Health status
On this page:
About the 2020–21 National Health Survey
Data for 2020–21 are based on information self-reported by the participants of the Australian Bureau of Statistics (ABS) 2020–21 National Health Survey (NHS).
Previous versions of the NHS have primarily been administered by trained ABS interviewers and were conducted face-to-face. The 2020–21 NHS was conducted during the COVID-19 pandemic. To maintain the safety of survey respondents and ABS Interviewers, the survey was collected via online, using self-completed questionnaire forms.
Non-response is usually reduced through interviewer follow-up of households who have not responded. As this was not possible during lockdown periods, there were lower response rates than previous NHS cycles, which impacted sample representativeness for some sub-populations. Additionally, the impact of COVID-19 and lockdowns might also have had direct or indirect impacts on people’s usual behaviour over the 2020–21 period. Due to these changes, comparisons to previous NHS data over time are not recommended when using the 2020–21 NHS results. For more information on the ABS NHS, refer to ABS National Health Survey: First results methodology.
This web report includes results from the 2020–21 NHS to explore ADF service and DVA client breakdowns by demographic information such as age and sex, health status and risk factors for chronic disease.
Data considerations
Data from the 2020–21 NHS presented in this chapter have been tested for statistically significant differences at the 5% level using confidence intervals, and comprehensive tables are available in Health of veterans: supplementary data tables – Table S2 and S3. For more information on the methodology used, see Technical notes.
While comparisons can be inferred from the information provided here from the 2020–21 NHS, some differences between the populations are likely to be confounded by the older age structure of the population who have ever served in the ADF, and comparisons should be used as a guide only. The results presented below have not been adjusted for age as the data could not meet requirements to do so, and readers should take this into consideration when interpreting the results presented.
Currently, women comprise around 18% of the population who have ever served in the ADF (AIHW analysis of ABS 2022a). These relatively low numbers constrain reporting on the health of women who have served, therefore this section of the report presents data for men only.
Self-assessed health status
Self-assessed health status is a commonly used measure of overall health which reflects a person’s perception of his or her own health at a given time (ABS 2018a). As a self-reported measure, it captures the combined effects of physical, social, emotional, and mental health and wellbeing.
Based on self-reported data from the 2020–21 NHS among males aged 18 years and over:
- The majority of those who had ever served in the ADF rated their health as good or better (Figure 3). Around three quarters (76%) of males who had ever served in the ADF considered themselves to be in excellent, very good or good health, while 24% of people who ever served considered their health to be fair or poor.
- Males who had ever served in the ADF were less likely to rate their health as excellent or very good than those who had never served (45% compared with 57%, respectively) (AIHW analysis of ABS 2022a).
Figure 3: Self-assessed health status by ADF service status, males aged 18 years and over, 2020–21
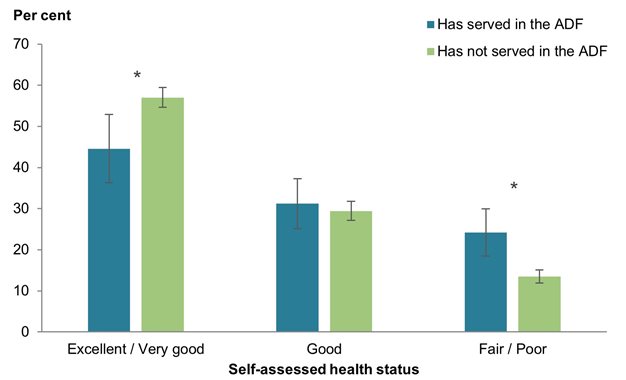
* A statistically significant difference between males who have served in the ADF and males who have never served in the ADF, calculated using the confidence interval of the difference between the two proportions.
Note: the thin vertical lines superimposed over the top end of each bar are 95% confidence intervals.
Chart: AIHW.
Source: AIHW analysis of ABS 2022a. See Health of veterans: supplementary data tables – Table S2.
Of males aged 18 years and over who had ever served and who self-reported being a DVA client in the 2020–21 NHS:
- #47%1 of males considered their health as being excellent or very good, which was similar to those who were non-DVA clients (#43%1) (Figure 4).
