Non-ST segment elevation myocardial infarction (NSTEMI)
Non-ST segment elevation myocardial infarction (NSTEMI) is a type of heart attack in which an artery is frequently partially blocked. This severely reduces blood flow. Almost half (48%) of the acute coronary syndrome (ACS) cohort had a diagnosis of NSTEMI.
- Almost half the people with NSTEMI had an interventional procedure. Compared to people who did not have an interventional procedure, these people:
- were younger, had a lower rate of prior CHD, more likely to be men
- were more likely to initiate the recommended medication regimen
- had better health outcomes.
- People with NSTEMI had the most variation in treatment pathways. The 3 most common treatment pathways captured the experience of 68% of people with NSTEMI, (compared to 76% for people with STEMI and 82% for people with unstable angina).
- The treatment pathways with the lowest proportion of people who experienced adverse health outcomes were those who had a procedure and either, did not initiate or persist with 4 classes of medications or those who initiated within 40 days and were still taking all 4 classes at 1 year post discharge.
Explore the treatment pathways for the people with this diagnosis in Figure 6 and information about the people who followed theses pathways in Figure 7.
A summary of these treatment pathways and the people who followed them is below.
Figure 6: Treatment pathways and outcomes, among those with NSTEMI
The Sankey shows the proportion of people who followed different treatment pathways illustrated with the 3 measurement points and survival at 3 years.
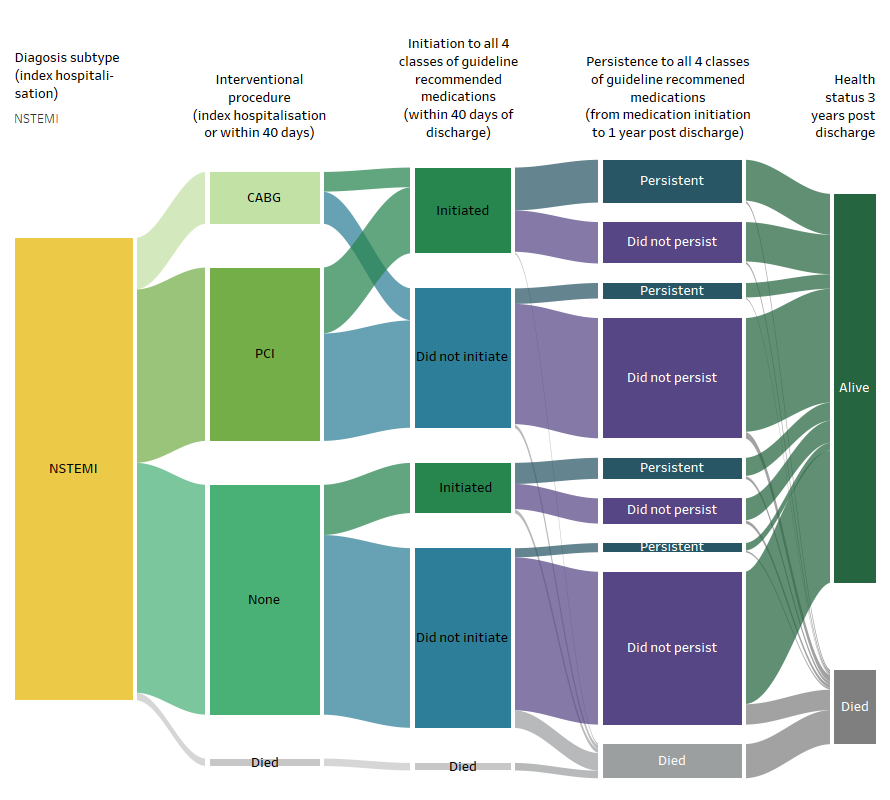
Source: AIHW NIHSI 2016-17 to 2019-20, analysis of NIHSI
Figure 7: Age group, sex, comorbidities, and health outcomes among those with NSTEMI, by treatment subgroup
Figuresshow that among those with NSTEMI, the most common age group is 65-74 andcomorbidity is hypertension.
