General practice, allied health and other primary care services
Citation
AIHW
Australian Institute of Health and Welfare (2024) General practice, allied health and other primary care services, AIHW, Australian Government, accessed 27 July 2024.
APA
Australian Institute of Health and Welfare. (2024). General practice, allied health and other primary care services. Retrieved from https://www.aihw.gov.au/reports/primary-health-care/general-practice-allied-health-primary-care
MLA
General practice, allied health and other primary care services. Australian Institute of Health and Welfare, 07 March 2024, https://www.aihw.gov.au/reports/primary-health-care/general-practice-allied-health-primary-care
Vancouver
Australian Institute of Health and Welfare. General practice, allied health and other primary care services [Internet]. Canberra: Australian Institute of Health and Welfare, 2024 [cited 2024 Jul. 27]. Available from: https://www.aihw.gov.au/reports/primary-health-care/general-practice-allied-health-primary-care
Harvard
Australian Institute of Health and Welfare (AIHW) 2024, General practice, allied health and other primary care services, viewed 27 July 2024, https://www.aihw.gov.au/reports/primary-health-care/general-practice-allied-health-primary-care
Get citations as an Endnote file: Endnote
What is primary care?
Primary health care is often the first contact a person has with the health system and can be delivered in various settings, by a range of providers. It may be provided by general practitioners (GPs) within general practice or in an aged care or community setting, by public or private service providers. Nursing care, midwifery, pharmacy, dentistry, Aboriginal health services, and allied health care are also examples of primary care services.
Comprehensive data on primary care are limited, but robust existing sources include claims information relating to Medicare-subsidised health services, patient-reported experiences of primary care and primary care expenditure.
Information on this page comes from the:
- Department of Health and Aged Care Medicare Benefits Schedule (MBS) claims data collection
- Australian Bureau of Statistics Patient Experience Survey
- AIHW Health and Welfare Expenditure Database.
Primary care service use
In 2022–23, there were around 197 million Medicare-subsidised primary care services in Australia, up from around 185 million in 2018–19. This includes:
- 166 million GP attendances, an increase of 5.0% from 2018–19 (158 million)
- 27 million allied health attendances, an increase of 11% from 2018–19 (24 million)
- 4.3 million services provided by nurses and Aboriginal health workers, an increase of 21% from 2018–19 (3.5 million) (AIHW 2020b; AIHW 2024).
Trends over time
Between 2018–19 and 2022–23, the proportion of people who received a primary health care service fluctuated and was likely impacted by the COVID-19 pandemic (Figure 1).
There was a peak in the proportion of those who received a service from a nurse and Aboriginal health worker (8.3%) in 2020–21, but a low in GP attendances (85%). For more information about how COVID-19 may have impacted the data reported in this report, see Primary care services and the effects of COVID-19.
