QIM 1: Proportion of regular clients with diabetes with an HbA1c result recorded in their GP record within the previous 12 months
On this page
- Overview
- Regional proportions of regular clients with diabetes and a current HbA1c
- National proportion of regular clients with diabetes and a current HbA1c result by age and sex
- References
Patients with Type 1 and 2 diabetes should have their glycosylated haemoglobin (HbA1c) measured at least every 12 months, or more frequently depending on the level of blood glucose control. The early identification and optimal management of diabetes can delay the progression of disease, improve quality of life, increase life expectancy, and decrease the need for high-cost interventions (RACGP 2020).
Capture of results recorded outside of the general practice setting
Some patients may receive care from other practitioners in addition to a GP including an endocrinologist/a specialist physician, and/or other health care providers to safely manage their diabetes (RACGP 2020). Results arising from clinical intervention conducted outside of the service that are known and recorded by the practice are included in the measure. However, sometimes an HbA1c result recorded elsewhere (for example, specialist service) is not recorded in the clinical information system of the client’s usual general practice (for example, due to incompatible clinical information system between a practice and a specialist service), meaning that these data will not be captured in the report.
Other sources of relevant data
Data on the prevalence of long-term health conditions like diabetes are captured in the National Health Survey (NHS) conducted by the Australian Bureau of Statistics (ABS). There are other administrative data collections where the data from these client-provider interactions are captured, e.g. Medicare Benefits Schedule (MBS), the National Diabetes Service Scheme (NDSS) register, and the Australasian Paediatric Endocrine Groups (APEG) state and territory registers.
This indicator reports on the proportion of regular clients of all ages who had a recorded diagnosis of Type 1, Type 2, or undefined diabetes, and who had an HbA1c result recorded within the previous 12 months in their GP record.
Regional proportions of regular clients with diabetes and a current HbA1c
Type 1 diabetes
Type 1 diabetes is a lifelong autoimmune disease that usually has its onset in childhood or early adolescence. The exact cause is unknown but it is believed to be the result of an interaction of genetic and environmental factors. The management of an individual with Type 1 diabetes requires a multidisciplinary healthcare network delivering integrated clinical care, using a complex array of health‐care tools (APEG and ADS 2011). A person with Type 1 diabetes requires daily insulin replacement to survive, except in cases where a pancreatic transplant occurs. In 2017-18, around 145,000 people had Type 1 diabetes of which 20,700 were children and young adults aged 0–24 years. This equates to 261 per 100,000 population, with a slightly higher rate among males compared with females (266 and 256 per 100,000 population, respectively) (AIHW 2020).
As of July 2021, nationally, 59.0% of regular clients of all ages who had a recorded diagnosis of Type 1 diabetes had an HbA1c result recorded within the previous 12 months in their GP record. This varied from 49.0% to 69.4% across PHNs.