- Regardless of DVA client status, around a quarter of males who had ever served in the ADF rated their health as fair or poor (#25%1 for DVA clients and 24% for non-DVA clients, respectively) (AIHW analysis of ABS 2022a).
Figure 4: Self-assessed health status by DVA client status, males aged 18 years and over, 2020–21
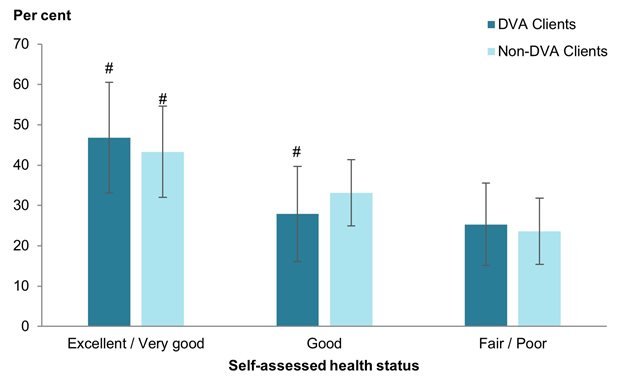
# Proportion has a high margin of error (MoE) and should be used with caution.
Note: the thin vertical lines superimposed over the top end of each bar are 95% confidence intervals.
Chart: AIHW.
Source: AIHW analysis of ABS 2022a. See Health of veterans: supplementary data tables – Table S2.
Health conditions
Long-term health conditions, both physical and mental, have a significant impact on health. In particular, mental health conditions, including depression, post-traumatic stress disorder (PTSD) and alcohol dependence disorder, have been identified as an issue of concern for Australia’s veterans (DVA 2015). Those who have served in the ADF also experience these and other conditions to varying degrees.
Based on self-reported data from the 2020–21 NHS, males aged 18 years and over who had ever served in the ADF had a higher prevalence of several long-term health conditions compared with those who had never served. This includes higher rates of:
- Arthritis (33% compared with 12%)
- Back problems (31% compared with 19%)
- Heart, stroke and vascular disease (15% compared with 5.9%)
- Diabetes (14% compared with 6.9%)
- Cancer (6.7% compared with 2.6%)
- Chronic obstructive pulmonary disease (COPD2) (3.6% compared with 1.0%) (AIHW analysis of ABS 2022a).
Among those who had ever served, the prevalence of long-term health conditions was similar regardless of DVA client status (AIHW analysis of ABS 2022a).
Results for health conditions have been tested for statistically significant differences (see Technical notes). Detailed results for all self-reported long-term conditions by ADF service status and DVA client status can be found in Health of veterans: supplementary data tables – Table S3.
Mental and behavioural conditions
Addressing the development and management of mental disorders such as depression, PTSD, other anxiety disorders and alcohol dependence for the veteran community has been identified as a priority for the Australian Government (DVA 2015). International studies suggest an increased prevalence of dementia among veterans compared with the general population; veterans have an increased prevalence of risk factors for dementia: including traumatic brain injury sustained through active duty, PTSD, and major depressive disorder (Rafferty 2018; Singer 2015).
The disclosure of mental health conditions during service can be associated with stigma and fear of repercussions on career (Joint Standing Committee on Foreign Affairs, Defence and Trade 2019). Mental health stigma is also associated with barriers to seeking help following transition to civilian life. It may be the case that non-DVA clients (or veterans who chose not to engage with DVA) are more reluctant or less likely to disclose poor mental health rather than those who are DVA clients or who have sought support from DVA. This limitation may apply to the data presented in this report.
Based on self-reported data from the 2020–21 NHS, of males aged 18 years and over:
- Over a quarter (27%) of those who had ever served in the ADF had a mental or behavioural condition, compared with less than 1 in 5 (17%) who had never served.
- 12% of males who ever served in the ADF reported having had depression or feeling depressed, which was similar to those who had never served (9.4%) (Figure 5).
- Those who had ever served in the ADF were around twice as likely to report having an anxiety-related disorder as those who had never served (21% compared with 11%) (AIHW analysis of ABS 2022a).
