Maternal deaths in Australia
In Australia, where childbirth is safe for most women, maternal death is rare. All maternal deaths are reviewed by health professionals to determine the likely cause and whether the pregnancy contributed to the death.
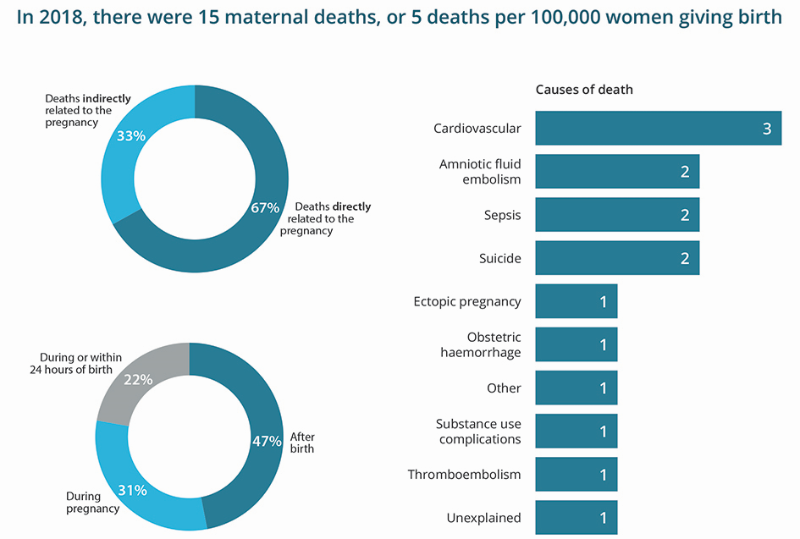
Maternal death is the death of a woman while pregnant or within 42 days of the end of pregnancy, regardless of the duration or outcome of the pregnancy. Maternal deaths are divided into two categories, direct and indirect. Direct maternal deaths are those resulting from obstetric complications of pregnancy or its management. Indirect maternal deaths are those resulting from diseases or conditions that were not due to a direct obstetric cause, but were aggravated by the physiologic effects of pregnancy. Deaths considered to be causally unrelated to pregnancy are classified as coincidental (see below for more information on these deaths).
Figure 1: Maternal deaths in Australia, 2018
Maternal mortality over time
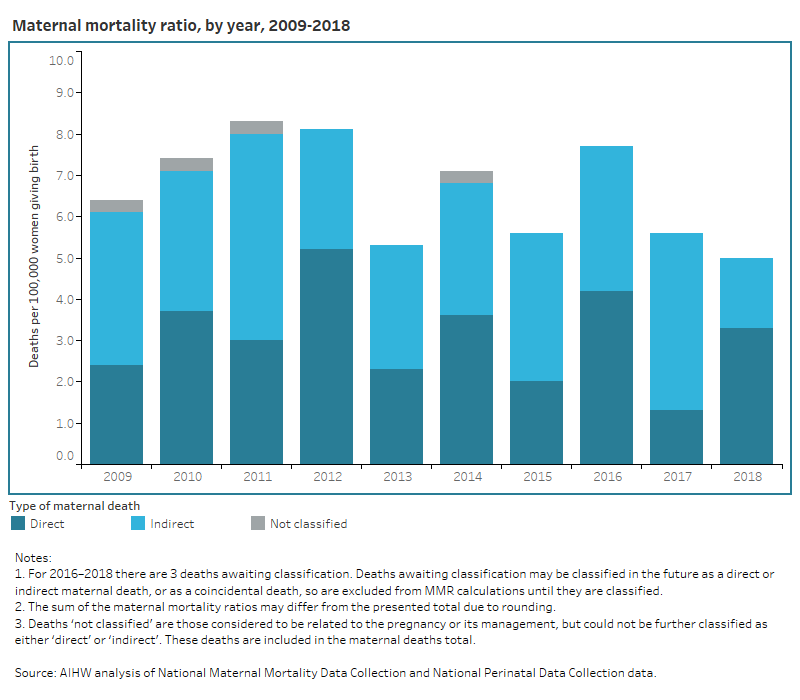
The incidence of maternal death is expressed as the maternal mortality ratio (MMR). The MMR is calculated using direct, indirect and not classified maternal deaths (excluding coincidental deaths and deaths awaiting classification) and expressed as per 100,000 women giving birth. Between 2009 and 2018, the MMR in Australia was relatively stable, ranging from between 5.0 to 8.4 per 100,000 women giving birth. Fluctuations appear to reflect the normal variability that might be expected with rare events such as maternal deaths.