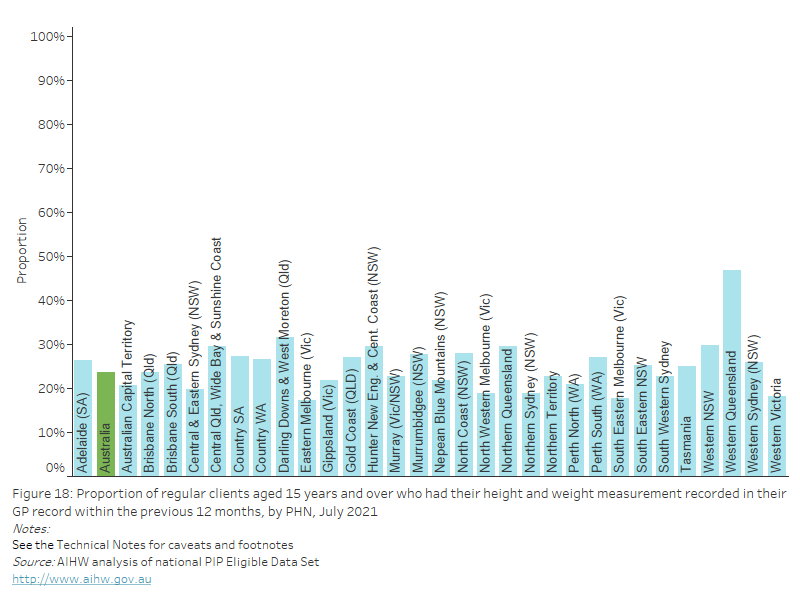
Figure 1: Proportion of regular clients with a recorded diagnosis of Type 1 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by PHN, July 2021
Figure 1: Proportion of regular clients with a recorded diagnosis of Type 1 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by PHN, July 2021
Type 2 diabetes
Type 2 diabetes is a chronic and progressive medical condition that results from two major metabolic dysfunctions: insulin resistance followed by pancreatic islet cell dysfunction, causing a relative insulin deficiency. These metabolic dysfunctions occur due to modifiable lifestyle-related risk factors interacting with non-modifiable and genetic risk factors. The relative insulin deficiency leads to chronic hyperglycaemia and multiple disturbances in carbohydrate, protein and fat metabolism (RACGP 2020). Type 2 diabetes is the most common form of diabetes, generally having a later onset than Type 1 diabetes, people with Type 2 diabetes produce insulin, but do not produce enough, and/or cannot use it effectively. It involves a genetic component, but is largely preventable and is often associated with lifestyle factors including physical inactivity, poor diet, being overweight or obese, and tobacco smoking. Type 2 diabetes can be managed with changes to diet and exercise, oral glucose-lowering medications, non-insulin injectable glucose-lowering medications, insulin injections, or a combination of these methods (RACGP 2020). Although it has typically been considered a disease of older people, reports show that it is being diagnosed at younger ages than in the past. Almost 1 million Australian adults had Type 2 diabetes in 2017–18 (ABS 2018).
As of July 2021, nationally, 73.4% of regular clients of all ages who had a recorded diagnosis of Type 2 diabetes had an HbA1c result recorded within the previous 12 months in their GP record. This varied from 66.5% to 82.1% across PHNs.
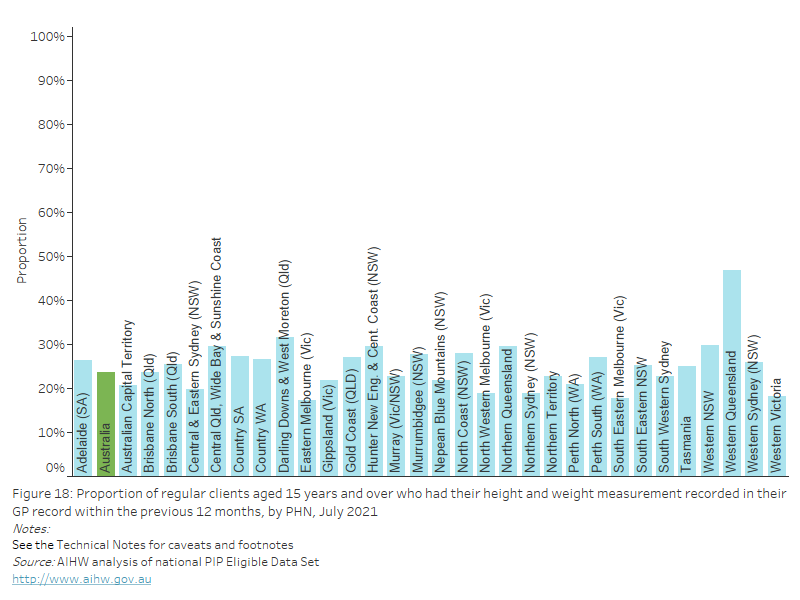
Figure 2: Proportion of regular clients with a recorded diagnosis of Type 2 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by PHN, July 2021
Figure 2: Proportion of regular clients with a recorded diagnosis of Type 2 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by PHN, July 2021
Undefined diabetes
As of July 2021, nationally, 66.3% of regular clients of all ages who had undefined diabetes recorded had an HbA1c result recorded within the previous 12 months in their GP record. This varied from 58.1% to 76.4% across PHNs.