Figure 5: Prevalence of depression and anxiety-related conditions by ADF service status, males aged 18 years and over, 2020–21
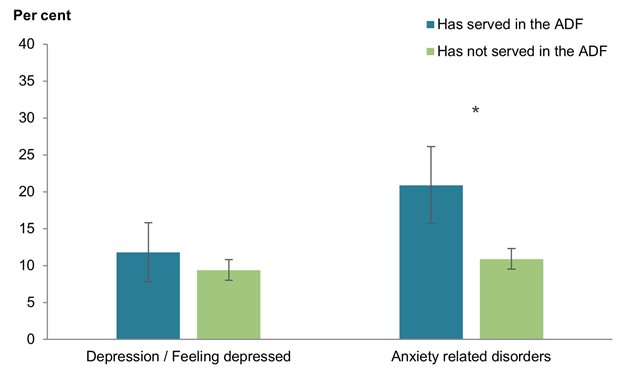
* A statistically significant difference between males who have served in the ADF and males who have never served in the ADF, calculated using the confidence interval of the difference between the two proportions.
Note: the thin vertical lines superimposed over the top end of each bar are 95% confidence intervals.
Chart: AIHW.
Source: AIHW analysis of ABS 2022a. See Health of veterans: supplementary data tables – Table S3.
Of males aged 18 years and over who had ever served and who self-reported being a DVA client in the 2020–21 NHS:
- #36%1 reported having mental and behavioural conditions, which was higher than those who were non-DVA clients (22%).
- A similar proportion of DVA clients reported depression or feeling depressed (14%) compared with non-DVA clients (11%; Figure 6).
- DVA clients were more than twice as likely to report having anxiety related disorders as non-DVA clients (#32%1 compared with 15%, respectively) (AIHW analysis of ABS 2022a).
Figure 6: Prevalence of depression and anxiety-related conditions by DVA client status, males aged 18 years and over, 2020–21
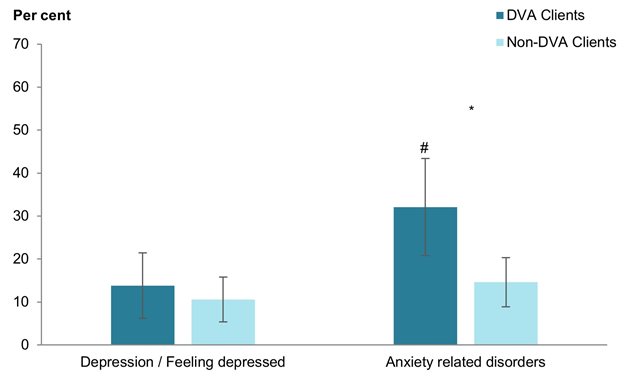
* A statistically significant difference between males who have served in the ADF and were DVA clients, and males who have ever served in the ADF and were not DVA clients, calculated using the confidence interval of the difference between the two proportions.
# Proportion has a high margin of error MoE) and should be used with caution.
Note: the thin vertical lines superimposed over the top end of each bar are 95% confidence intervals.
Chart: AIHW.
Source: AIHW analysis of ABS 2022a. See Health of veterans: supplementary data tables – Table S3.
One indication of the mental health and wellbeing of a population is provided by measuring levels of psychological distress using the Kessler Psychological Distress Scale (K10). The K10 questionnaire was developed to yield a global measure of psychosocial distress, based on questions about people’s level of nervousness, agitation, psychological fatigue and depression in the past four weeks (ABS 2018b).
Based on self-reported data from the 2020–21 NHS, of males aged 18 years and over:
- 1 in 5 (20%) males who had ever served in the ADF experienced high/very high psychological distress. This was similar to those who had never served in the ADF (16%).
- Of those who had ever served, DVA clients had similar rate of experiencing high/very high psychological distress to non-DVA clients (#19%1 and 20% respectively) (AIHW analysis of ABS 2022).
Deaths
In 2021, a study population of members who served in the ADF between 1985 and 2019 was created by using administration data from historical and current ADF personnel systems. Previous analysis on ADF members were restricted to members who served in the ADF from 2001 and were based on the current ADF personnel system.