Figure 1: Proportion of people who received a primary care service, 2018–19 to 2022–23
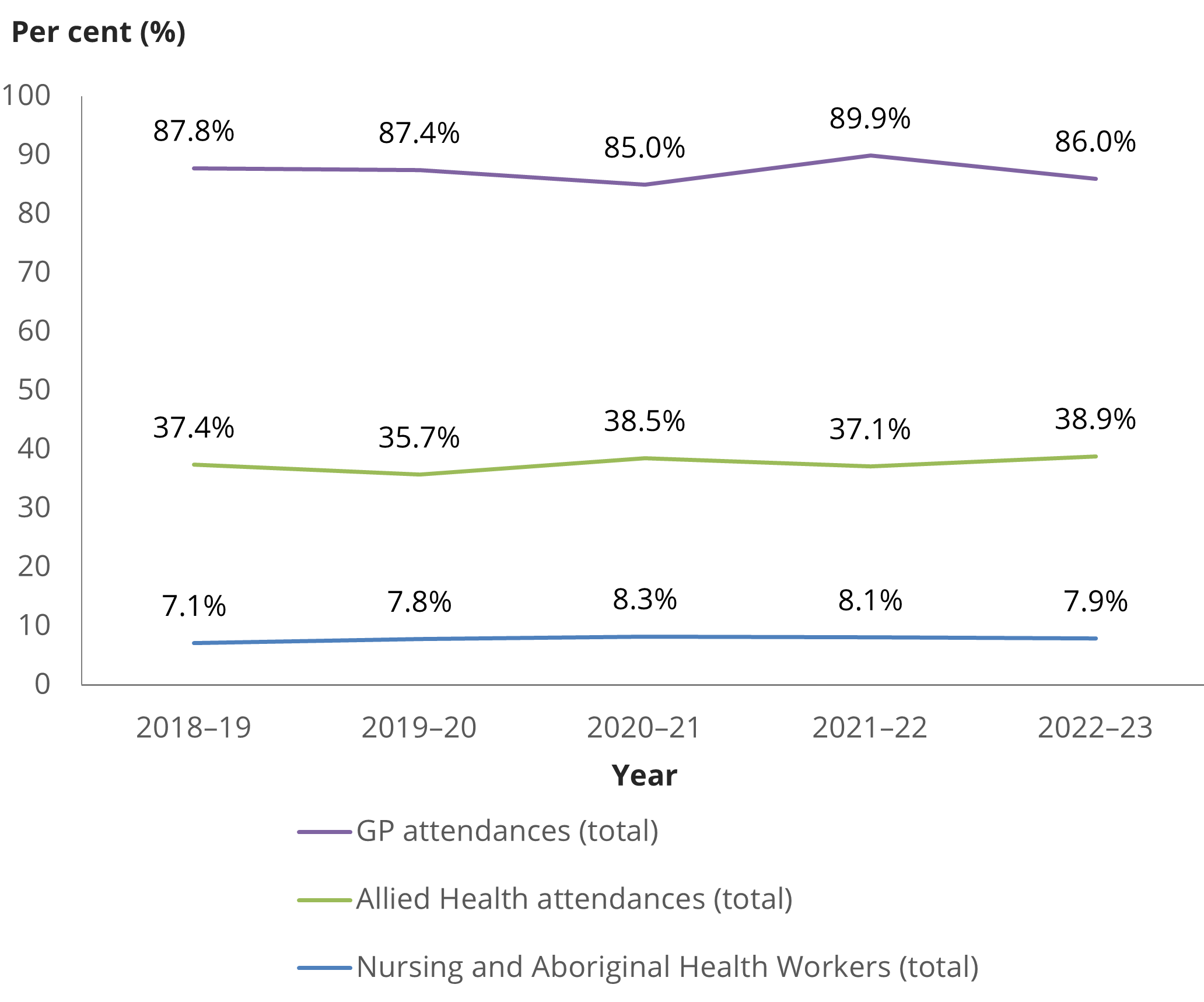
Chart: AIHW. Source: AIHW analysis of Department of Health and Aged Care Medicare Benefits Schedule (MBS) claims data, 2018–19, 2019–20, 2020–21, 2021–22, 2022–23
Between 2018–19 and 2022–23, the rate (per 100 people) of primary health care service provision also changed (Figure 2). The rate of services provided by an allied health nurse and Aboriginal health worker peaked in 2020–21 (104 and 17 services per 100 people, respectively). In 2021–22, a peak in the rate of GP services was recorded (735 services per 100 people). This could be in response to the expansion and uptake of Medicare-subsidised telehealth and COVID-19 vaccinations during this time (AIHW 2022).
