Mental illness and substance use
Substance use and substance use disorder can precede and increase the risk of developing other mental disorders, and vice versa.

There is a high prevalence of substance use disorder and another mental disorder co-occurring within the same individual.
People living with substance use disorder and another co-occurring mental illness experience greater combined disease severity and poorer outcomes than those who experience these conditions individually.
What is the relationship between mental illness and substance use?
The relationship between mental illness and substance use is complex. A mental illness may make a person more likely to use drugs as an attempt to self-medicate symptoms associated with their mental illness. Conversely, substance use may be a contributing factor for the initial symptoms of mental illness. Certain substances may cause a substance-induced psychosis which can last for days or weeks after the end of intoxication. There is evidence that individuals who experience substance-induced psychosis are at significant risk of later transitioning to long-term psychotic illness (Vassos 2023). Critically, this does not mean that substance use necessarily triggers mental illness or vice versa: common risk factors (such as trauma, personality traits, genetic influences and the childhood environment) may cause substance use and mental illness to independently develop in the same individual (UNODC 2022).
The 2019 National Drug Strategy Household Survey (NDSHS) (Figure ATOD.1) found that, compared with adults without a mental illness, those with a mental illness were:
- more likely to drink alcohol at risky levels (21% compared with 17%)
- twice as likely to smoke (20% compared with 10%)
- 1.7 times as likely to use illicit any drug (26% compared with 15%)
- about twice as likely to use meth/amphetamines (2.6% compared with 1.2%)
- about twice as likely to use pharmaceuticals for non-medical purposes (8% compared with 4%).
For more information see Alcohol, tobacco and other drug use in Australia: People with mental health conditions.
Figure ATOD.1 Is there a difference in rates of substance use according to mental health status?
Horizontal bar chart showing percentage of people aged 18 years and older in 2019 who used alcohol, tobacco and illicit drugs according to whether in the previous 12 months they had been (a) diagnosed or treated for a mental illness or (b) not diagnosed or treated for a mental illness. Across all substance categories (Alcohol use – Lifetime risk; Alcohol use – Single occasion risk [at least monthly]; Daily smoking; Any illicit drug use; Cannabis use; Cocaine use; Ecstasy use; Meth/amphetamine use; Use of pharmaceuticals for non-medical purposes) substance use is higher among people diagnosed or treated for a mental illness compared with people not diagnosed or treated for a mental illness.
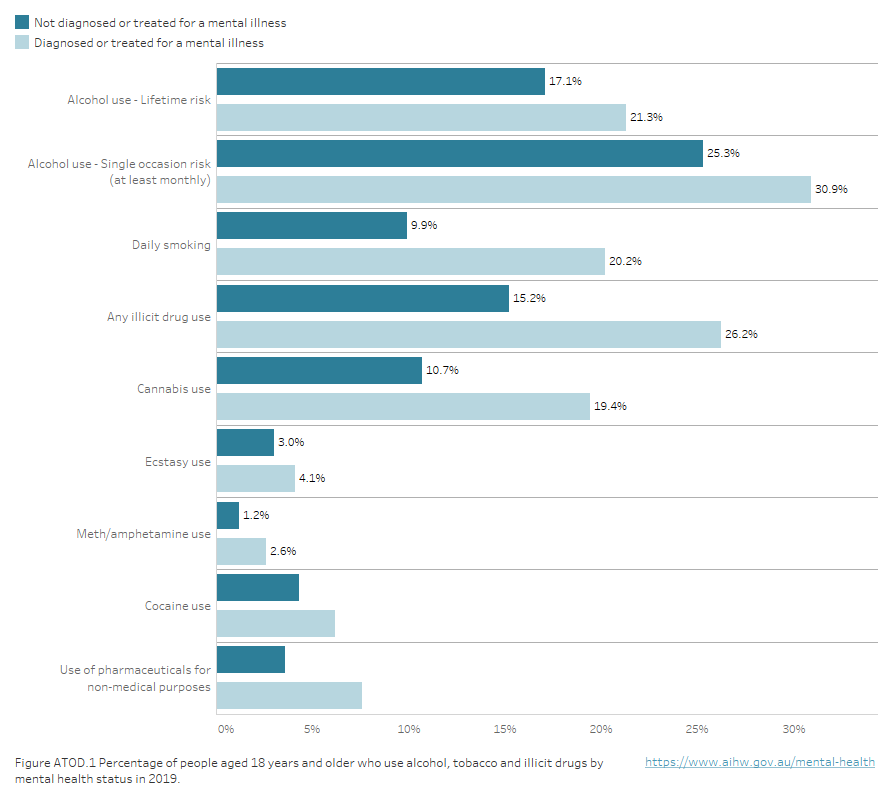
Notes.