The expansion of the ex-serving population has more than doubled from previous analysis. The larger study population enables more detailed analysis, providing greater insight into the risk and protective factors within the permanent, reserve, and ex-serving populations. A limitation is the study population does not include members who separated prior to 1 January 1985. For more information, see Serving and ex-serving Australian Defence Force members who have served since 1985: population characteristics 2019.
Between 2001 and 2019, there were 12,060 registered deaths among members with ADF service since 1 January 1985. Of these, around 10,800 (89%) occurred among ex-serving ADF members, almost 600 (5.0%) among permanent ADF members and 680 (5.6%) among reserve ADF members (Table 3).
| Males | Females | Persons | |
|---|---|---|---|
| Permanent | 550 | 47 | 597 |
| Reserve | 628 | 52 | 680 |
| Ex-serving | 10,017 | 766 | 10,783 |
| Total in all ADF service groups(a) | 11,195 | 865 | 12,060 |
| Total deaths in Australian population(b) | 1,419,131 | 1,339,953 | 2,759,084 |
(a) Consists of deaths by all causes for males and females aged 16 years and over for permanent, reserve, and ex-serving ADF members.
(b) Number of deaths by all causes for all ADF members are included in the Australian population deaths by all causes count.
Source: AIHW analysis of linked Defence Historical Personnel data–PMKeyS–NDI data 1985–2019, AIHW NMD 2002–2019.
The number of deaths by permanent, reserve, and ex-serving members with at least 1 day of service since 1 January 1985 by year is presented in Table 4. When interpreting Table 4, it is important to remember that the ex-serving population increases each year.
| Year | Permanent | Reserve | Ex-serving | Total in all ADF service groups(a) |
|---|---|---|---|---|
| 2001 | 41 | 35 | 250 | 326 |
| 2002 | 42 | 40 | 252 | 334 |
| 2003 | 30 | 28 | 320 | 378 |
| 2004 | 24 | 33 | 336 | 393 |
| 2005 | 34 | 36 | 339 | 409 |
| 2006 | 29 | 35 | 369 | 433 |
| 2007 | 32 | 42 | 415 | 489 |
| 2008 | 29 | 30 | 424 | 483 |
| 2009 | 33 | 49 | 489 | 571 |
| 2010 | 42 | 37 | 502 | 581 |
| 2011 | 43 | 37 | 559 | 639 |
| 2012 | 29 | 38 | 610 | 677 |
| 2013 | 24 | 47 | 637 | 708 |
| 2014 | 26 | 44 | 723 | 793 |
| 2015 | 28 | 25 | 774 | 827 |
| 2016 | 27 | 37 | 823 | 887 |
| 2017 | 38 | 24 | 947 | 1,009 |
| 2018 | 23 | 32 | 975 | 1,030 |
| 2019 | 23 | 31 | 1,039 | 1,093 |
| Total | 597 | 680 | 10,783 | 12,060 |
(a) Consists of deaths by all causes for males and females aged 16 years and over for permanent, reserve, and ex-serving ADF members.
Source: AIHW analysis of linked Defence historical personnel data–PMKeyS–NDI data 1985–2019.
Figures 7 and 8 show age-specific all-cause mortality rates of males and females who served in the ADF since 1985 for the period 2002–2019. Data for 2001 are not included in the calculation of these rates, as data for the permanent and reserve populations were not available before 2002 due to a change in Defence personnel management systems at that time. Analysis of ex-serving personnel was restricted to data from 2002 onwards, in line with reporting for permanent and reserve ADF population groups.
Age-specific all-cause mortality rates for permanent, reserve, or ex-serving ADF males were lower than rates for Australian males, except for ex-serving ADF males aged 16–29 where the rate was higher than Australian males (Figure 7).
