All arthritis
Page highlights
Arthritis is an umbrella term for a wide range of inflammatory conditions affecting the joints. Osteoarthritis, rheumatoid arthritis and gout are common types of arthritis.
An estimated 3.6 million (15%) people in Australia reported having arthritis (excluding gout) in 2017–18.
- People with arthritis had around double the rates of ‘fair’ to ‘poor’ health (31%), ‘moderate’ to ‘very severe’ pain (56%), and ‘high’ to ‘very high’ psychological distress (22%) compared with those without the condition.
- In 2023, musculoskeletal conditions were responsible for 13% of the total burden of disease (approximately 723,000 disability-adjusted life years (DALY)).
- In 2020–21, health expenditure for osteoarthritis and rheumatoid arthritis were estimated to be $4.3 billion and $966.1 million respectively.
Treatment and management of arthritis
In 2021–22, osteoarthritis was the most common type of arthritis hospitalisation and as a principal diagnosis accounted for 2.5% of all hospitalisations.
75% of people aged 45 and over with arthritis had at least one other chronic condition in 2017–18, back problems being the most common at 36%.
What is arthritis?
Arthritis is an umbrella term for a wide range of inflammatory conditions affecting the joints. This often results in pain, stiffness, swelling and redness in affected joints. Age, overweight and obesity, injury and genetic factors increase the risk of developing arthritis. Osteoarthritis, rheumatoid arthritis and gout are common types of arthritis.
How common is arthritis?
Arthritis – including osteoarthritis, rheumatoid arthritis and ‘other type and unknown’ – affected an estimated 3.6 million (15%) people in Australia, according to the 2017–18 Australian Bureau of Statistics (ABS) National Health Survey (NHS) (ABS 2018).
Note: This does not include gout. For more information, see gout.
Osteoarthritis and rheumatoid arthritis are the most common forms of arthritis:
- osteoarthritis is a chronic condition characterised by the deterioration of the cartilage that overlies the ends of bones in joints. Approximately 2.2 million people in Australia (9.3%) had osteoarthritis, affecting 12% of females and 6.8% of males) in 2017–18 (ABS 2018)
- rheumatoid arthritis is a systemic autoimmune disease where the body’s immune system attacks its own tissues. Approximately 456,000 people in Australia (1.9%) had rheumatoid arthritis, affecting 2.3% of females and 1.5% of males in 2017–18 (ABS 2018) (Figure 1).
Figure 1: Prevalence of self-reported arthritis in Australia, by arthritis type and sex, 2017–18
Note: Refers to people who self-reported that they were diagnosed by a doctor or nurse as having arthritis (current and long term) and also people who self-reported having arthritis.
Source: ABS 2018 (All arthritis 2023 Supplementary data table 1.1).
Prevalence in Aboriginal and Torres Strait Islander (First Nations) people
The Australian Institute of Health and Welfare (AIHW) uses ‘First Nations people’ to refer to Aboriginal and/or Torres Strait Islander people in this report.
According to self-reported data from the ABS National Aboriginal and Torres Strait Islander Health Survey (NATSIHS), in 2018–19, about 85,600 (11%) of First Nations people reported having arthritis – including about 8,800 who lived in remote areas (5.9% of the remote First Nations population) (ABS 2019a).
After adjusting for differences in age structures, arthritis prevalence was:
- more common in First Nations females compared with First Nations males (19% and 13%, respectively)
- slightly higher for First Nations people compared with non-Indigenous people (17% and 13%, respectively) (Figure 2).
Figure 2: Prevalence of arthritis by Indigenous status and sex, 2018–19
Note: Age-standardised to the Australian population as at 30 June 2001.
Source: ABS 2019a (All arthritis 2023 Supplementary data table 1.2)
Impact of arthritis
Arthritis can have a profound impact on a person’s quality of life and wellbeing due to acute and chronic pain, physical limitations, management of the condition and mental health impacts. This can often result in withdrawal from social, community and occupational activities (Briggs et al. 2016).
How does arthritis affect quality of life?
Although arthritis affects people of all ages, its prevalence increases sharply from the age of 45 years. It can have a significant impact on a person’s physical health, due to the pain and physical limitations associated with the disease.
Arthritis can also affect mental wellbeing. The chronic and progressive symptoms and the management of the condition can cause distress, which may lead to mental health issues such as anxiety or depression (Sharma et al. 2016).