Figure 2: Rate (per 100 people) of primary care service provision, 2018–19 to 2022–23
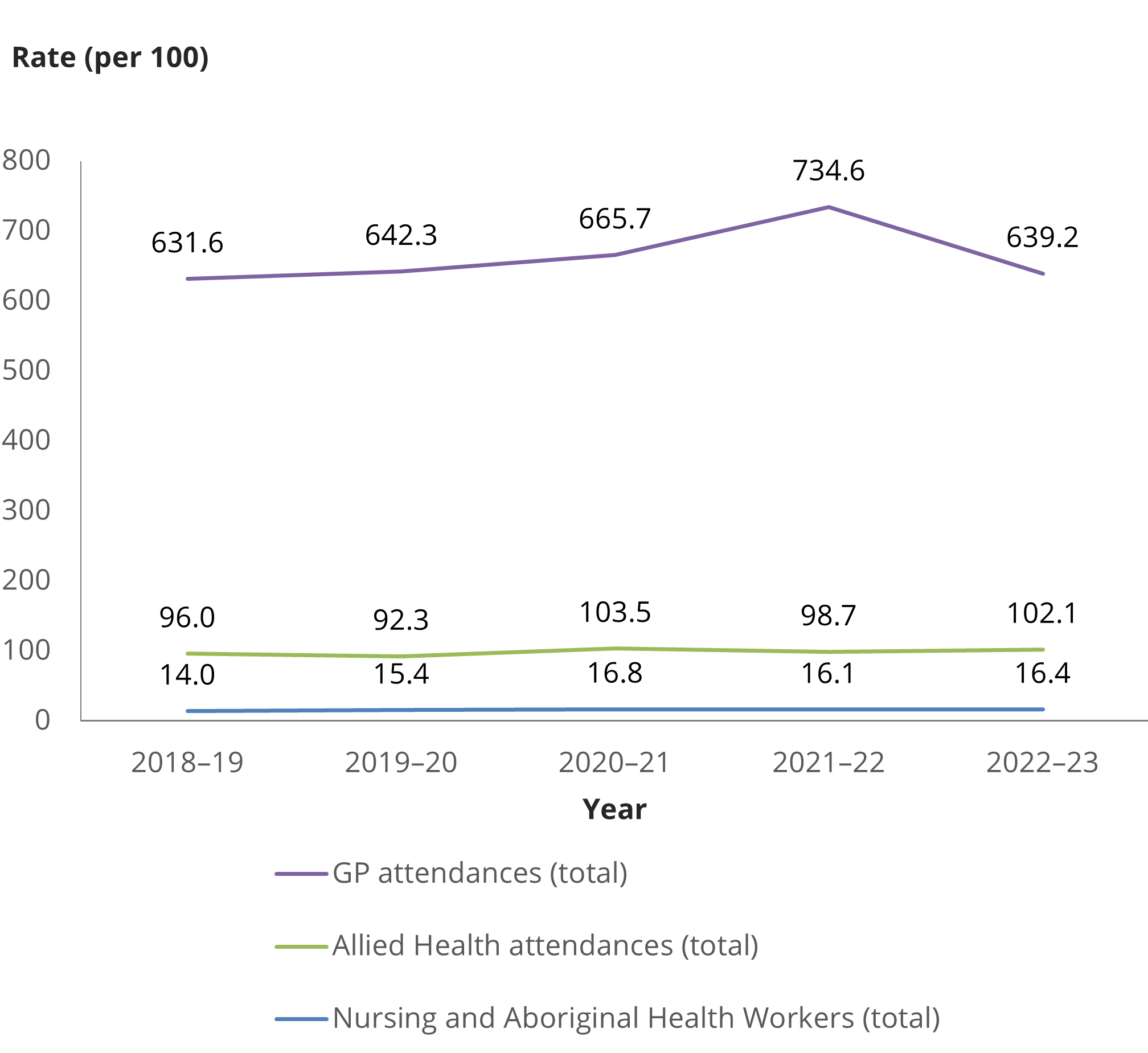
Chart: AIHW. Source: AIHW analysis of Department of Health and Aged Care Medicare Benefits Schedule (MBS) claims data, 2018–19, 2019–20, 2020–21, 2021–22, 2022–23.