Figure 7: Age-specific rates of all-cause mortality (per 100,000 population per year), males in ADF service status group with at least 1 day of service since 1 January 1985 and Australian males, 2002–2019
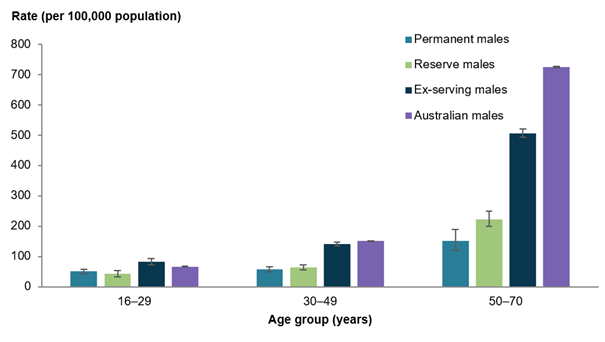
Notes
1. The thin vertical lines superimposed over the top end of each bar are 95% confidence intervals.
2. Rate of all-cause mortality in the Australian population matched by sex and within the same age range.
Chart: AIHW.
Source: AIHW analysis of linked Defence historical personnel data–PMKeyS–NDI data 1985–2019; AIHW NMD 2002–2019. See Health of veterans: supplementary data tables – Table S4.
Due to the small number of deaths among females in permanent and reserve service, these service status groups have been aggregated.
Age-specific all-cause mortality rates for permanent and reserve ADF females were lower than rates for Australian females. For ex-serving ADF females compared with Australian females (Figure 8):
- Ex-serving ADF females aged 16–29 had a higher rate.
- Ex-serving ADF females aged 30–49 had a similar rate.
- Ex-serving ADF females aged 50–70 had a lower rate.
Figure 8: Age-specific rates of all-cause mortality (per 100,000 population per year), ex-serving ADF females with at least 1 day of service since 1 January 1985 and Australian females, 2002–2019
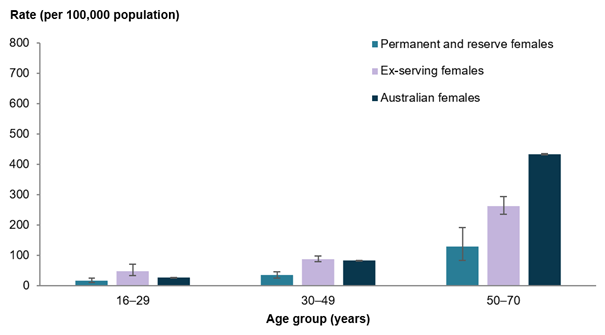
Notes
1. The thin vertical lines superimposed over the top end of each bar are 95% confidence intervals.
2. Rate of all-cause mortality in the Australian population matched by sex and within the same age range.
Chart: AIHW.
Source: AIHW analysis of linked Defence historical personnel data–PMKeyS–NDI data 1985–2019; AIHW NMD 2002–2019. See Health of veterans: supplementary data tables – Table S5.
Leading causes of death
Tables 5 and 6 provide the top leading cause of death in permanent, reserve, and ex-serving ADF males and ex-serving females for 2002–2019 for age groups, with the Australian comparison.
For permanent, reserve, and ex-serving ADF males, and males in the Australian population aged 16–49, the leading cause of death was suicide, except for permanent males aged 16–29 where the leading cause was land transport accidents (Table 5). For those aged 50 years and over, the leading cause of death for all groups was Coronary Heart Disease.
Additional information on leading causes of death is available in Health of veterans: supplementary data tables – Tables S9 and S10.
| Age group (years) | Permanent males | Reserve males | Ex-serving males | Australian males |
|---|---|---|---|---|
| 16–29 | Land transport accidents (38.6%) | Suicide (29.2%) | Suicide (42.2%) | Suicide (29.1%) |
| 30-49 | Suicide (20.8%) | Suicide (22.4%) | Suicide (25.3%) | Suicide (17.4%) |
| 50 years and over | Coronary heart disease (12.3%) | Coronary heart disease (11.6%) | Coronary heart disease (14.1%) | Coronary heart disease (16.5%) |
(a) Excludes 174 male deaths that have no underlying cause recorded.
(b) Proportions are of all deaths with a recorded underlying cause of death within each age group.
Source: AIHW analysis of linked Defence historical personnel data–PMKeyS–NDI data 1985–2019, AIHW NMD 2002–2019.