Chart title: Maternal mortality ratio, by year, 2009-2018
The horizontal bar chart shows that the maternal mortality ratio ranged between 5.0 deaths per 100,000 women giving birth and 8.4 deaths per 100,000 women giving birth.
Causes of maternal deaths
The most frequent causes of maternal death reported in Australia between 2009 and 2018 were complications of pre-existing cardiovascular disease and non-obstetric haemorrhage (mostly haemorrhage within the brain and haemorrhage from a ruptured aneurysm of the splenic artery).
The most frequent causes of direct maternal death between 2009 and 2018 were thromboembolism and obstetric haemorrhage.
Chart title: Number of maternal deaths, by cause of death, 2009-2018
The horizontal bar chart shows that the most common cause of maternal death was cardiovascular disease (29 maternal deaths) and the least common cause of maternal death was cancer (1 maternal death).

Coincidental deaths are defined as those that are reported to have occurred during pregnancy or within 42 days of the end of pregnancy, but are considered to be causally unrelated to pregnancy. Unlike direct and indirect maternal deaths, coincidental deaths are excluded from analysis and MMR calculations.
There were 46 coincidental deaths in Australia from 2009–2018. The most common causes of these deaths were motor vehicle trauma and cancer. For more information visit data tables 1 & 2.
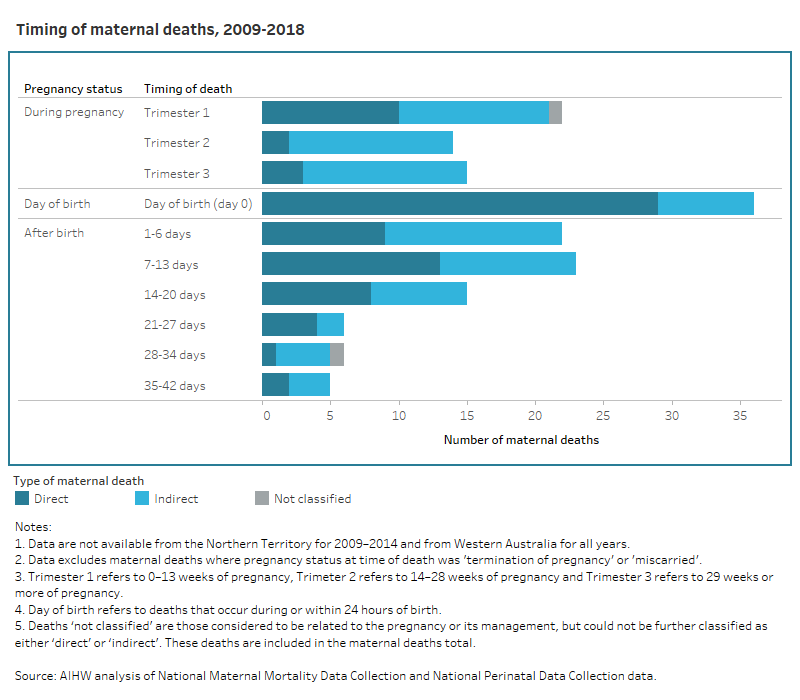
Timing of maternal deaths
Understanding the timing of maternal deaths is important for identifying periods of critical risk. Between 2009 and 2018 nearly one third (31%) of maternal deaths occurred in women who were reported to be pregnant at the time of their death, and of these women more 2 in 5 (43%) died during the first trimester of pregnancy (less than 14 weeks of pregnancy).
In the same period, one in five (22%) maternal deaths were reported to have occurred during the birth process or within 24 hours of giving birth, and nearly half (47%) of all maternal deaths occurred after birth, with 3 in 5 (58%) deaths occurring within 1 to 13 days of giving birth. These proportions do not include maternal deaths following or due to miscarriage or termination of pregnancy as the timing of death was not adequately reported for these cases.
