Changes to the cancer risk data and guidance using the risk methods
Cancer data commentary no. 1
The 2020 release of Cancer data in Australia (CDiA) contains a greater range of risk data than previous AIHW releases. This cancer data commentary provides guidance on using the new risk data and summarises key changes.
Changes to CDiA include the following:
- Previously, the only risk data available was not adjusted for competing mortality; now risk adjusted for competing mortality is also available
- Risk by age 5 up to risk by age 90 (in 5-year increments) and lifetime risk are now released – previously only risk by age 75 and by age 85 were available
- Because of methodological issues associated with its derivation, ‘All cancers combined’ incidence risk time series is not available
- While the previous method of calculating incidence risk (not adjusted for competing mortality) has been revised, the new method is similar to the previous method and produces comparable results (with the exception of ‘All cancers combined’ incidence).
‘Cancer risk’ is generally used to describe the risk of being diagnosed with, or the risk of dying from, cancer.
CDiA includes a ‘risk adjusted for competing mortality’ (AdjCom) method and a ‘risk unadjusted for competing mortality’ (RUCM) method. A more technical overview of the methods is available in the methods section of CDiA.
Risk unadjusted for competing mortality only considers the likelihood of being diagnosed with, or dying from, cancer. ‘Competing mortality’ considers the probability of a certain event occurring for a person (e.g. diagnosis of cancer, death from cancer) while taking into account the fact that the person might die before the event happens. The additional factor of competing mortality results in an estimate that better reflects the ‘real world’ risk but it also produces more complex comparisons. In particular, to what extent are changes in risk over time, or differences between the risk for two populations, influenced by competing mortality and to what extent are they driven by cancer risk?
Why publish two risk methods?
The different methods have their own respective strengths and limitations. Therefore, one method may be better suited to inform a particular investigation than the other. Guidance on using the methods is provided in more detail in the following sections.
What are the practical differences between the risk methods?
AdjCom measures risk by taking into account the mortality that occurs due to other causes whereas RUCM does not. The following hypothetical situation helps highlight the practical differences.
- Suppose that in 1982 and then in 2015, only people aged 10 to 14 were diagnosed with condition X and only people aged 85 to 89 were diagnosed with condition Y.
- Suppose that the number of people who were diagnosed with condition X was equal to 0.5% of the population alive aged 10 to 14, and the number of people who were diagnosed with condition Y was equal to 0.5% of the population alive aged 85 to 89.
Table 1 provides the risk of diagnosis using RUCM and AdjCom for conditions X and Y in 1982 and 2015 and calculates the risk for each condition.
Condition | RUCM 1982 | RUCM 2015 | AdjCom 1982 | AdjCom 2015 |
|---|---|---|---|---|
Condition X | 2.4690% (1 in 41) | 2.4690% (1 in 41) | 2.4635% (1 in 41) | 2.4889% (1 in 40) |
Condition Y | 2.4690% (1 in 41) | 2.4690% (1 in 41) | 0.4822% (1 in 207) | 1.0636% (1 in 94) |
Observations:
- RUCM for conditions X and Y were the same for 1982. RUCM does not distinguish between age groups. A population risk based only on a rate of 0.5% of 10 to 14 year olds will be the same as a population risk based only on 0.5% of all 85 to 89 year olds.
- AdjCom for condition Y is less than AdjCom for condition X. When competing mortality is taken into account, people have less chance of being diagnosed with condition Y than condition X because a much smaller proportion of people reach age 85 than reach age 10.
- RUCM has remained the same over time. For conditions X and Y, RUCM is the same from 1982 to 2015 because the incidence rates of X and Y have remained unchanged and RUCM does not distinguish between age groups or the likelihood of surviving to a given age.
- AdjCom has increased over time. The risk of being diagnosed with condition Y has more than doubled, even though the incidence rates in 1982 and 2015 are the same (0.5% of the population aged 85 to 89). This occurred because a much greater proportion of people are living to the age of 85 in 2015 than in 1982.
Please note that RUCM minus AdjCom does not somehow isolate the effect of competing mortality. In fact, AdjCom can be higher than RUCM, as is the case for condition X in 2015 in the example above. To view RUCM and AdjCom formulas, please go to Cancer data in Australia methods section.
Which risk method should I use?