According to the 2017–18 NHS, people aged 45 and over with arthritis were:
- 1.9 times as likely to report having ‘fair’ to ‘poor’ health compared with those without arthritis (31% and 16%, respectively) (Figure 3)
- 2.3 times as likely as people without arthritis to experience ‘moderate’ to ‘very severe’ pain in the last 4 weeks (56% and 24%, respectively) (Figure 4)
- 2.2 times as likely as those without arthritis to experience high or very high levels of psychological distress (22% and 10%, respectively) (Figure 5).
In addition, 45% of people aged 45 and over with arthritis described their pain as having a ‘moderate’ to ‘extreme’ interference with their normal work during the last 4 weeks (ABS 2019b).
Figure 3: Self-assessed health of people aged 45 and over with and without arthritis, 2017–18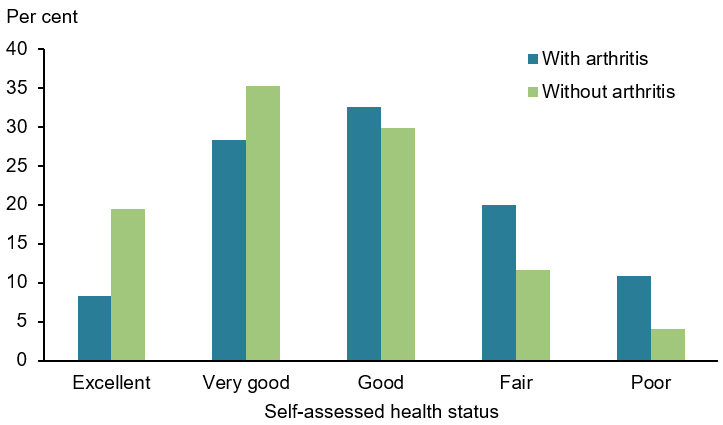
Note: Age-standardised to the 2001 Australian population.
Source: AIHW analysis of ABS 2019b (All arthritis 2023 Supplementary data table 2.1).
Figure 4: Pain(a) experienced by people aged 45 and over with and without arthritis, 2017–18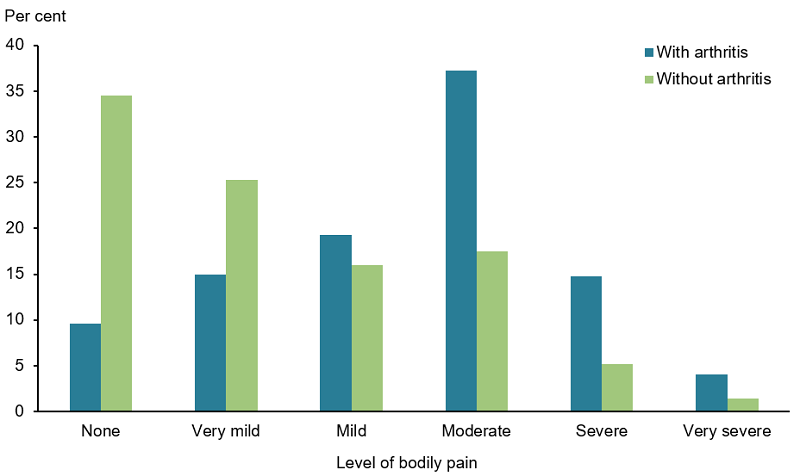
(a) Bodily pain experienced in the 4 weeks prior to interview.
Note: Age-standardised to the 2001 Australian population.
Source: AIHW analysis of ABS 2019b (All arthritis 2023 Supplementary data table 2.2).
Figure 5: Psychological distress(a) experienced by people aged 45 and over with and without arthritis, 2017–18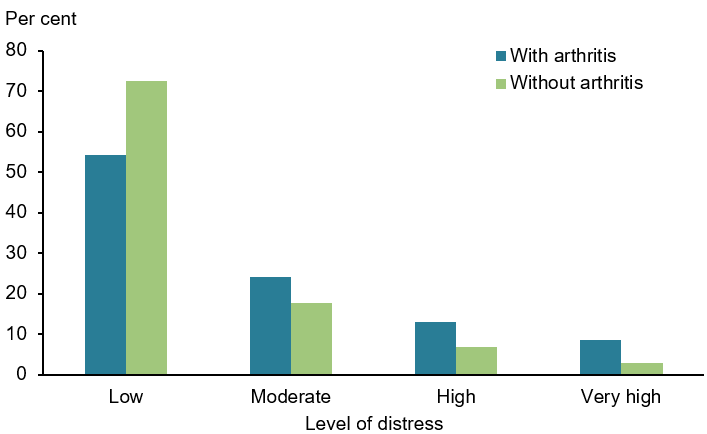
(a) Psychological distress is measured using the Kessler Psychological Distress Scale (K10), which involves 10 questions about negative emotional states experienced in the previous 4 weeks. The scores are grouped into Low: K10 score 10–15, Moderate: 16–21, High: 22–29, Very high: 30–50.