Primary care services and the effects of COVID-19
The COVID-19 pandemic had a severe impact on various aspects of everyday life, including health care. The pandemic demonstrated how a health crisis can drastically influence the delivery of primary care services within the community, as seen by changes in consultation styles with patients and the uptake of digital health advancements.
Telehealth in primary care during the COVID-19 pandemic was an essential measure that enabled continuity of care. Between March 2020 and March 2022, around 17 million Australians used over 100 million telehealth consultations (Department of Health and Aged Care 2023b).
Many MBS telehealth items introduced on a temporary basis in response to the COVID-19 pandemic have now been made permanent, including telehealth services provided by GPs, medical practitioners, nurse practitioners, participating midwives, and allied health providers (Department of Health and Aged Care 2022). For more information, see the Department of Health and Aged Care.
The introduction of electronic prescribing has allowed continuity of care as well as reduced administrative burden for health care providers through more effective management of prescription refill requests (ADHA 2023). As at October 2023, over 175 million electronic prescriptions have been issued since May 2020 by more than 73,000 GP and nurse practitioner prescribers (ADHA 2023). Electronic prescribing is now widely available and forms part of the broader digital health and medicines safety framework in Australia. For more information, see Digital health.
The effects of the COVID-19 pandemic also highlighted the need to further investigate ways to support all Australians’ access to primary care services. The use of telehealth services and digital health information was found to be least accessible to those from culturally and linguistically diverse communities, those with low literacy levels, low socioeconomic status and people living in rural and remote areas (NHMRC 2022).
General practice
A GP is often the first point of contact in the health system, and over time, Australians are seeing GPs more often. From Medicare’s inception in 1984 until 2022, the yearly GP services attendance rate has increased from 3.8 to 6.8 visits per person (AIHW 2023b).
Between 2015–16 and 2019–20, almost 9 in 10 Australians received at least one Medicare-subsidised GP attendance (AIHW 2020a, 2020b). This figure dropped to 85% in 2020–21 as COVID-19 restrictions were introduced in response to the pandemic (AIHW 2021). In 2021–22, it increased to 90% of Australians, with the expansion and uptake of Medicare-subsidised telehealth and COVID-19 vaccinations (AIHW 2022). In 2022–23, it decreased to 86% of Australians who received at least one Medicare-subsidised GP attendance (AIHW 2024). This was reflected in a reduction in short (Level A) consultations, which includes straightforward services, such as vaccinations. While there were 9.1 million short (Level A) consultations in 2021–22, this decreased to 7.9 million in 2022–23: a reduction of 13% or around 1.2 million services.
The reasons for changes in rates of GP services over time are multifaceted and can include:
- the inclusion and cessation of additional telehealth and COVID-19 vaccination MBS items provided in response to the pandemic
- differing access to appropriate and affordable care for vulnerable population groups
- the availability of bulk billing to patients, such as increased bulk billing incentives for GPs during the COVID-19 pandemic (Department of Health and Aged Care 2023c).
In Australia in 2022–23, females (90%) were more likely to see a GP than males (82%) and received more Medicare-subsidised GP attendances per person (7.3, compared with 5.4 for males). This was similar to 2018–19 for females (91% saw a GP and there were 7.2 attendances per person), but a decrease for males (84% and 5.5). There was a decrease in GP attendance after hours for males over this period.
The rate of Medicare-subsidised GP services per person increased with age and was highest for those aged 80 and over (17.3 services per person) in 2022 –23. This was an increase from 16.1 services per person for those aged 80 and over in 2018–19.
A higher proportion of people living in metropolitan Primary Health Network (PHN) areas had a Medicare-subsidised GP attendance after hours (20%), compared with those in regional PHN areas (9%). This was a decrease from 2018–19, where 28% of people living in metropolitan PHN areas and 15% of those in regional PHN areas had an attendance (AIHW 2020, 2024).