The selection of which risk method to use depends on the purpose of the investigation. The most complete understanding of risk is accomplished when using the two methods together.
By factoring in competing mortality, AdjCom provides a better estimate of ‘real world’ cancer risk (that is, a better approximation of the likelihood of being diagnosed with, or dying from, cancer in Australia). However, when viewing changes over time or between populations, the question when using AdjCom is “are the observed differences or changes due to competing mortality or due to the risk purely attributable to cancer?".
On the other hand, in not factoring in competing mortality, RUCM is less representative of the ‘real world’ risk, particularly at older ages. However, its strength is that comparisons and time series are solely attributable to cancer risk (i.e. not affected by differences in competing mortality).
Because the methods have opposing strengths and limitations, use of the two methods together can help provide a more complete understanding of risk. In general, when writing about cancer risk, AIHW cite AdjCom but also use RUCM to understand cancer-specific trends that are isolated from competing mortality.
How the risk methods can be used together
RUCM and AdjCom measure risk differently and are not directly comparable. However, the information from the respective time series can be used in a complementary manner to provide greater insights into changes over time; the following discussion of changes in lung cancer risk over time helps illustrate this by using AdjCom to estimate the ‘real world’ risk and RUCM to isolate cancer risk.
Between 1982 and 2020, the risk of persons being diagnosed with lung cancer by the age of 90 is estimated to have increased from 1 in 23 to 1 in 18. The increase in risk of being diagnosed with lung cancer by the age of 90 is mostly due to a greater proportion of people surviving to the ages where lung cancer is more commonly diagnosed but increasing lung cancer rates have contributed to some degree (Figure 1).
Figure 1: Risk of being diagnosed with lung cancer by the age of 90, risk adjusted for competing mortality and risk unadajusted for competing mortality, persons, 1982 to 2020
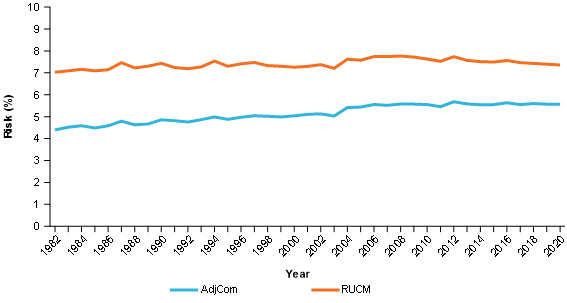
Source: AIHW ACD 2016
The above interpretation of lung cancer risk is undertaken by using AdjCom to provide the ‘real world’ estimate but RUCM to interpret cancer specific risk change over time. Given RUCM focusses only on cancer risk and the RUCM time series is considerably flatter than AdjCom, the sharper increase in AdjCom is likely predominantly due to changes in competing mortality over time.
When using RUCM to assist in the interpretation of AdjCom time series, note that RUCM less AdjCom does not equal competing mortality.
Difficulties using AdjCom to compare populations with different competing mortality
AdjCom comparisons between different populations are accurate but can be open to misinterpretation. Where readers are not aware of the competing mortality concept, it is likely that comparisons will be interpreted as only being due to cancer rates. Where readers are aware of the concept, the question often arises as to whether differences are due to competing mortality or cancer rates.
The potential for misinterpretation, and how to address the issue by using the methods together, is demonstrated in the following consideration of the question ‘Are males more likely to be diagnosed with pancreatic cancer?’.
AdjCom analysis:
The risk of males being diagnosed with pancreatic cancer by the age of 90 between 1982 and 2020 is generally quite similar to females (Figure 2).
RUCM analysis:
Between 1982 and 2020, males consistently have a greater risk of being diagnosed with pancreatic cancer by the age of 90 (Figure 2).
AdjCom used in conjunction with RUCM analysis:
Between 1982 and 2020, the risk of males being diagnosed with pancreatic cancer is quite similar to females. More precisely though, males have a greater risk of being diagnosed with pancreatic cancer but females are more likely to live to the ages where pancreatic cancer more commonly occurs (Figure 2).