Note: Age-standardised to the 2001 Australian population.
Source: AIHW analysis of ABS 2019b (All arthritis 2023 Supplementary data table 2.4).
Burden of disease
What is burden of disease?
Burden of disease is measured using the summary metric of disability-adjusted life years (DALY, also known as the total burden). One DALY is one year of healthy life lost to disease and injury. DALY caused by living in poor health (non-fatal burden) are the ‘years lived with disability’ (YLD). DALY caused by premature death (fatal burden) are the ‘years of life lost’ (YLL) and are measured against an ideal life expectancy. DALY allows the impact of premature deaths and living with health impacts from disease or injury to be compared and reported in a consistent manner (AIHW 2022).
Common forms of arthritis (osteoarthritis, rheumatoid arthritis and gout) are large contributors to illness, pain and disability in Australia. Based on data from the Australian Burden of Disease Study 2023, musculoskeletal conditions were responsible for 13% of the total burden of disease (approximately 723,000 disability-adjusted life years (DALY)). Of this proportion:
- osteoarthritis contributed 20% of disease burden
- rheumatoid arthritis contributed 16%
- gout contributed 0.7%.
The remaining burden was attributed to ‘other musculoskeletal conditions’ (30%) and ‘back pain and problems’ (34%) (AIHW 2023a) (Figure 6).
For more information, see osteoarthritis, rheumatoid arthritis and gout.
Figure 6: Musculoskeletal conditions burden (DALY), by disease, 2023
Source: AIHW 2023a.
Health system expenditure
Arthritis significantly impacts the Australian economy. Increased health care costs and higher use of health care services (for example, general practitioners, specialists, allied health and pharmaceuticals) required to treat and manage arthritis represent direct financial costs to the health care system.
There are also indirect costs associated with arthritis and/or musculoskeletal conditions and comorbidities, such as productivity losses, disability support pensions and other welfare payments, early retirement and carer costs (AIHW 2014; Arthritis Australia 2014).
In 2020–21, health expenditure for arthritis was estimated to be:
- $4.3 billion for osteoarthritis, representing 2.9% of total disease expenditure
- $966.1 million for rheumatoid arthritis, representing 0.6% of total disease expenditure (AIHW 2023b).
For more information, see Disease expenditure in Australia 2020–21.
Treatment and management of arthritis
Primary health care
At present, there is no cure for arthritis, with treatment aiming to manage symptoms and maximise quality of life. Arthritis-related conditions are predominantly managed in primary health care settings by a range of health professionals. Treatment involves a combination of self-management (such as diet and exercise), education on living with the condition, physiotherapy, medication (for pain and inflammation), and referral to specialist care where necessary (WHO 2019).
Until 2017, the Bettering the Evaluation and Care of Health (BEACH) survey was the most detailed source of data about general practice activity in Australia (Britt et al. 2016). Based on BEACH survey data, arthritis was managed at an estimated 3.5% of general practice visits in 2015–16 (Britt et al. 2016).
It is worth noting that there is currently no nationally consistent primary health care data collection to monitor provision of care by GPs. See General practice, allied health and other primary care services.
Medications
Medication is primarily used to manage symptoms of pain, inflammation and improve functioning and quality of life among people with arthritis. Medications can range from general over-the-counter analgesics (painkillers) to highly specialised medications and vary depending on the type and severity of the condition.
Hospitalisations for arthritis
Osteoarthritis was the most common type of arthritis hospitalisation in 2021–22, and as a principal diagnosis accounted for 2.1% of all hospitalisations. Rheumatoid arthritis and gout accounted for 0.1% each.
Surgery
Joint replacement surgery may be required for those with severe arthritic conditions who are unresponsive to medication and exercise (RACGP 2018). These procedures restore joint function, help relieve pain and improve quality of life of the affected person. Osteoarthritis is the most common condition leading to hip and knee replacement surgery in Australia (AOANJRR 2019).
For more information on these conditions, see the osteoarthritis, rheumatoid arthritis, juvenile arthritis and gout pages.
