Treatment
Many types of treatment are available in Australia to assist people with problematic drug use. Most aim to reduce the harm of drug use, for example counselling, information and education, and diversion programs, while some use a structured drug-free setting with abstinence oriented interventions to help prevent relapse and develop skills and attitudes that assist clients to make changes leading to drug-free lifestyles.
Drugs of concern
- Alcohol, cannabis, amphetamines and heroin have remained the top principal (that is, main) drugs for which clients received treatment since 2006–07—this is the same for both Indigenous and non-Indigenous clients.
- In 2015–16, 32% of closed treatment episodes were for alcohol, 23% for cannabis, 23% for amphetamines and 6% for heroin as the main drug of concern.
- Across most states and territories alcohol was also the top drug of concern; however in SA and WA it was amphetamines, and in Qld it was Cannabis.
- Treatment for the use of amphetamines increased over the 5 years to 2015–16 (from 11% of closed treatment episodes to 23%).
Treatment delivery setting
- The majority of clients receiving treatment for heroin (76%), cannabis (72%) amphetamines (68%), or alcohol (68%) as their principal drug of concern, received treatment in a non-residential treatment facility, such as a community health centre (Figure Treatment 1).
- Residential treatment facilities (where clients reside in a facility that is not their home or usual place of residence) were the second most common treatment setting for clients with amphetamines (19%), heroin, or alcohol (both 17%) as their principal drug of concern (Figure Treatment 1).
- Outreach settings were the second most common for clients receiving treatment for cannabis (16%) as their main drug of concern (Figure Treatment 1).
Figure Treatment 1: Closed treatment episodes provided, by selected principal drugs of concern and treatment delivery setting (%), 2015–16
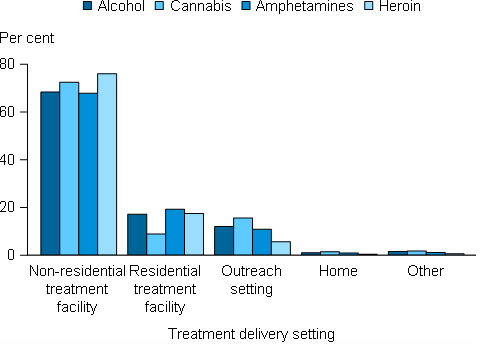
Source: AODTS NMDS. See Supplementary Table S1.
Treatment types
- Counselling continues to be the most common main treatment type provided to clients, comprising almost 2 in 5 (38%) closed treatment episodes in 2015–16 for all clients
- It has continued to be the most common main treatment type since 2006–07, and for both Indigenous and non-Indigenous clients
- In 2015–16, assessment only was the second most common main treatment type (16%), followed by support and case management only (13%).
Length of treatment
For those clients seeking treatment for their own drug use:
- In 2015–16, the median duration of treatment for closed treatment episodes was just under 3 weeks (19 days).
- Treatment duration varied by drug of concern. In 2015–16, the median duration of closed treatment episodes was 39 days for clients receiving treatment for heroin, 28 days for amphetamines, 27 days for alcohol, and 13 days for cannabis (Figure Treatment 2).
- Almost 4 in 5 (79%) closed treatment episodes in 2015–16 ended within 3 months.
- Over the 5 years to 2015–16, clients receiving treatment for heroin or amphetamines as their principal drug of concern tended to have treatment episodes of a longer duration, compared to those receiving treatment for alcohol or cannabis, although treatment lengths for alcohol have increased in recent years (Figure Treatment 2).
- The decline in median episode length for cannabis between 2012–13 and 2015–16 has been affected by an increase in the number of diversion programs for people using cannabis (which had relatively shorter durations on average).
Figure Treatment 2: Closed treatment episodes provided, by selected principal drugs of concern and median duration, 2011–12 to 2015–16
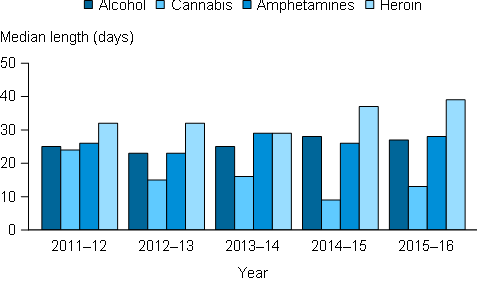
Source: AODTS NMDS. See Supplementary Table S2.