Figure 2: Risk of being diagnosed with pancreatic cancer by the age of 90, by sex, RUCM and AdjCom, 1982 to 2020
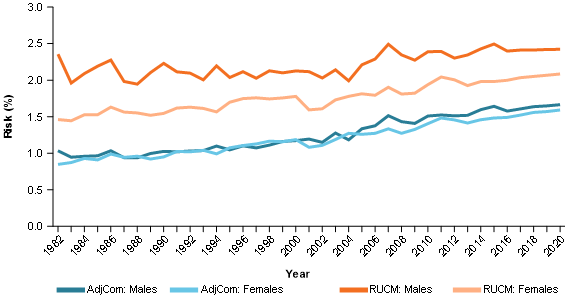
Source: AIHW ACD 2016
International cancer risk comparisons
When comparing Australian cancer risk data internationally, care should be taken to ensure the comparisons use the same method.
The International Agency for Research on Cancer presents international risk comparisons; these comparisons are unadjusted for competing mortality and the comparisons measure risk of being diagnosed with (based on cases), and risk of death from, specific cancers. The RUCM data AIHW produces is the most comparable method, noting that it measures the risk of being diagnosed for people, not cases (Appendix B provides information on the generally negligible difference between measuring risk of people being diagnosed with cancer and the risk of cancer cases being diagnosed).
General hints for using risk adjusted for competing mortality
Using life expectancy to help interpret change in risk adjusted for competing mortality
Over time, life expectancy is increasing. Cancer is more common in older ages and more people are surviving to older ages. Cancer specific risk may be increasing or decreasing depending on the cancer but the greater number of people reaching older ages, the greater the upwards pressure on the population’s cancer risk.
Using life expectancy to help risk adjusted for competing mortality comparisons
AdjCom comparisons between populations are influenced by cancer rates and competing mortality. RUCM can be used to identify which population has higher rates of cancer. In regards to competing mortality differences, the population with lower life expectancy should have less upwards pressure on risk to some extent because the population is less likely to live to the ages where cancer more commonly occurs.
Using ‘younger’ age groups to simplify interpreting risk adjusted for competing mortality
In many circumstances, risk will be used as supportive information or used a simple measure to inform a general audience. In such circumstances, it may be both undesirable and impractical to distinguish between competing mortality impacts and cancer specific impacts. If appropriate, consideration could be given to reporting on risk by age 75 in preference to older ages. Risk by age 75 is less impacted by competing mortality than older ages; this results in:
- RUCM and AdjCom estimates being more similar than at older ages and therefore less likely to provide contradictory comparisons or trends
- interpretation of risk over time, or between sexes, being more strongly influenced by cancer specific risk (cancer specific risk is assumed to be the focal point for many general audiences).
Lifetime risk may not be the most appropriate indicator to inform risk for the general population
Lifetime risk is not the risk for an average lifetime. Lifetime risk may be considered as risk by the age of the oldest person in the population for each year; this will be risk by age over 100 for the cancer data time series. Given most people are not expected to live to beyond 100, lifetime risk may not be the most appropriate indicator where the purpose is to provide the general population with a simple and relevant indication of cancer risk.
For both AdjCom and RUCM, risk is reported in 5-year increments from risk by age 5 to risk by age 90. Lifetime risk is also provided for AdjCom.
The provision of additional risk data by age allows interpretation of cancer risk, and cancer risk trends, for more stages of life.
The time series for All cancers combined incidence risk are not available because the RUCM and AdjCom methods cannot do so with suitable accuracy; the following paragraphs discuss this in more detail.
What should AdjCom and RUCM measure?
The AdjCom and RUCM methods should ideally calculate incidence risk only including people who have not been diagnosed with cancer before; the population who have previously been diagnosed with cancer realised their cancer incidence risk in the year they were first diagnosed with cancer.
What do AdjCom and RUCM measure?
The AdjCom and RUCM methods used calculate incidence risk based on the number of people diagnosed in the year, irrespective of whether individuals have been diagnosed with cancer in previous years.
Why can’t cancer incidence risk be calculated using only those diagnosed with cancer for the first time?
Over 100 years of cancer incidence data would be required to identify all people diagnosed with cancer for the first time so the data required to calculate the exact risk of diagnosis are not yet available, i.e. based only on those diagnosed with cancer for the first time.
A ‘best estimate’ of cancer incidence risk using the ‘first time diagnosed’ concept is provided in Attachment A. The ‘best estimate’ is provided for 2015 and uses 34 years of cancer data to identify and account for the population who have previously been diagnosed with cancer.
