Radiotherapy waiting times
A waiting time was calculated for every record with a valid ready-for-care date and radiotherapy course start date (99.4% of all courses of radiotherapy that began in Australia in 2018–19; almost 73,800 records). See Box: Calculation of waiting time from ready-for-care date below, for more information. See Technical notes for details of data exclusions for waiting times calculations.
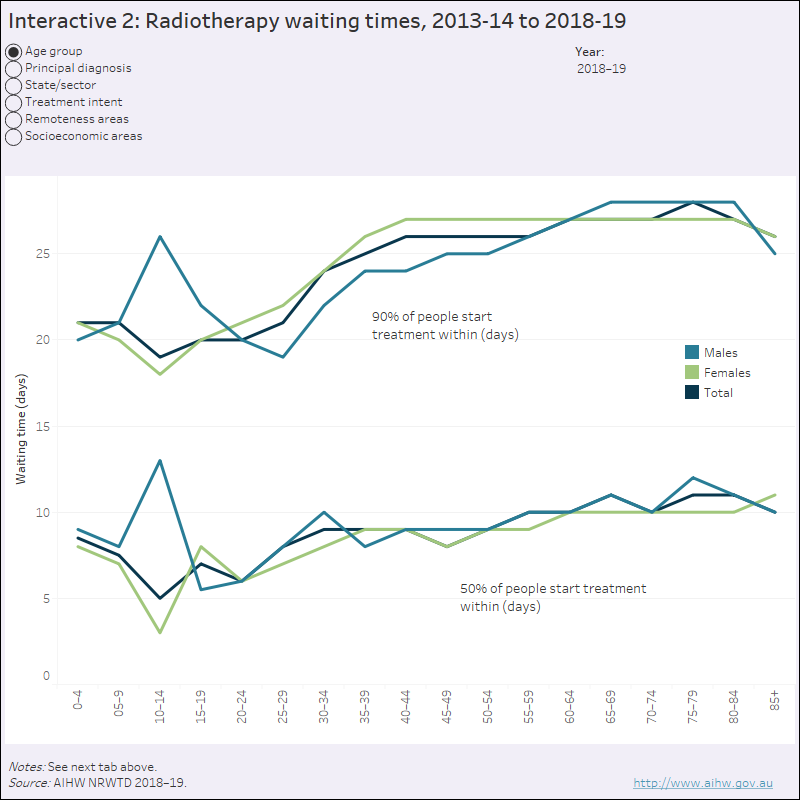
Waiting times for all patients are presented as the number of days a patient waited at the 50th and 90th percentiles:
- The 50th percentile (the median waiting time, or the middle value in a group of data arranged from lowest to highest for the number of days waited) represents the number of days within which 50% of patients began radiotherapy treatment.
- The 90th percentile data represent the number of days within which 90% of patients began treatment.
50% of all patients received treatment within 10 days of being assessed as ready for care
90% of all patients received treatment within 27 days of being assessed as ready for care
Waiting times are presented by state and territory for public providers, nationally for private providers, and in total. While the data are presented separately for public and private providers in this report, comparisons should be made with caution because some data recording practices may differ across individual sites, states and territories, and sectors, particularly in the way ready-for-care dates are set, which affects the calculation of waiting times. These differences may also reflect varying service provision arrangements between the public and private sectors (and in both sectors across jurisdictions).
Comparison of waiting times between 2013–14 and 2014–15, and subsequent years should be undertaken with caution due to differences in participation rates by private radiotherapy providers which generally report shorter waiting times. There were more submissions of data on radiotherapy courses with valid waiting times by private providers in 2015–16, 2016–17, 2017–18 and 2018–19 collections than in previous years.
Interactive figure 2 presents data for 2013–14 to 2018–19, by sex and by:
- age group
- top 10 principal diagnoses
- intent of treatment
- state/territory and sector
- remoteness of residence, and
- socioeconomic area of the person.
Key points for radiotherapy courses started in 2018–19
- Overall, waiting times were the same for males and females (50% treated within 10 days and 90% within 27 days).
- Waiting times (by intention of treatment) were shortest for patients receiving palliative radiotherapy (50% treated within 7 days), and were longest for patients receiving curative radiotherapy (50% within 14 days).
- 50% of people receiving non-emergency treatment were treated within 10 days, 90% within 27 days.
- For male patients with prostate cancer (25% of men), 50% started treatment within 12 days, and 90% within 34 days.
- For female patients with breast cancer (42% of females), 50% started treatment within 11 days, and 90% within 28 days.
Emergency radiotherapy
An emergency course of radiotherapy is defined as treatment required within 24 hours of the patient being determined to be ready for care, in the opinion of the treating clinician. However, as only the date the patient was ready for care and the date they started the course of radiotherapy are collected (and information about the time of day is not available), this indicator is reported as the proportion of patients who were treated either on the same day or the day after they were ready for care.
There were 1,101 emergency courses in 2018–19 (1.5% of courses); 1,093 of these had valid waiting times.
96% of patients who were clinically assessed as emergency patients began treatment on the same or the
next day
Socioeconomic and remoteness areas
Area-of-usual-residence data can be used to calculate remoteness and socioeconomic of the area where a patient usually resides. The population living in the 20% of areas with the greatest overall level of disadvantage is described as the ‘lowest socioeconomic areas’. The 20% at the other end of the scale—the top fifth—is described as the ‘highest socioeconomic areas’.
Waiting times were shortest for those patients living in the highest socioeconomic areas — 50% of patients began treatment within 8 days.
Compared with those living in the lowest socioeconomic areas — 50% began treatment within 12 days.
While waiting times by remoteness were similar to each other, this may reflect the fact that waiting times are only measured from when a patient is ready for care, so any delays in accessing care due to the need to travel to providers are not captured in this dataset.
Data visualisation Interactive 2: Radiotherapy waiting times, 2013–14 to 2018–19. Interactive figure 1 presents waiting times data for 2013–14 to 2018–19, by sex and by age group, top 10 principal diagnoses, intent of treatment, state/territory and sector, remoteness of residence, and socioeconomic area of the person. Details can be found in the supplementary tables
Calculation of waiting time from ready-for-care date
The waiting time is the number of days from when the patient is ready to be treated with radiotherapy in the opinion of the treating clinician (‘ready for care’) until the day the patient first receives radiotherapy treatment—that is, the number of days between the Ready-for-care date and the Radiotherapy start date. Reported waiting times include non-working days (such as weekends or public holidays) and other days on which a service was not able to provide services (such as when key staff are unavailable or where there has been equipment failure).
Other waiting periods—such as the time between when a person contacts their general practitioner and their first appointment with a medical oncologist, and the time between receipt of the patient’s first referral to a radiation oncologist to the date of that patient’s first consultation with a radiation oncologist—are not collected in this data set.
The ready-for-care date is set by the treating clinician and takes into account things such as the need for prior treatment or post-operative healing. If the patient is not ready for care on this date for personal reasons, the ready-for-care date will be set at a later time, when the patient states they are ready.
Service bottlenecks or peak periods of demand that may affect ease of access to radiotherapy services should not influence clinical decisions around the setting of ready-for-care dates. Treatment may be delayed due to waiting times in pre-treatment imaging or testing, treatment service availability, staff shortages, equipment breakdown, or even a lack of available accommodation for a patient travelling for treatment. Factors that are, and are not, expected to influence the ready-for-care date are described in the metadata for ‘Ready-for-care date’ available in METeOR (METeOR identifier: 448141).
References
RANZCR (Royal Australian and New Zealand College of Radiologists) 2015. What is radiation therapy? Sydney: RANZCR. Viewed 19 August 2020.