Chart title: Timing of maternal deaths, 2009-2018
The horizontal bar chart shows that 51 maternal deaths occurred during pregnancy, 36 maternal deaths occurred during or within 24 hours of birth and 77 maternal deaths occurred after birth.
Characteristics of women who died
This section presents some demographic characteristics of the women who died from 2012–2018. It should be noted that not all demographic information was available for all women who died.
Chart title: Maternal mortality ratio, by maternal age, 2012-2018
The horizontal bar chart shows that the maternal mortality ratio ranged between 18.7 deaths per 100,000 women giving birth for women aged less than 20 to 2.2 deaths per 100,000 women giving birth for women aged 20-24
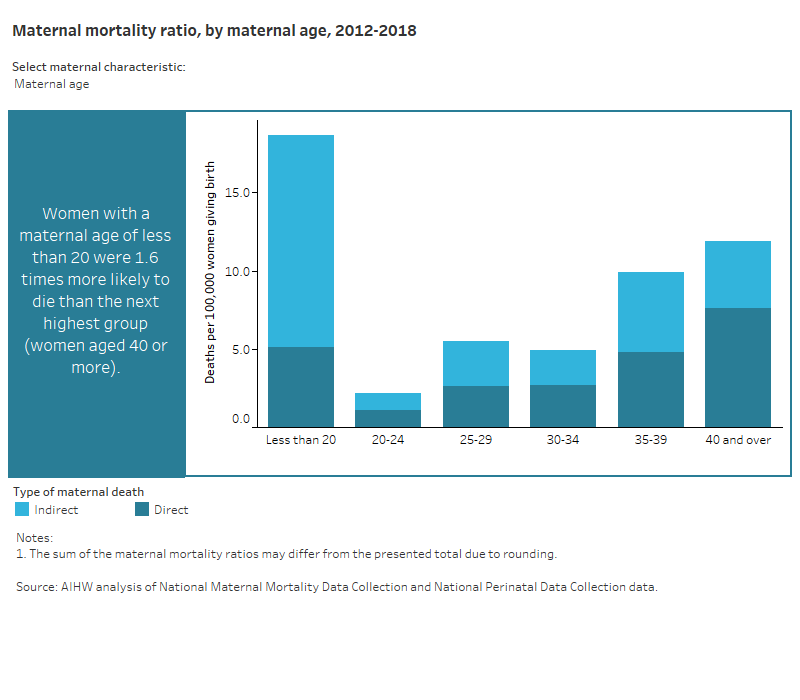
Maternal age
Women aged less than 20 had the highest MMR, followed by those aged 40 or more (18.7 and 11.9 per 100,000 women giving birth). The lowest MMR was for women in the 20 to 24 age group, followed by women in the 30 to 34 age group (2.2 and 4.9 per 100,000 women giving birth).
Maternal Indigenous status
Between 2012 and 2018, the MMR for Aboriginal and Torres Strait Islander women was 20.2 per 100,000 women giving birth. In the same period, the MMR for non-Indigenous women was 5.5 per 100,000 women giving birth.
Parity
Parity refers to a woman’s number of previous pregnancies, excluding the current pregnancy, carried to a viable gestational age (usually 20 weeks). The rate of maternal death increased with parity, from an MMR of 4.7 per 100,000 women giving birth for women with a parity of none, to an MMR of 4.6 per 100,000 women giving birth for women with a parity of 1, and increasing up to 14.6 per 100,000 women giving birth for women with a parity of 4 or more.
Smoking status
The rate of maternal deaths was higher in women who reported smoking during the first 20 weeks of pregnancy than in women who reported that they did not smoke during the first 20 weeks of pregnancy (16.7 compared to 3.4 per 100,000 women giving birth). As the number of maternal deaths with an unknown smoking status is relatively high (37% of data from included jurisdictions), caution should be used when interpreting these data.
Remoteness
Women who lived in Remote and Very Remote areas had the highest MMR, followed by women who lived in Inner Regional areas (12.3 and 8.9 per 100,000 women giving birth). The lowest MMR was for women who lived in Major Cities (5.7 per 100,000 women giving birth). The rate of maternal death in areas other than Major Cities should be treated with caution due to the small numbers.