Are the AdjCom and RUCM incidence risk measures reliable?
Comparisons between AdjCom and the ‘best estimate’ of cancer incidence risk are provided in Attachment A. Where the two values are suitably close, AdjCom and RUCM risk are considered acceptable proxies that are accurate enough to approximate cancer incidence risk.
For most cancers, the proxy and the best estimate are usually quite close. However, for the group ‘all cancers combined’, the proxy measure of risk is around 10 percentage points higher than the best estimate. The all cancers combined incidence risk using the proxy is over-stated to the extent that it is not considered suitable.
Is the all cancers combined mortality risk time series available?
All cancers combined mortality risk is available. The complexities surrounding cancer incidence risk do not apply to cancer mortality risk. This is because death occurs only once, so the issue of multiple diagnoses and recognising the first occurrence does not apply to mortality risk.
What information is available to inform all cancers combined risk?
The ‘best estimate’ of all cancers combined incidence risk as presented in Attachment A can be used as the most recent estimate of risk. The ‘best estimate’ is only produced for the most recent year for which all states and territories have provided data. A time-series is not available due to comparability issues across time. For example, 2015 will have over 30 years of data from which to identify if a person has been diagnosed with cancer before, whereas the first year of data, 1982, would have no earlier years to identify if a person has been diagnosed with cancer before.
Prior to the 2020 release of cancer risk data, AIHW measured risk of diagnosis using the RUCM method. However, the previous method measured this risk using ‘cases diagnosed in the year’ while the replacement method of RUCM measures this risk using ‘people diagnosed in the year’. The change to measuring risk of people being diagnosed is closer to the recommended measure of measuring risk of people who were diagnosed for the first time. Attachment B quantifies the impact of changing measurement from cases to people for 2015.
Note that the RUCM method of measuring the risk of death from cancer has not changed from previous publications.
Lifetime risk of diagnosis and risk of diagnosis before age 85 for persons, 2015
Comparison of risk adjusted for competing mortality estimates based on:
- people diagnosed for the first time ever (Method A)
- people diagnosed in a year (Method B)
* the first time ever only factors if a person has been diagnosed previously and since 1982; data on earlier years is not available