Of the 166 million GP attendances in 2022–23, the most common type of attendance was a Level B consultation (a standard consultation that lasts less than 20 minutes) (107 million attendances). This was also the case in 2018–19 (99 million attendances).
Allied health
The allied health sector comprises a range of services provided by health practitioners who are generally university qualified and have specialised expertise in preventing, diagnosing and treating a range of conditions and illnesses. Allied health services include Aboriginal health workers, Aboriginal and Torres Strait Islander Health Practitioners, audiologists, chiropractors, diabetes educators, dietitians, exercise physiologists, mental health workers, occupational therapists, osteopaths, physiotherapists, podiatrists, psychologists and speech pathologists.
Allied health services subsidised by the MBS do not cover all allied health treatments. Allied health services are also accessed and funded through many arrangements, such as those subsidised by private health insurance or the Department of Veterans’ Affairs.
For more information, see Health of veterans.
In Australia in 2022–23:
- About 2 in 5 (39%) Australians received at least one Medicare-subsidised allied health service, up from 37% in 2018–19.
- Females (44%) were more likely to see an allied health professional than males (33%) and received more Medicare-subsidised services per person (1.2, compared with 0.8 for males), consistent with 2018–19.
- The number of allied health Medicare-subsidised services per person increased with age and was highest for those aged 80 and over (2.5 services per person), consistent with 2018–19.
- People living in metropolitan PHN areas received 105 Medicare-subsidised allied health services per 100 people – those living in regional PHN areas received 96 per 100 people. Compared with 2018–19, there was a greater increase in Medicare-subsidised allied health services where people were living in metropolitan PHN areas (97 per 100 people), than for those living in regional PHN areas (95 per 100 people) (AIHW 2020b; AIHW 2024).
Of the 27 million Medicare-subsidised allied health services provided in 2022–23:
- The most common type of service was optometry (11 million). This was also the case in 2018–19 (9.8 million).
- Mental health care (including psychologists and other allied mental health) accounted for around 6.9 million services, podiatry 3.6 million, and physiotherapy 3.0 million services.
- Other allied health services including dietetics, occupational therapy, speech pathology, diabetes education and audiology accounted for around 760,000 services (AIHW 2024).
Nursing and Aboriginal health workers
This section includes information on Medicare-subsidised services provided in non-admitted patient settings by:
- nurse practitioners: registered nurses with experience in a clinical specialty
- midwives: registered health professionals who care for women's health and wellbeing during pregnancy and childbirth
- practice nurses/Aboriginal health workers: registered or enrolled nurses, Aboriginal and Torres Strait Islander health practitioners, or Aboriginal health workers employed in general practice.
In 2022–23, 7.9% of Australians received at least one Medicare-subsidised nursing or Aboriginal health worker service, up from 7.1% in 2018–19 (AIHW 2020b, 2024).
In Australia, in 2022–23, the following Medicare-subsidised services were provided:
- Nurse practitioners provided more than 1 million services (3.9 services per 100 people). This is up from around 570,000 services (2.3 per 100 people) in 2018–19
- There were over 210,000 midwifery services, an increase from 2018–19 (97,000)
- There were 3.0 million practice nurse/Aboriginal health worker services provided on behalf of a medical practitioner, representing 12 services per 100 people. This is up from around 2.8 million services (11 services per 100 people) in 2018–19 (AIHW 2020b, 2024).
Health care claims data are generated and collected from the MBS. Most data relates to health goods and services received or performed (indicated by an item number), limited demographics of the patients who received them, who provided the services and at what cost (Department of Health and Aged Care 2020).
Medicare does not cover all health care services and Medicare claims data are limited in being able to indicate the reasons why a patient visited a health care provider or the actions taken to assist them. This kind of data, as well as data relating to the outcomes and quality of services provided is needed to ensure appropriate and high value care is being delivered.
Barriers to GP service use and experience of care
Australians may delay or not visit a GP due to cost, service availability and waiting times (ABS 2023).