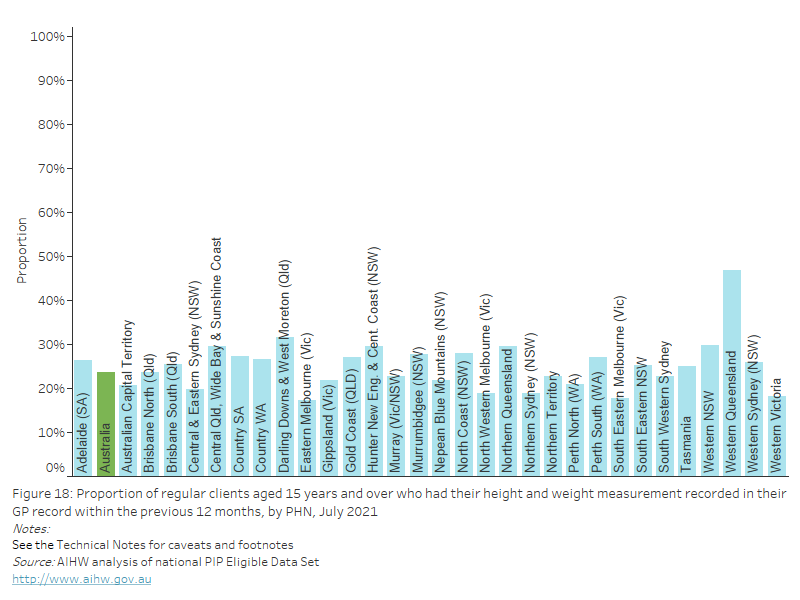
Figure 3: Proportion of regular clients with undefined diabetes recorded and an HbA1c result recorded in their GP record within the previous 12 months, by PHN, July 2021
Figure 3: Proportion of regular clients with undefined diabetes recorded and an HbA1c result recorded in their GP record within the previous 12 months, by PHN, July 2021
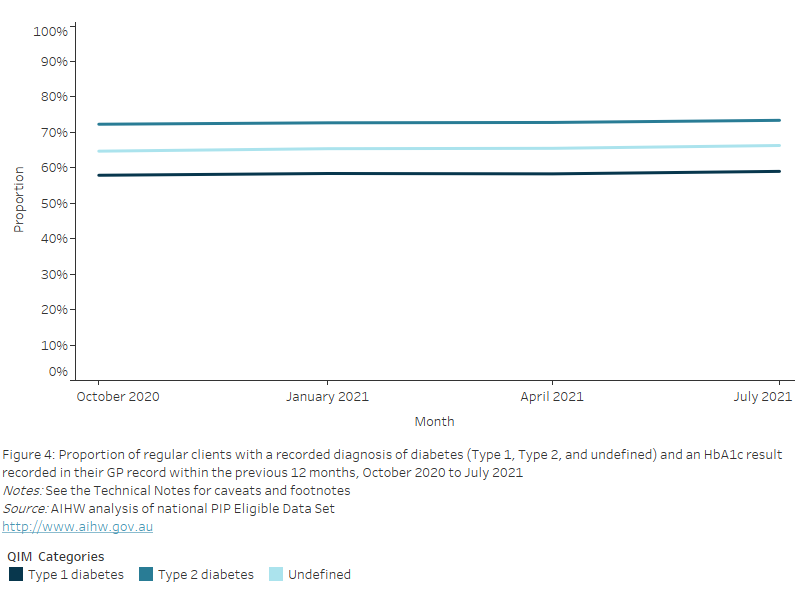
Nationally, between October 2020 and July 2021, the proportion of regular clients of all ages who had an HbA1c result recorded within the previous 12 months in their GP record, remained constant:
- at 57.9% and 59.0% for Type 1 diabetes.