| Cancer site/type | Lifetime risk of diagnosis Method A % | Lifetime risk of diagnosis Method A 1 in ... | Lifetime risk of diagnosis Method B % | Lifetime risk of diagnosis Method B 1 in ... | Risk of diagnosis before age 85 Method A % | Risk of diagnosis before age 85 Method A 1 in ... | Risk of diagnosis before age 85 Method B % | Risk of diagnosis before age 85 Method B 1 in ... |
|---|---|---|---|---|---|---|---|---|
Acute lymphoblastic leukaemia (ALL) | 0.1492 | 670 | 0.1492 | 670 | 0.1414 | 707 | 0.1414 | 707 |
Acute myeloid leukaemia (AML) | 0.4826 | 207 | 0.4826 | 207 | 0.3842 | 260 | 0.3842 | 260 |
All blood cancers combined | 6.9784 | 14 | 7.0902 | 14 | 5.5780 | 18 | 5.6781 | 18 |
All cancers combined | 50.7679 | 2 | 60.4152 | 2 | 43.2378 | 2 | 50.5515 | 2 |
Anal cancer | 0.2056 | 486 | 0.2056 | 486 | 0.1824 | 548 | 0.1824 | 548 |
Bladder cancer | 1.5179 | 66 | 1.5204 | 66 | 1.0836 | 92 | 1.0846 | 92 |
Bone cancer | 0.1051 | 951 | 0.1051 | 951 | 0.0966 | 1,036 | 0.0966 | 1,036 |
Brain cancer | 0.7492 | 133 | 0.7492 | 133 | 0.6738 | 148 | 0.6738 | 148 |
Breast cancer | 13.9630 | 7 | 13.9794 | 7 | 12.5910 | 8 | 12.6060 | 8 |
Cancer of other and ill-defined digestive organs | 0.1537 | 650 | 0.1537 | 650 | 0.0792 | 1,262 | 0.0792 | 1,262 |
Cancer of other soft tissue | 0.3402 | 294 | 0.3402 | 294 | 0.2881 | 347 | 0.2881 | 347 |
Cancer of small intestine | 0.2561 | 391 | 0.2561 | 391 | 0.2175 | 460 | 0.2175 | 460 |
Cancer of the gallbladder and extrahepatic bile ducts | 0.5128 | 195 | 0.5128 | 195 | 0.3793 | 264 | 0.3793 | 264 |
Cancer of the salivary glands | 0.1552 | 644 | 0.1552 | 644 | 0.1218 | 821 | 0.1218 | 821 |
Cancer of unknown primary site | 1.4443 | 69 | 1.4450 | 69 | 0.8589 | 116 | 0.8596 | 116 |
Cervical cancer | 0.5805 | 172 | 0.5818 | 172 | 0.5545 | 180 | 0.5557 | 180 |
Chronic lymphocytic leukaemia (CLL) | 0.8249 | 121 | 0.8249 | 121 | 0.6783 | 147 | 0.6783 | 147 |
Chronic myeloid leukaemia (CML) | 0.1368 | 731 | 0.1368 | 731 | 0.1127 | 887 | 0.1127 | 887 |
Colon cancer | 5.3789 | 19 | 5.3863 | 19 | 4.2091 | 24 | 4.2132 | 24 |
Colorectal cancer | 7.5169 | 13 | 7.6324 | 13 | 6.0378 | 17 | 6.1236 | 16 |
Eye cancer | 0.1575 | 635 | 0.1575 | 635 | 0.1348 | 742 | 0.1348 | 742 |
Gynaecological cancers | 4.7001 | 21 | 4.7502 | 21 | 4.1486 | 24 | 4.1853 | 24 |
Head and neck cancer (excluding lip) | 1.5594 | 64 | 1.6196 | 62 | 1.3639 | 73 | 1.4184 | 71 |
Head and neck cancer (with lip) | 1.9785 | 51 | 2.0507 | 49 | 1.7096 | 58 | 1.7737 | 56 |
Hodgkin lymphoma | 0.2423 | 413 | 0.2423 | 413 | 0.2244 | 446 | 0.2244 | 446 |
Hypopharyngeal cancer | 0.0827 | 1,209 | 0.0827 | 1,209 | 0.0739 | 1,354 | 0.0739 | 1,354 |
Immunoproliferative cancers | 0.1363 | 734 | 0.1363 | 734 | 0.1086 | 921 | 0.1086 | 921 |
Kaposi sarcoma | 0.0239 | 4,188 | 0.0239 | 4,188 | 0.0191 | 5,232 | 0.0191 | 5,232 |
Kidney cancer | 1.5171 | 66 | 1.5171 | 66 | 1.3577 | 74 | 1.3577 | 74 |