- Alcohol use – Lifetime risk: risky is defined by the 2009 NHMRC guideline 1 as ‘on average, had more than 2 standard drinks per day’.
- Alcohol use – Single occasion risk is derived from the National Health and Medical Research Council (NHMRC) 2009 guideline 2 ‘had more than 4 standard drinks on one occasion at least once a month’.
- Mental illness includes depression, anxiety disorders, schizophrenia, bipolar disorder, eating disorders, and other forms of psychosis.
- Any illicit drug use; Cannabis use; Cocaine use; Ecstasy use; Meth/amphetamine use; and Use of pharmaceuticals for non-medical purposes are defined as having used the specified drug in the 12 months prior to the survey.
Source: AIHW 2020
A recent study of Australian general practice records (Belcher et al. 2021) showed the rate of moderate to heavy drinking among patients with severe mental illness and/or long-term mental illness was 4.7%, more than double that for the population without (2.2%). The same study also showed almost half (47%) of people with severe or long-term mental illness are current or past smokers, compared with one third (30%) of the population without (Belcher et al. 2021).
The 2010 National Survey of High Impact Psychosis (SHIP) showed rates of smoking, harmful use and dependence of alcohol and illicit drugs among adults living with psychotic illness were well above the general population. Among those living with psychotic illness, 66% reported currently smoking compared with 25% of the general population. Half of people living with psychotic illness (51%) had a lifetime history of harmful alcohol use or dependence, double the rate in the general population (25%), and over half (55%) had a lifetime history of harmful illicit drug use or dependence – 6 times the rate of the general population (9%) (Morgan et al. 2012).
Comorbidity of substance use disorders with other mental illnesses
Substance use disorders – which are categorised as mental disorders – are the third most prevalent category of mental disorder among Australian adults, with an estimated 650,000 (3%) Australian adults experiencing substance use disorders in the 12 months prior to the 2020–2022 National Study of Mental Health and Wellbeing (ABS 2023).
Comorbidity between substance use disorders and other mental illnesses is common (Mills et al. 2019). According to the NSMHW 2020–2022, while 9% of people who met the diagnostic criteria for an anxiety disorder or affective disorder also met the criteria for a substance use disorder, 46% who met the diagnostic criteria for substance use disorder, also met the criteria for an anxiety or affective disorder (ABS 2023). Among people entering alcohol and other drug treatment programs in Australia, between 50–76% meet the diagnostic criteria for at least one comorbid mental disorder (see Mills et al. 2019).
Comorbidity of substance use disorders and other mental illnesses increases the already heavy burden a person would experience with either of these in isolation (Leung et al. 2016). Compared to people with no comorbidity, people with comorbid substance use disorder and mental illness are more likely to experience poorer short- and long-term outcomes for their mental health and substance use, levels of impairment that are more severe, and greater use of health services (Leung et al 2016).
While mental illness is associated with a reduced life expectancy (Lawrence et al. 2013), research has shown that the combination of substance use disorder with another mental illness is associated with markedly higher mortality rates and larger reductions in life expectancy (Plana-Ripoll et al 2020). This is commensurate with the relatively high fatal disease burden associated with substance use disorders compared to most other types of mental illness. While the 2023 Australian Burden of Disease Study does not contain data on comorbidity of substance use disorders and other mental illness, Mental and substance use disorders were estimated to be responsible for 15% of the total burden of disease, placing it second as a broad disease group after Cancer (17%) (AIHW 2023).
Where can I find more information?