- at 72.3% and 73.4% for Type 2 diabetes.
- at 64.7% and 66.3% for undefined diabetes.
Figure 4: Proportion of regular clients with a recorded diagnosis of diabetes (Type 1, Type 2, and undefined) and an HbA1c result recorded in their GP record within the previous 12 months, October 2020 to July 2021
Figure 4: Proportion of regular clients with a recorded diagnosis of diabetes (Type 1, Type 2, and undefined) and an HbA1c result recorded in their GP record within the previous 12 months, October 2020 to July 2021
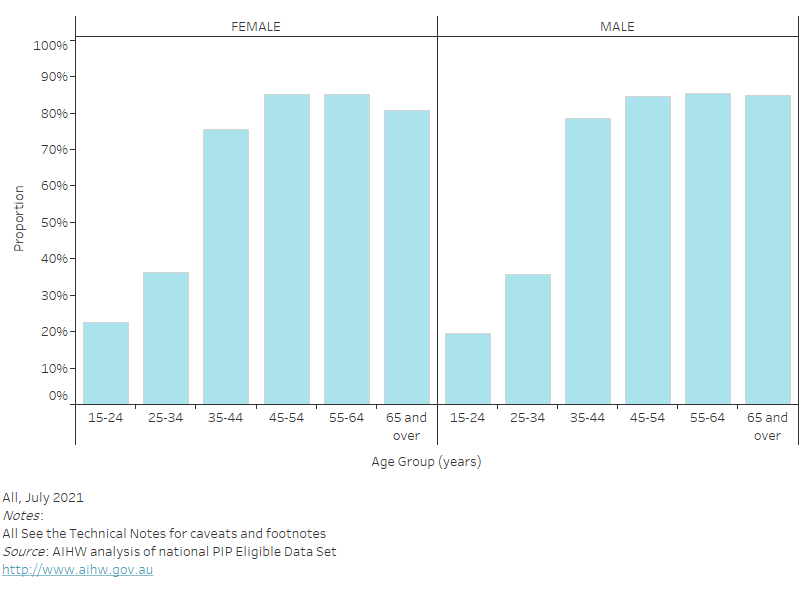
National proportion of regular clients with diabetes and a current HbA1c result by age and sex
Type 1 diabetes
As of July 2021, nationally, the proportion of regular clients of all ages who had Type 1 diabetes and who had an HbA1c result recorded within the previous 12 months in their GP record, increased with age and was:
- highest in the 65 years and over age group for both females (74.1%) and males (75.2%).
- lowest in the 0–14 years age group for both females (22.4%) and males (20.1%).
Figure 5: Proportion of regular clients with Type 1 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by age and sex, July 2021
Figure 5: Proportion of regular clients with Type 1 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by age and sex, July 2021
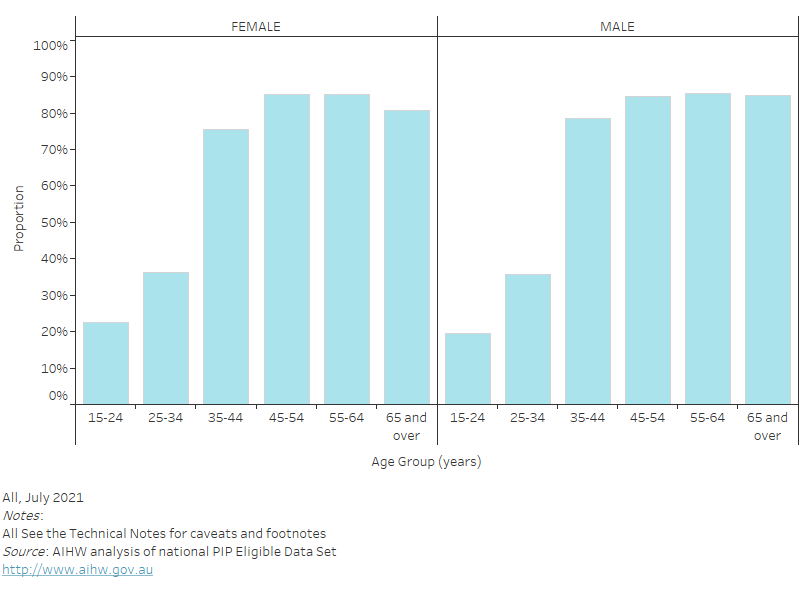
Type 2 diabetes
As of July 2021, nationally, the proportion of regular clients of all ages who had Type 2 diabetes and who had an Hb1Ac result recorded in their GP record within the previous 12 months also increased with age and was:
- highest in the 65 years and over age group for both females (74.6%) and males (76.1%).