The leading cause of death for ex-serving ADF females, and females in the Australian population was death by suicide for those aged 16–29 (Table 6). Whereas for those aged 30–49 and 50 years and over, the leading cause of death was different for ex-serving ADF females, and females in the Australian population.
Figures were too small to present leading causes of death by age group for permanent and reserve ADF females separately.
| Age group (years) | Ex-serving females | Australian females |
|---|---|---|
| 16–29 | Death by suicide (41.4%) | Death by suicide (22.0%) |
| 30-49 | Death by suicide (18.0%) | Breast cancer (12.6%) |
| 50 years and over | Breast cancer (14.6%) | Coronary heart disease (14.3%) |
(a) Excludes one female death that has no underlying cause recorded.
(b) Proportions are of all deaths with a recorded underlying cause of death within each age group.
Source: AIHW analysis of linked Defence historical personnel data–PMKeyS–NDI data 1985–2019, AIHW NMD 2002–2019.
Death by suicide among ADF members
There is continuing concern within the ADF and the wider Australian community about deaths by suicide in permanent, reserve, and ex-serving ADF members. In particular, the ex-serving members may face increased risk of death by suicide (AIHW 2021). For the latest available information on serving and ex-serving ADF members who died by suicide, see Serving and ex-serving Australian Defence Force members who have served since 1985: suicide monitoring 1997 to 2020.
The below section uses data from the Serving and ex-serving Australian Defence Force members who have served since 1985: suicide monitoring 2001 to 2019 report to remain consistent with the data reference periods used in the broader Deaths section of this report.
Death by suicide by age and service status group
Between 2001 and 2019 there were 1,273 certified deaths by suicide among members with ADF service since 1 January 1985 (AIHW 2021).
For those with service since 1985, the rate of death by suicide was highest for ex-serving males. Rates of death by suicide between 2002 and 2019 by service status and sex were as follows:
- 11.3 per 100,000 population per year for permanent males
- 12.5 per 100,000 population per year for reserve males
- 29.8 per 100,000 population per year for ex-serving males
- 14.9 per 100,000 population per year for ex-serving females.
Due to the small number of deaths by suicide among females in permanent and reserve service, rates of deaths by suicide are not reported for these subgroups.
Compared with the Australian population and after adjusting for age, rates of deaths by suicide between 2002 and 2019 were:
- 51% lower for permanent males
- 48% lower for reserve males
- 24% higher for ex-serving males
- 102% (or 2.02 times) higher for ex-serving females (AIHW 2021).
Younger age groups are at greater risk of suicide
The rates of death by suicide for both ex-serving males and females between 2002 and 2019 varied by age at time of death by suicide. Between 2002 and 2019, the rate of death by suicide for ex-serving males aged 50 years and over was lower than ex-serving males under 50 years of age (18.9 and 35.2 per 100,000 population per year). However, ex-serving females’ rates of death by suicide were similar regardless of age at death by suicide (AIHW 2021).
Those with a longer length of service have lower rates of death by suicide
Rates of death by suicide between 2002 and 2019 for ex-serving males decreased as length of service increased. The rate of death by suicide was lowest for ex-serving males who served more than 20 years (15.4 per 100,000 population per year) and highest for those who had served less than one year (46.4 per 100,000 population per year) (AIHW 2021).
Those who separate as commissioned officers have lower rates of death by suicide
Between 2002 and 2019, the rates of death by suicide for ex-serving males who were commissioned officers at the time of separation was half that of those who were all other ranks (15.1 compared with 31.8 per 100,000 population per year). For ex-serving females, rates of death by suicide were similar for both commissioned officers and all other ranks (AIHW 2021).
Members who separate voluntarily have lower rates of death by suicide
Due to a change in the way the reason for separating from the ADF was recorded in 2002, analysis is presently only reported for ADF members who separated from 1 January 2003 onwards. Between 2003 and 2019, the rate of death by suicide for ex-serving males by reason for separation was lowest for those who separated voluntarily (22.2 per 100,000 population per year) and highest for those whose reason for separation was involuntary medical (73.1 per 100,000 population per year). In addition, ex-serving males who separated voluntarily from the ADF have a similar rate of death by suicide as the Australian males (22.4 compared with 22.2 per 100,000 population per year) (AIHW 2021).
