gave birth aged 35 and over, by selected maternal characteristics over an 11-year period (where available).
Figure 1: Proportion of women who gave birth aged 35 and over, by selected topic
Line graph of proportion of mothers aged 35 and over by selected topics between 2011 and 2021.
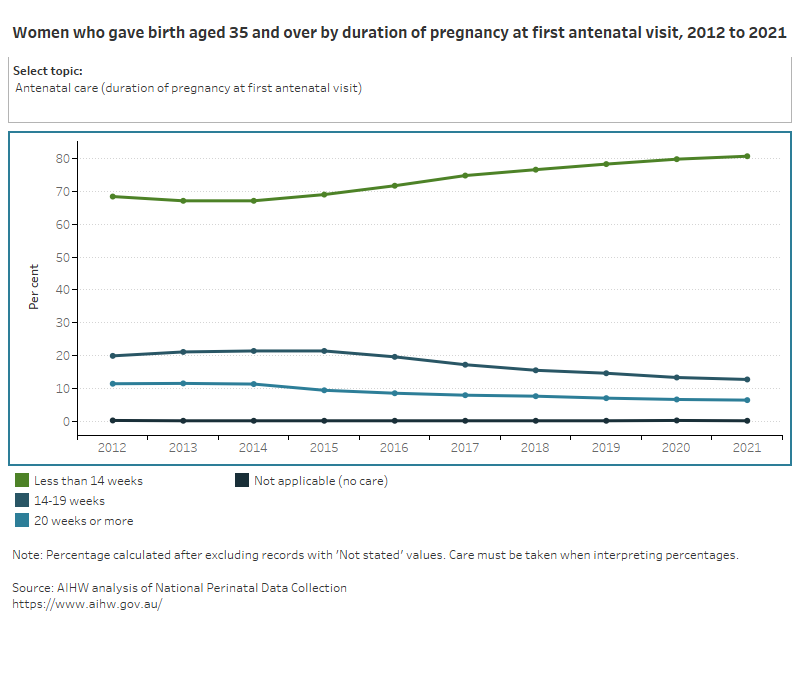
Most mothers aged 35 and over accessed antenatal care in the first trimester (81%) and the majority had 5 or more antenatal visits (96%).
Over time, the most common onset of labour type for mothers aged 35 and over has become no labour (36% in 2021, up from 30% in 2011 when spontaneous was the most common onset of labour), with a corresponding caesarean section rate of almost 1 in 2 (48% in 2021).
Mothers aged 35 and over are unlikely to smoke during pregnancy, with 5.5% reporting that they smoked at any time during pregnancy in 2021. This rate has fallen over time (8.5% in 2011).
It is important to note that mothers aged 35 and over experience differences in relation to maternal characteristics, health behaviours and outcomes – and perinatal outcomes – when compared to the overall population of Australian mothers and babies. These differences can be explored when viewing Maternal age at the chapter or topic level throughout this report.
Babies born to mothers aged 35 and over
In 2021, babies born to mothers aged 35 and over accounted for 4.5% (14,113) of all births.
Figure 2 presents data for babies born to women who gave birth aged 35 and over, by selected baby characteristics over an 11-year period (where available).
Figure 2: Proportion of liveborn babies of mothers aged 35 and over, by selected topic
Line graph of babies of mother aged 35 and over by selected topics between 2019 and 2021.
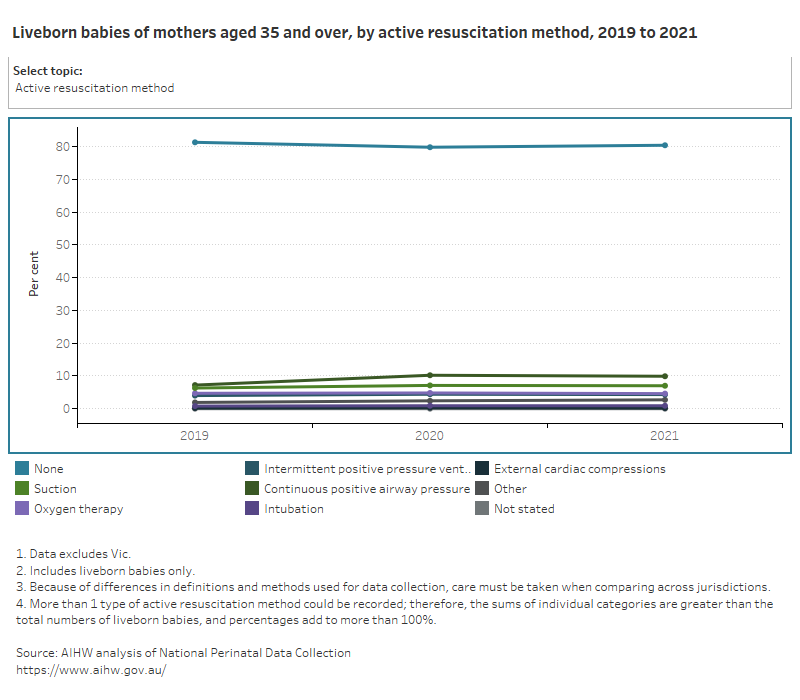
In 2021, most babies born to mothers aged 35 and over were born at term and had a normal birthweight (91% and 92%, respectively).
Over 1 in 5 babies born to mothers aged 35 and over required active resuscitation or admission to SCN/NICU (20% and 17%, respectively), and 37% had a hospital stay of 4 days or more.
References
Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Bommarito K, Madden T, Olsen MA, Subramaniam H, Peipert JF and Bierut LJ (2015) ‘Maternal age and risk of labor and delivery complications’, Maternal and Child Health Journal, 19(6):1202–1211, doi:10.1007/s10995-014-1624-7.
Dietl A, Cupisti S, Beckmann MW, Schwab M and Zollner U (2015) ‘Pregnancy and obstetrical outcomes in women over 40 years of age’, Geburtshilfe und Frauenheilkunde, 75(8):827–832, doi:10.1055/s-0035-1546109.
Fuchs F, Monet B, Ducruet T, Chaillet N and Audibert F (2018) ‘Effect of maternal age on the risk of preterm birth: a large cohort study’, PLOS One, 13(1):e0191002, doi:10.1371/journal.pone.0191002.
Li Y, Ren X, He L, Li J, Zhang S and Chen W (2020) ‘Maternal age and the risk of gestational diabetes mellitus: a systematic review and meta-analysis of over 120 million participants’, Diabetes Research and Clinical Practice, 162:108044, doi:10.1016/j.diabres.2020.108044.
Marozio L, Picardo E, Filippini C, Mainolfi E, Berchialla P, Cavallo F, Tancredi A and Benedetto C (2019) ‘Maternal age over 40 years and pregnancy outcome: a hospital-based survey’, Journal of Maternal-Fetal and Neonatal Medicine, 32(10):1602–1608, doi:10.1080/14767058.2017.1410793.