For more information, refer to:
- Alcohol, tobacco and other drugs in Australia: People with mental health conditions
- National Drug Strategy Household Survey 2019
- Physical health of people with mental illness
- National Study of Mental Health and Wellbeing, 2020–2022
- Australian Burden of Disease Study 2023
Key concept | Description |
|---|---|
| Burden of disease | Burden of disease is measured in disability-adjusted life years (DALYs) – years of life lost due to premature mortality (fatal burden) and years of healthy life lost due to poor health (non-fatal burden). |
Comorbidity refers to occurrence of more than 1 condition/disorder at the same time. | |
Fatal burden is the burden from dying prematurely as measured by years of life lost (YLL). Often used synonymously with years of life lost, and also referred to as ‘life lost’. | |
Psychotic illnesses are a diverse group of illnesses characterised by fundamental distortions of thinking, perception and emotional response. Two of the main symptoms are delusions and hallucinations. Psychotic illnesses are classified according to diagnostic criteria in the ICD-10 and include:
| |
Severe mental illness – often used interchangeably with serious mental illness and severe and persistent mental illness – commonly includes diagnoses of schizophrenia, major affective disorders and some personality disorders resulting in lifelong disabling conditions that severely impair personal and social functioning, and require ongoing and long-term support and treatment. These terms lack consensus definition but are commonly characterised by the combination of diagnosis, disability and duration (Zumstein and Riese 2020). | |
As opposed to substance use which may occur without disorder, substance use disorder is the persistent use of drugs (including alcohol and tobacco) despite serious harms and negative consequences associated with their use. Substance use disorders are classified as mental disorders. In the International Statistical Classification of Diseases and Related Health Problems,10th revision (ICD-10) , substance use disorders come under the block Mental and behavioural disorders due to psychoactive substance use. This block contains a wide variety of disorders that differ in severity and clinical form but that are all attributable to the use of one or more psychoactive substances, which may or may not have been medically prescribed. For more information on the classification of substance use disorders in the NSMHW 2020–2022, see the National Study of Mental Health and Wellbeing Methodology. |
ABS (2023) National Study of Mental Health and Wellbeing, 2020-22: Summary of results, ABS, Australian Government, accessed 12 October 2023.
Australian Institute of Health and Welfare (AIHW) (2020) National Drug Strategy Household Survey 2019, AIHW, Australian Government, accessed 15 March 2022.
AIHW (2023) Australian Burden of Disease Study 2023, AIHW, Australian Government, accessed 10 January 2024.
Belcher J, Myton R, Yoo J, Boville C and Chidwick K (2021) ‘Exploring the physical health of patients with severe or long-term mental illness using routinely collected general practice data from MedicineInsight’, Australian Journal of General Practice, 50(12):944–949, doi:10.31128/AJGP-08-20-5563
Lawrence D, Hancock K and Kisely S (2013) ‘The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers’, British Medical Journal, 346:f2539, doi:10.1136/bmj.f2539.
Leung J, Stockings E, Wong I, Galasyuk N, Diminic S, Leitch E, Whiteford H, Degenhardt L, Ritter A and Harris M (2016) Co-morbid mental and substance use disorders - A meta-review of treatment effectiveness, Technical Report Number 336, National Drug and Alcohol Research Centre, University of New South Wales, Sydney.
Mills K, Marel C, Madden E and Teesson M (2019) Lessening the Burden of Comorbid Substance Use and Mental Disorders Through Evidence-Based Care: The Case for a National Minimum Qualifications Strategy, Submission to the Australian Government Productivity Commission Mental Health Inquiry, Matilda Centre for Research in Mental Health and Substance Use, University of Sydney, Sydney.
Morgan VA, Waterreus A, Jablensky A, Mackinnon A, McGrath JJ, Carr V, Bush R, Castle D, Cohen M, Harvey C, Galletly C, Stain HJ, Neil AL, McGorry P, Hocking B, Shah S and Saw S. (2012) ‘People living with psychotic illness 2010: The second Australian national survey’ Aust N Z J Psychiatry, 46(8):735-52, doi: 10.1177/0004867412449877.
Plana-Ripoll O, Musliner KL, Dalsgaard S, Momen NC, Weye N, Christensen MK, Agerbo E, Iburg KM, Laursen TM, Mortensen PB, Pedersen CB, Petersen LV, Santomauro DF, Vilhjálmsson BJ, Whiteford HA and McGrath JJ (2020) ‘Nature and prevalence of combinations of mental disorders and their association with excess mortality in a population-based cohort study’ World Psychiatry, 19(3):339-349, doi: 10.1002/wps.20802
Walker ER, McGee RE and Druss BG (2015) ‘Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis’, JAMA Psychiatry, 72(4):334–341, doi:10.1001/jamapsychiatry.2014.2502.
United Nations Office on Drugs and Crime (UNODC) (2022) Comorbidities in drug use disorders: No wrong door, Discussion paper, UN, accessed 17 October 2023.
Vassos E (2023) What is the Link Between Substance-Induced Psychosis and Primary Psychotic Disorders? Am J Psychiatry, 180(6):404-406, doi: 10.1176/appi.ajp.20230298.
Zumstein N and Riese F (2020) ‘Defining Severe and Persistent Mental Illness-A Pragmatic Utility Concept Analysis’ Front Psychiatry 11:648. doi:10.3389/fpsyt.2020.00648.
Data in this section were late updated in February 2024.