If you need help or support, please contact:
Open Arms - Veterans and Families Counselling 1800 011 046
Open Arms Suicide Intervention
Defence All-hours Support Line (ASL) 1800 628 036
Defence Member and Family Helpline 1800 624 608
Defence Chaplaincy Support 1300 333 362
Lifeline 13 11 14
Suicide Call Back Service 1300 659 467
Beyond Blue Support Service 1300 22 4636
For information on support provided by DVA, see:
Disability
A disability or restrictive long-term health condition exists if a limitation, restriction, impairment, disease, or disorder has lasted, or is expected to last, for 6 months or more, and restricts everyday activities (ABS 2019).
According to the 2020–21 NHS, a disability or restrictive long-term condition is classified by whether or not a person has a specific limitation or restriction. There are 5 levels of activity limitation in the 2020–21 NHS: profound, severe, moderate, mild and school/employment restriction. These are based on whether a person needs help, has difficulty, or uses aids or equipment with any core activities (mobility, self-care, and communication).
According to self-reported data from the 2020–21 NHS, almost 2 in 5 (37%) males who had ever served in the ADF had a disability with a limitation or restriction, while 1 in 5 (20%) had a disability but with no limitation or restriction. These proportions were around twice as high as those of males who had never served (17% and 12%, respectively) (AIHW analysis of ABS 2022a).
Further information will be available from the Survey of Disability, Ageing and Carers (SDAC), with detailed information from this survey expected to be available from the ABS in late-2023.
The DVA supports many veterans who suffer from injuries or diseases caused or aggravated by ADF service. As at 30 June 2021, there were over 189,500 veterans with an accepted disability, equating to 72% of the DVA treatment population (DVA 2021).
1 Proportions marked with a hash (#) have a high MoE and should be interpreted with caution. A high MoE is considered as greater than 10%.
2 These results include males aged 18 years and over, however, COPD occurs mostly in people aged 45 and over. While it is occasionally reported in younger age groups, in those aged 45 and over there is more certainty that the condition is COPD and not another respiratory condition. As such, COPD results should be interpreted with caution.
ABS (Australian Bureau of Statistics) (2018a) Self-assessed health status, ABS, Australian Government, accessed 11 May 2022.
ABS (2018b) Mental Health, ABS, Australian Government, accessed 06 December 2022.
ABS (2019) Disability, Ageing and Carers, Australia: Summary of Findings, 2018, ABS, Australian Government, accessed 11 May 2022.
ABS (2022a) Microdata: National Health Survey, 2020–21, AIHW analysis of detailed microdata, accessed 10 October 2022.
ABS (2022b) National Study of Mental Health and Wellbeing, ABS, Australian Government, accessed 30 September 2022.
AIHW (Australian Institute of Health and Welfare) (2021) Serving and ex-serving Australian Defence Force members who have served since 1985: suicide monitoring 2001 to 2019, AIHW, Australian Government, accessed 11 May 2022.
DVA (Department of Veterans Affairs) (2015) Social Heath Strategy 2015–2023 for the Veteran and Ex-Service Community, DVA, Australian Government, accessed 20 March 2022.
DVA (2021) Department of Veterans’ Affairs annual report 2020–21, DVA, Australian Government, accessed 11 May 2022.
Joint Standing Committee on Foreign Affairs, Defence and Trade (2019). Inquiry into transition from the Australian Defence Force (ADF), Parliament of the Commonwealth of Australia, Australian Government, accessed 26 October 2022.
Rafferty LA, Cawkill PE, Setvelink SAM, Greenberg K and Greenberg N (2018) ‘Dementia, post-traumatic stress disorder and major depressive disorder: a review of the mental health risk factors for dementia in the military veteran population’, Psychological Medicine, 48(9):1400–1409, doi:10.1017/S0033291717001386.
Singer CM (2015) ‘Dementia risk factors in veterans’, Journal of Aging Life Care, accessed 29 June 2020.