- lowest in the 0-14 years age group for both females (14.9%) and males (12.7%).
Figure 6: Proportion of regular clients with Type 2 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by age and sex, July 2021
Figure 6: Proportion of regular clients with Type 2 diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by age and sex, July 2021
Undefined diabetes
As of July 2021, nationally, the proportion of regular clients of all ages who had undefined diabetes and who had an HbA1c result recorded in their GP record also increased with age and was:
- highest in the 65 years and over age group for both females (68.3%) and males (69.2%).
- lowest in the 0-14 years age group for both females (15.7%) and males (9.5%).
Figure 7: Proportion of regular clients with undefined diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by age and sex, July 2021
Figure 7: Proportion of regular clients with undefined diabetes and an HbA1c result recorded in their GP record within the previous 12 months, by age and sex, July 2021

- A client is classified as having diabetes for this measure, if they have Type 1 or Type 2 or undefined diabetes as a diagnosis in their GP record.
- Clinical definitions for diabetes vary across clinical information systems, as different coding schemes are used. This may lead to some variation in the number of clients who will be picked up by different systems (Department of Health 2017).
- Any clients who had gestational diabetes but also have Type 1 or 2 diabetes are included in the measure.
- Multidisciplinary care delivered by multiple providers are often required to safely manage patients with diabetes and its complications. For example, younger patients and patients with Type 1 diabetes are more likely to receive shared care from specialist services. Missing information on HbA1c for these patients could relate to the information not being shared electronically between the specialist services and general practices.
- Results arising from measurements conducted outside of the service that are known and recorded in the GP record are included.
- Clients are excluded from the measure if they:
- had secondary diabetes, gestational diabetes mellitus (GDM), previous GDM, impaired fasting glucose, impaired glucose tolerance,
- had results from measurements conducted outside of the service which were not available to the service and had not visited the service in the previous 12 months.
- There are other administrative data collections where the data from these client-provider interactions are captured for example, Medicare Benefits Schedule (MBS), the National Diabetes Service Scheme (NDSS) register, the Australasian Paediatric Endocrine Groups (APEG) state and territory registers.
Australian Bureau of Statistics (ABS) 2018. National Health Survey: first results, 2017–18. ABS cat. no. 4324.0.55.001. Canberra: ABS. Viewed 12 August 2021.
AIHW 2020. Diabetes. Cat. no. CVD 82. Canberra: AIHW. Viewed 12 August 2021.
Australasian Paediatric Endocrine Group (APEG) and Australian Diabetes Society (ADS) 2011. National evidence-based clinical care guidelines for type 1 diabetes in children, adolescents and adults, Canberra: Department of Health. Viewed 12 August 2021.
Department of Health 2017. National Key Performance Indicators for Aboriginal and Torres Strait Islander primary health care - Data Validation Project Report. Canberra: Department of Health.
RACGP 2020. Management of type 2 diabetes: A handbook for general practice. East Melbourne, Vic: RACGP. Viewed 12 August 2021.