Laryngeal cancer | 0.2821 | 355 | 0.2821 | 355 | 0.2521 | 397 | 0.2521 | 397 |
Leukaemia | 1.8992 | 53 | 1.9088 | 52 | 1.5405 | 65 | 1.5492 | 65 |
Lip cancer | 0.4311 | 232 | 0.4311 | 232 | 0.3553 | 281 | 0.3553 | 281 |
Liver cancer | 0.9608 | 104 | 0.9611 | 104 | 0.8270 | 121 | 0.8273 | 121 |
Lung cancer | 5.8633 | 17 | 5.9000 | 17 | 4.8731 | 21 | 4.9077 | 20 |
Lymphoma | 2.6273 | 38 | 2.6425 | 38 | 2.2005 | 45 | 2.2156 | 45 |
Melanoma of the skin | 6.1037 | 16 | 6.1086 | 16 | 5.1930 | 19 | 5.1978 | 19 |
Mesothelioma | 0.4134 | 242 | 0.4134 | 242 | 0.3074 | 325 | 0.3074 | 325 |
Mouth cancer | 0.2841 | 352 | 0.2841 | 352 | 0.2295 | 436 | 0.2295 | 436 |
Multiple myeloma | 0.9315 | 107 | 0.9315 | 107 | 0.7660 | 131 | 0.7660 | 131 |
Myelodysplastic syndromes | 0.8336 | 120 | 0.8336 | 120 | 0.5236 | 191 | 0.5236 | 191 |
Nasal cavity, middle ear and sinuses cancer | 0.0979 | 1,021 | 0.0979 | 1,021 | 0.0771 | 1,297 | 0.0771 | 1,297 |
Nasopharyngeal cancer | 0.0498 | 2,010 | 0.0498 | 2,010 | 0.0488 | 2,050 | 0.0488 | 2,050 |
Neuroendocrine tumours | 1.7932 | 56 | 1.8010 | 56 | 1.5412 | 65 | 1.5473 | 65 |
Non-Hodgkin lymphoma | 2.3953 | 42 | 2.4010 | 42 | 1.9864 | 50 | 1.9921 | 50 |
Non-melanoma skin cancer (rare types) | 0.5461 | 183 | 0.5511 | 181 | 0.3592 | 278 | 0.3635 | 275 |
Oesophageal cancer | 0.7208 | 139 | 0.7215 | 139 | 0.5733 | 174 | 0.5740 | 174 |
Oropharyngeal cancer | 0.2661 | 376 | 0.2661 | 376 | 0.2560 | 391 | 0.2560 | 391 |
Ovarian cancer | 1.2121 | 83 | 1.2121 | 83 | 1.0084 | 99 | 1.0084 | 99 |
Pancreatic cancer | 1.7829 | 56 | 1.7829 | 56 | 1.3386 | 75 | 1.3386 | 75 |
Penile cancer | 0.1017 | 983 | 0.1017 | 983 | 0.0852 | 1,174 | 0.0852 | 1,174 |
Peritoneal cancer | 0.0968 | 1,033 | 0.0971 | 1,030 | 0.0835 | 1,197 | 0.0839 | 1,192 |
Prostate cancer | 17.4717 | 6 | 17.4732 | 6 | 15.6084 | 6 | 15.6099 | 6 |
Rectal cancer | 2.3007 | 43 | 2.3017 | 43 | 1.9581 | 51 | 1.9591 | 51 |
Soft tissue sarcoma | 0.6944 | 144 | 0.6970 | 143 | 0.5882 | 170 | 0.5908 | 169 |
Stomach cancer | 1.0694 | 94 | 1.0702 | 93 | 0.8354 | 120 | 0.8362 | 120 |
Testicular cancer | 0.5093 | 196 | 0.5093 | 196 | 0.5078 | 197 | 0.5078 | 197 |
Thyroid cancer | 1.0519 | 95 | 1.0548 | 95 | 1.0204 | 98 | 1.0232 | 98 |
Tongue cancer | 0.3795 | 264 | 0.3795 | 264 | 0.3428 | 292 | 0.3428 | 292 |
Uterine cancer | 2.3069 | 43 | 2.3089 | 43 | 2.0998 | 48 | 2.1018 | 48 |
Vaginal cancer | 0.0792 | 1,263 | 0.0792 | 1,263 | 0.0582 | 1,717 | 0.0582 | 1,717 |
Vulvar cancer | 0.3492 | 286 | 0.3492 | 286 | 0.2657 | 376 | 0.2657 | 376 |
Notes:
- Risk estimates for sex-specific cancers are presented for the relevant sex e.g. the risk of being diagnosed with prostate cancer is presented as the risk of being diagnosed in males.
- Risk estimates for breast cancer are presented as the risk of diagnosis in females.