In 2022–23:
- 23% of people delayed seeing a GP for reasons such as service availability, being too busy or experiencing long waiting times. This was a decrease from 2021–22 (25%).
- 7.0% of people who needed to see a GP delayed or did not see a GP due to cost. This was an increase from 2021–22 (3.5%).
- People with a long-term health condition were more likely to delay or not use GP services when needed than those without a long-term health condition (34% compared to 25%, respectively). Of these people, 7.8% cited cost as a reason for delaying or not seeing a GP when needed, compared with 5.9% for people without a long-term health condition.
- 29% of people delayed or did not see a GP for their own mental health when needed. Of these, 10% reported that cost was a reason.
- 30% of people felt they waited longer than acceptable for a GP appointment, compared to 23% in 2021–22 (ABS 2023).
In 2022–23, most people who needed to and saw a GP reported positive experiences:
- 71% reported their GP always listened carefully
- 80% reported their GP always showed respect
- 71% reported their GP always spent enough time with them (ABS 2023).
Expenditure on primary care services
According to the AIHW Health Expenditure Database, in 2021–22 and during the height of the COVID-19 pandemic, approximately one-third ($84.1 billion) of all health spending in Australia was for primary care. Of this:
- $13.6 billion was for unreferred medical services (mainly general practice)
- $13.4 billion was for benefit-paid pharmaceuticals
- $12.6 billion was for other medications (AIHW 2023a).
In 2021–22 there was an $8.3 billion (10.9%) increase in spending in real terms on primary health care from 2020–21. This increase was associated with spending related to the pandemic, such as:
- $7.6 billion on public health, including spending on COVID-19 vaccines, rapid antigen test kits and personal protective equipment products
- $1.1 billion on community health and other, including psychosocial program support (AIHW 2023a).
According to the Department of Health and Aged Care MBS claims data, in 2022–23, around $10.6 billion was paid in Medicare benefits for primary care services, including:
- GP attendances ($8.7 billion)
- allied health ($1.8 billion)
- nursing and Aboriginal health workers ($89 million) (AIHW 2024).
Primary health care data development
Although primary health care is an important component of Australia’s health care system, the availability of primary health care data remains limited.
This page focuses on Medicare, patient experience and expenditure data sources with national coverage. However, these sources do not provide complete nor comprehensive insight into primary health care in Australia. Nationally consistent primary health care data is a known information gap for effective population health monitoring, research, policy, and planning. The AIHW is committed to a work program that aims to fill this gap.
The AIHW is leading the development of processes for the governance, standardisation, collection, analysis and reporting of a National Primary Health Care Data Collection (NPHCDC), with the initial focus being on general practice. The initial scope of the NPHCDC will be the collection, analysis and reporting of general practice data, with a view to develop and incorporate broader primary health care data. This work program aims to improve primary health care data and address information gaps relating to why a patient went to a primary health care provider, what occurred during the consultation, what actions were recommended and taken, and with what outcome.
This work program also supports the Department of Health and Aged Care with the Primary Health Care 10 Year Plan and Strengthening Medicare Taskforce; the purposes of these are outlined below. These create national direction for those in the policy and data sectors and provide tangible recommendations to work towards.
The AIHW also releases information from the national Practice Incentives Program Quality Improvement (PIPQI) Eligible Data Set, bringing together data provided by Primary Health Networks from general practices across 10 Quality Improvement Measures.
Primary Health Care Plan
In August 2019, the Australian Government commissioned the development of a Primary Health Care 10 Year Plan (the Plan). Finalised in 2022, the Plan focusses on Australia’s primary health care services and integration of primary health care with hospitals and other parts of the health system, including aged care, disability care and social care systems (Department of Health and Aged Care 2023b). An action area of the Plan includes data-driven quality improvement to support person-centred care data development and linkage projects through collaboration with the AIHW and other peak organisations.