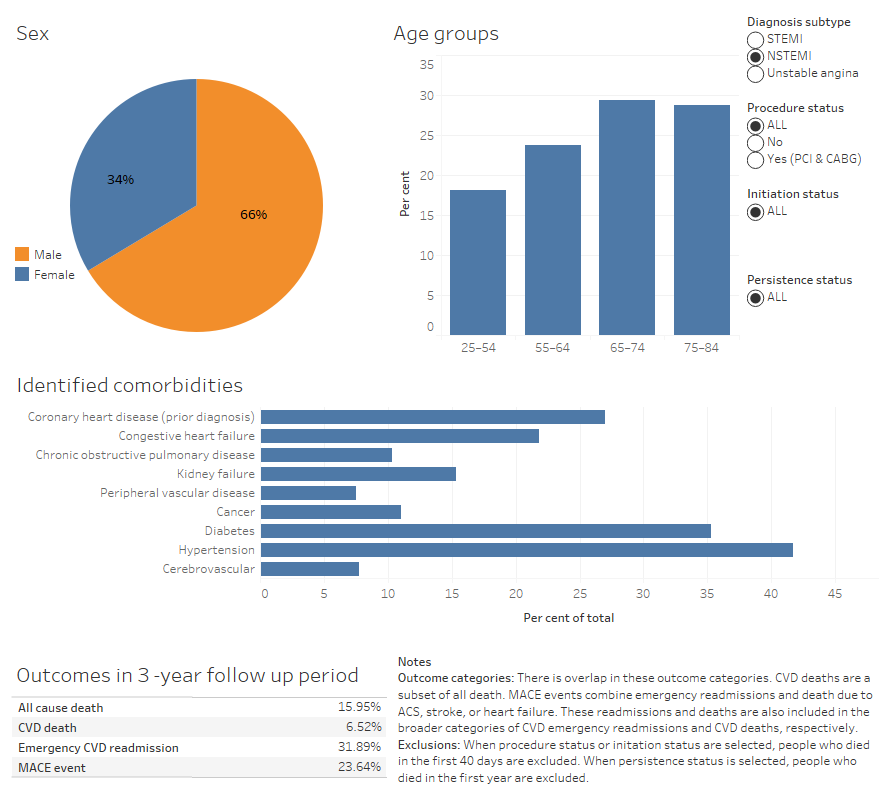
Source: AIHW NIHSI 2010–11 to 2019–20, analysis of NIHSI
People’s treatment pathways after a NSTEMI hospitalisation
People’s treatment pathways are described using 3 measurement points during or after their initial ACS hospitalisations (referred to as the index hospitalisation).
Note that differences in health outcomes experienced by people following different treatment pathways should not be interpreted as causal. Many factors, impact both treatment decisions and the risk of experiencing poor health outcomes.
Measurement point 1: Interventional procedure
Of those with NSTEMI, 11% underwent a CABG procedure, and 38% underwent a PCI at the index stay or within 40 days of discharge. Those who did not undergo a procedure tended to be older, with a greater proportion of people aged 65 and over (no procedure: 64% CABG: 57%, PCI: 50%), have higher rates of prior CHD (no procedure: 34% CABG: 17%, PCI: 21%), and more be likely women (no procedure: 42% CABG: 21%, PCI: 26%).
Thirty seven percent of people who did not have a procedure had an emergency CVD readmission, 28% had a MACE and 22% died within 3 years. In comparison, among those who underwent a CABG procedure, 25% had an emergency readmission, 16% had a MACE and 7% died. Among those who underwent a PCI, 27% had an emergency CVD readmission, 19% had a MACE and 8% died within 3 years.
Measurement point 2: Medication initiation
Thirty percent of people with NSTEMI initiated all 4 guideline indicated medication classes within 40 days of hospital discharge. The proportion was higher among those who underwent a procedure (38%) compared to those who did not (22%).
Among those who did not undergo a procedure, a higher proportion of people who initiated 4 classes of medicines at 40 days had an emergency CVD readmission (41% and MACE (34%) compared with people who did not initiate (36% and 26% for emergency readmissions and MACE respectively). This may reflect higher risk profiles driving both medication decisions and health outcomes.
Among those who did undergo a procedure, there was little difference in the outcomes among those who did and did not initiate all 4 medication classes at 40 days (see Figure 7).
Measurement point 3: Persistence to medication
Note, persistence measures are only estimated for those who were alive at one year. All comparisons below exclude people who died in the first year after index hospitalisation.
Among people with NSTEMI alive at 1 year post hospital discharge, 21% continued to take all 4 guideline indicated medication classes. Those who did not undergo a procedure or initiate the 4 drug classes within 40 days post discharge, but had medications supplied later and were then persistent at 1 year, had worse health outcomes when compared to other NSTEMI treatment subgroups. One in 2 had an emergency CVD readmission, 2 in 5 had a MACE and 17% died in the follow up period. In some cases, the later initiation of medication may have been in response to the readmission event.
The subgroups with the lowest proportion of people who experienced adverse health outcomes were those who had a procedure but did not initiate or persist with 4 classes of medications (readmissions: 25% MACE: 17% death: 5.4%) and those who had a procedure, initiated within 40 days and were still taking all 4 classes at 1 year post discharge (readmissions: 26% MACE: 18% death: 4.5%).
See Figure 7 for comparisons of age group, sex, comorbidities and health outcomes among treatment groups.