Source: AIHW 2016 Australian Cancer Database
Risk of diagnosis before age 75 and age 85, persons, 2015
Comparison of risk unadjusted for competing mortality estimates based on:
- cases diagnosed in a year (Method A)
- people diagnosed in a year (Method B)
| Cancer site/type | Diagnosis before age 75 Method A % | Diagnosis before age 75 Method A 1 in ... | Diagnosis before age 75 Method B % | Diagnosis before age 75 Method B 1 in ... | Diagnosis before age 85 Method A % | Diagnosis before age 85 Method A 1 in ... | Diagnosis before age 85 Method B % | Diagnosis before age 85 Method B 1 in ... |
|---|---|---|---|---|---|---|---|---|
Acute lymphoblastic leukaemia (ALL) | 0.1292 | 774 | 0.1292 | 774 | 0.1532 | 653 | 0.1532 | 653 |
Acute myeloid leukaemia (AML) | 0.2468 | 405 | 0.2468 | 405 | 0.4831 | 207 | 0.4831 | 207 |
All blood cancers combined | 3.7598 | 27 | 3.7512 | 27 | 6.9097 | 14 | 6.8820 | 15 |
All cancers combined | 31.6111 | 3 | 31.1792 | 3 | 47.0215 | 2 | 46.3565 | 2 |
Anal cancer | 0.1469 | 681 | 0.1469 | 681 | 0.2176 | 459 | 0.2176 | 459 |
Bladder cancer | 0.5817 | 172 | 0.5817 | 172 | 1.4279 | 70 | 1.4279 | 70 |
Bone cancer | 0.0827 | 1,210 | 0.0827 | 1,210 | 0.1097 | 912 | 0.1097 | 912 |
Brain cancer | 0.5438 | 184 | 0.5438 | 184 | 0.7925 | 126 | 0.7925 | 126 |
Breast cancer | 10.2107 | 10 | 10.2101 | 10 | 13.2263 | 8 | 13.2258 | 8 |
Cancer of other and ill-defined digestive organs | 0.0403 | 2,478 | 0.0403 | 2,478 | 0.1055 | 948 | 0.1055 | 948 |
Cancer of other soft tissue | 0.2182 | 458 | 0.2182 | 458 | 0.3463 | 289 | 0.3463 | 289 |
Cancer of small intestine | 0.1591 | 628 | 0.1587 | 630 | 0.2652 | 377 | 0.2648 | 378 |
Cancer of the gallbladder and extrahepatic bile ducts | 0.2208 | 453 | 0.2205 | 454 | 0.4935 | 203 | 0.4932 | 203 |
Cancer of the salivary glands | 0.0867 | 1,154 | 0.0867 | 1,154 | 0.1496 | 669 | 0.1496 | 669 |
Cancer of unknown primary site | 0.4514 | 222 | 0.4514 | 222 | 1.1344 | 88 | 1.1344 | 88 |
Cervical cancer | 0.4890 | 204 | 0.4878 | 205 | 0.6040 | 166 | 0.6027 | 166 |
Chronic lymphocytic leukaemia (CLL) | 0.4671 | 214 | 0.4671 | 214 | 0.8525 | 117 | 0.8525 | 117 |
Chronic myeloid leukaemia (CML) | 0.0940 | 1,064 | 0.0940 | 1,064 | 0.1325 | 755 | 0.1325 | 755 |
Colon cancer | 2.5473 | 39 | 2.5391 | 39 | 5.2992 | 19 | 5.2846 | 19 |
Colorectal cancer | 3.9495 | 25 | 3.9167 | 26 | 7.5604 | 13 | 7.4842 | 13 |
Eye cancer | 0.1040 | 961 | 0.1040 | 961 | 0.1641 | 609 | 0.1641 | 609 |
Gynaecological cancers | 3.2728 | 31 | 3.2380 | 31 | 4.7229 | 21 | 4.6777 | 21 |
Head and neck cancer (excluding lip) | 1.1712 | 85 | 1.1657 | 86 | 1.6840 | 59 | 1.6770 | 60 |
Head and neck cancer (with lip) | 1.4484 | 69 | 1.4429 | 69 | 2.1027 | 48 | 2.0957 | 48 |
Hodgkin lymphoma | 0.1972 | 507 | 0.1972 | 507 | 0.2500 | 400 | 0.2500 | 400 |
Hypopharyngeal cancer | 0.0569 | 1,759 | 0.0569 | 1,759 | 0.0897 | 1,115 | 0.0897 | 1,115 |
Immunoproliferative cancers | 0.0733 | 1,365 | 0.0733 | 1,365 | 0.1360 | 735 | 0.1360 | 735 |