Comorbidities of arthritis
People with arthritis often have other chronic diseases and long-term conditions (comorbidities).
In 2017–18:
- 75% people aged 45 and over with arthritis had at least one other chronic condition
- back problems were the most common comorbidity (36%), followed by mental and behavioural conditions (30%) and asthma (18%) (ABS 2019b) (Figure 7).
Figure 7: Prevalence of chronic conditions in people aged 45 and over with and without arthritis, 2017–18
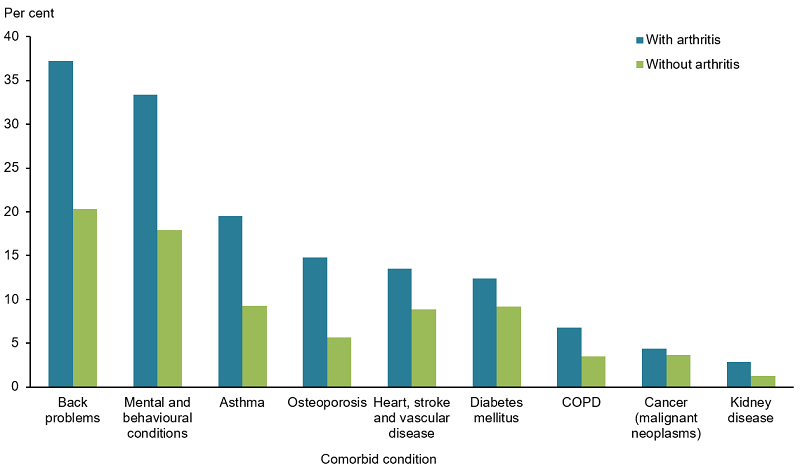
Notes
- Age-standardised to the 2001 Australian population.
- Proportions do not total 100% as one person may have more than one additional diagnosis.
Source: AIHW analysis of ABS 2019b (All arthritis 2023 Supplementary data table 2.5).
ABS (Australian Bureau of Statistics) (2018) National Health Survey: First results, 2017–18. ABS cat. no. 4364.0.55.001, AIHW, Australian Government, accessed 28 April 2021.
ABS (2019a) National Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, 2018–19. ABS cat. no. 4715.0, ABS, Australian Government, accessed 28 April 2021.
ABS (2019b) Microdata: National Health Survey, 2017–18, AIHW analysis detailed microdata, accessed 28 April 2021.
AIHW (Australian Institute of Health and Welfare) (2014) Health-care expenditure on arthritis and other musculoskeletal conditions: 2008–09, AIHW, Australian Government, accessed 28 April 2021.
AIHW (2022) Australian Burden of Disease Study 2022, AIHW, Australian Government, accessed 06 June 2023. doi:10.25816/e2v0-gp02, accessed 28 April 2021.
AIHW (2023a) Australian Burden of Disease Study 2023, AIHW, Australian Government, accessed 14 December 2023.
AIHW (2023b) Disease expenditure in Australia 2020–21, AIHW, Australian Government, accessed 14 December 2023.
AOANJRR (Australian Orthopaedic Association National Joint Replacement Registry) (2019) Annual report 2019: Hip, knee and shoulder arthroplasty. AOA website, accessed 28 April 2021.
Arthritis Australia (2014) Time to move: rheumatoid arthritis, a national strategy to reduce a costly burden, Arthritis Australia website, accessed 28 April 2021.
Briggs AM, Cross MJ, Hoy DG, Sànchez-Riera L, Blyth FM, Woolf AD and March LM (2016) ‘Musculoskeletal Health Conditions Represent a Global Threat to Healthy Aging: A Report for the 2015 World Health Organization World Report on Ageing and Health’, Gerontologist 56:S243-S255.
Britt H, Miller GC, Henderson J, Bayram C, Harrison C, Valenti L, Pan Y, Charles J, Pollack AJ, Wong C and Gordon J (2016) ‘General practice activity in Australia 2015–16’, General practice series no. 40. Sydney University Press.
RACGP (The Royal Australian College of General Practitioners) (2018) Guideline for the management of knee and hip osteoarthritis, RACGP website, accessed 28 April 2021.
Sharma A, Kudesia P, Shi Q and Gandhi R (2016) ‘Anxiety and depression in patients with osteoarthritis: impact and management challenges’, Open Access Rheumatology: Research and Reviews, 8:103–113.
WHO (World Health Organization) (2019) Musculoskeletal conditions: fact sheet, WHO website, accessed 3 June 2020.