Strengthening Medicare
To support the Plan, the Australian Government brought together health leaders to form the Strengthening Medicare Taskforce (the Taskforce), with a focus on strengthening Medicare to lay the foundations for longer-term reform and investment in the primary care system (Department of Health and Aged Care 2023c).
In December 2022, the Taskforce released the Strengthening Medicare Taskforce Report which details recommendations on increasing access to, and modernisation of, primary care in Australia (Department of Health and Aged Care 2023c). Recommendations included:
- modernising My Health Record to significantly increase the health information available to individuals and their health care professionals
- better connecting health data across all parts of the health system
- investing in better health data for research and evaluation of models of care and to support health system planning
- providing an uplift in primary care IT infrastructure, education and support to primary care practices
- making it easier for all Australians to access, manage, understand and share their own health information (Department of Health and Aged Care 2023c).
In response to these recommendations the Australian Government announced a $824 million investment in digital health within the 2023–24 May Budget, including to modernise the My Health Record system and fund other digital health initiatives (Department of Health and Aged Care 2023d). The Australian Government is also introducing the MyMedicare voluntary patient registration system to strengthen the relationship between patients, their general practice, GPs and primary care teams to produce better continuity of care.
Ongoing work to improve primary health care data, including establishing linked primary health care data, will enhance the evidence for policy, planning, research and practice.
Where do I go for more information?
For more information on primary health care, see:
- Primary health care data development, for updates on the development of AIHW’s National Primary Health Care Data Collection
- Department of Health and Aged Care 10 Year Primary Health Care Plan
For more on this topic, visit Primary health care.
ABS (Australian Bureau of Statistics) (2023) Patient experiences in Australia: summary of findings, 2022–23, ABS website, accessed 21 November 2023.
Australian Digital Health Agency (ADHA) (2023) Electronic prescriptions for prescribers, ADHA website, accessed 24 November 2023.
AIHW (Australian Institute of Health and Welfare) (2020a) Impacts of COVID-19 on Medicare Benefits Scheme and Pharmaceutical Benefits Scheme service use, AIHW website, accessed 11 February 2022.
AIHW (2020b) Medicare-subsidised GP, allied health and specialist health care across local areas: 2013–14 to 2018–19, AIHW website, accessed 18 November 2023.
AIHW (2021) Medicare-subsidised GP, allied health and specialist health care across local areas: 2019–20 to 2020–21, AIHW website, accessed 18 November 2023.
AIHW (2022) Medicare-subsidised GP, allied health and specialist health care across local areas: 2021–22, AIHW website, accessed 18 November 2023.
AIHW (2023a) Health Expenditure Australia 2021–22, AIHW website, accessed 25 October 2023.
AIHW (2023b) Medicare funding of GP services over time, AIHW, Australian Government, accessed 24 November 2023.
AIHW (2024) Medicare-subsidised GP, allied health and specialist health care across local areas: 2022–23.
Department of Health and Aged Care (2020) An MBS for the 21st Century Recommendations, Learnings and Ideas for the Future, Department of Health and Aged Care website, accessed 3 January 2023.
Department of Health and Aged Care (2022) Temporary COVID-19 MBS Telehealth Services – Factsheet, Department of Health and Aged Care website, accessed 22 November 2023.
Department of Health and Aged Care (2023b) Australia’s Primary Health Care 10 Year Plan 2022–2032, Department of Health and Aged Care website, accessed 31 October 2023.
Department of Health and Aged Care (2023c) Strengthening Medicare Taskforce Report, Department of Health and Aged Care website, accessed 31 October 2023.
Department of Health and Aged Care (2023d) Budget 2023–24 - Strengthening Medicare, Department of Health and Aged Care website, accessed 20 November 2023.
NHMRC (National Health and Medical Research Council) (2022) Strengthening Australia’s health system post COVID-19, PHCAG, accessed 22 November 2023.