Kaposi sarcoma | 0.0144 | 6,942 | 0.0144 | 6,942 | 0.0238 | 4,202 | 0.0238 | 4,202 |
Kidney cancer | 1.0910 | 92 | 1.0903 | 92 | 1.6202 | 62 | 1.6195 | 62 |
Laryngeal cancer | 0.1932 | 518 | 0.1928 | 519 | 0.3112 | 321 | 0.3101 | 323 |
Leukaemia | 1.0659 | 94 | 1.0643 | 94 | 1.9144 | 52 | 1.9106 | 52 |
Lip cancer | 0.2805 | 357 | 0.2805 | 357 | 0.4259 | 235 | 0.4259 | 235 |
Liver cancer | 0.6056 | 165 | 0.6056 | 165 | 1.0117 | 99 | 1.0117 | 99 |
Lung cancer | 3.1713 | 32 | 3.1580 | 32 | 6.1065 | 16 | 6.0845 | 16 |
Lymphoma | 1.5740 | 64 | 1.5726 | 64 | 2.7017 | 37 | 2.7003 | 37 |
Melanoma of the skin | 3.9255 | 25 | 3.9255 | 25 | 6.0996 | 16 | 6.0996 | 16 |
Mesothelioma | 0.1625 | 616 | 0.1625 | 616 | 0.4081 | 245 | 0.4081 | 245 |
Mouth cancer | 0.1775 | 564 | 0.1771 | 565 | 0.2814 | 355 | 0.2811 | 356 |
Multiple myeloma | 0.5055 | 198 | 0.5055 | 198 | 0.9699 | 103 | 0.9699 | 103 |
Myelodysplastic syndromes | 0.2225 | 449 | 0.2225 | 449 | 0.7120 | 140 | 0.7120 | 140 |
Nasal cavity, middle ear and sinuses cancer | 0.0616 | 1,624 | 0.0616 | 1,624 | 0.0916 | 1,092 | 0.0916 | 1,092 |
Nasopharyngeal cancer | 0.0436 | 2,294 | 0.0436 | 2,294 | 0.0555 | 1,802 | 0.0555 | 1,802 |
Neuroendocrine tumours | 1.1545 | 87 | 1.1515 | 87 | 1.8807 | 53 | 1.8759 | 53 |
Non-Hodgkin lymphoma | 1.3796 | 72 | 1.3791 | 73 | 2.4579 | 41 | 2.4574 | 41 |
Non-melanoma skin cancer (rare types) | 0.1886 | 530 | 0.1883 | 531 | 0.4796 | 209 | 0.4792 | 209 |
Oesophageal cancer | 0.3762 | 266 | 0.3754 | 266 | 0.7307 | 137 | 0.7298 | 137 |
Oropharyngeal cancer | 0.2392 | 418 | 0.2392 | 418 | 0.2914 | 343 | 0.2914 | 343 |
Ovarian cancer | 0.7546 | 133 | 0.7529 | 133 | 1.1633 | 86 | 1.1616 | 86 |
Pancreatic cancer | 0.8343 | 120 | 0.8338 | 120 | 1.7042 | 59 | 1.7037 | 59 |
Penile cancer | 0.0574 | 1,742 | 0.0574 | 1,742 | 0.1154 | 867 | 0.1154 | 867 |
Peritoneal cancer | 0.0592 | 1,690 | 0.0592 | 1,690 | 0.1038 | 963 | 0.1038 | 963 |
Prostate cancer | 12.0198 | 8 | 12.0198 | 8 | 18.2445 | 5 | 18.2445 | 5 |
Rectal cancer | 1.4389 | 69 | 1.4370 | 70 | 2.3877 | 42 | 2.3858 | 42 |
Soft tissue sarcoma | 0.4343 | 230 | 0.4343 | 230 | 0.7162 | 140 | 0.7154 | 140 |
Stomach cancer | 0.5361 | 187 | 0.5351 | 187 | 1.0632 | 94 | 1.0622 | 94 |
Testicular cancer | 0.5165 | 194 | 0.5165 | 194 | 0.5249 | 191 | 0.5249 | 191 |
Thyroid cancer | 0.9721 | 103 | 0.9603 | 104 | 1.1448 | 87 | 1.1322 | 88 |
Tongue cancer | 0.2999 | 333 | 0.2999 | 333 | 0.3998 | 250 | 0.3998 | 250 |
Uterine cancer | 1.6707 | 60 | 1.6701 | 60 | 2.3797 | 42 | 2.3771 | 42 |
Vaginal cancer | 0.0429 | 2,328 | 0.0429 | 2,328 | 0.0674 | 1,483 | 0.0674 | 1,483 |
Vulvar cancer | 0.1747 | 572 | 0.1747 | 572 | 0.3159 | 317 | 0.3159 | 317 |
Notes:
- Risk estimates for sex-specific cancers are presented for the relevant sex e.g. the risk of being diagnosed with prostate cancer is presented as the risk of being diagnosed in males.
- Risk estimates for breast cancer are presented as the risk of diagnosis in females.
Source: AIHW 2016 Australian Cancer Database


