Summary
Maternity models of care in Australia in 2023
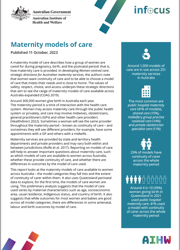
A maternity model of care describes how a group of women are cared for during pregnancy, birth, and the postnatal period. In 2023:
- Around 1,000 models of care were in use across 251 maternity services.
- Most of these (81%) fall into 4 categories: public hospital maternity care (41%), shared care (15%), midwifery group practice caseload care (14%), and private obstetrician specialist care (11%).
- Over two-thirds of public maternity services (69%) have at least one public hospital maternity care model of care, 60% have a shared care model of care, and 49% a midwifery group practice caseload care model of care.
- Around 29% of models have continuity of carer for the whole maternity period; nearly three-quarters (73%) of maternity services have at least one model of care with continuity of carer for the whole maternity period.
- Around 35% of models have continuity of carer for part of the maternity period, such as the antenatal period only; a similar proportion (36%) have no continuity of carer.
Maternity models of care in women giving birth in Queensland in 2021
Most women giving birth in Queensland in 2021 (94%) used either: public hospital maternity care (39%), private obstetrician specialist care (22%), midwifery group practice caseload care (18%), or shared care (15%). A small proportion used public hospital high risk maternity care (2.7%) and just 3.8% used a model of care that fell into another model category.
Around 4 in 10 women (41%) used a model of care with continuity of carer across the whole maternity period, largely reflecting the use of private obstetrician specialist care and midwifery group practice caseload care.
The model of care used varies by maternal characteristics. For example:
- Women aged 35 to 39, or 40 years and over were more likely to use private obstetrician specialist care (33% and 35% respectively, compared with 22% overall), as were women in the least disadvantaged socioeconomic areas (42%, compared with 22% overall).
- Aboriginal and Torres Strait Islander (First Nations) women were less likely to use private obstetrician specialist care than non-Indigenous women (2.5%, compared with 23%).
- Women born in Australia were more likely to use midwifery group practice caseload care than those born overseas (20%, compared with 14%); those born overseas were more likely to use shared care (21%, compared with 12%).
Antenatal, labour and birth outcomes for most women and babies were good across all model categories, including high risk models of care. There were, however, some differences across them. In looking at these it is important to remember that some models of care will target specific groups of women and differences may be related to the characteristics of the women these models of care were designed for.
- The proportion of women having a non-instrumental vaginal birth was higher in those using midwifery group practice caseload care (68%), and lower in those using private obstetrician specialist care (34%) or public hospital high risk maternity care (42%).
- The proportion of women having a caesarean section was higher in those using private obstetrician specialist care (56%) or public hospital high risk maternity care (52%), and lower in those using midwifery group practice caseload care (23%).
- A higher proportion of babies born to women using public hospital high risk maternity care had poorer outcomes across some indicators, for example being born pre-term, or with a low birthweight. This is not surprising as these models of care are designed to support women with known medical high risk or complex pregnancies.
Key findings
1. What is a maternity model of care?
2. Why report on models of care?
3. How many models of care are there?
4. What are the most common models of care?
5. How many women use different models of care?
6. Do antenatal, labour and birth outcomes vary by model of care?
7. Conclusion
8. About the data
End matter: Glossary, References, Acknowledgements.