Welfare workforce
Citation
AIHW
Australian Institute of Health and Welfare (2023) Welfare workforce, AIHW, Australian Government, accessed 27 July 2024.
APA
Australian Institute of Health and Welfare. (2023). Welfare workforce. Retrieved from https://www.aihw.gov.au/reports/australias-welfare/welfare-workforce
MLA
Welfare workforce. Australian Institute of Health and Welfare, 07 September 2023, https://www.aihw.gov.au/reports/australias-welfare/welfare-workforce
Vancouver
Australian Institute of Health and Welfare. Welfare workforce [Internet]. Canberra: Australian Institute of Health and Welfare, 2023 [cited 2024 Jul. 27]. Available from: https://www.aihw.gov.au/reports/australias-welfare/welfare-workforce
Harvard
Australian Institute of Health and Welfare (AIHW) 2023, Welfare workforce, viewed 27 July 2024, https://www.aihw.gov.au/reports/australias-welfare/welfare-workforce
Get citations as an Endnote file: Endnote

The welfare workforce comprises individuals in paid employment who directly provide welfare-related services. These services are provided by a diverse range of public and private organizations and encompass various areas, including care in residential aged care facilities and counselling and social assistance for students in educational settings. It is important to note that medical and healthcare services, as well as hospitality, are not included in the welfare workforce. In general, a formal definition for the welfare workforce used here is mentioned in defining the welfare workforce.
This page provides a broad summary of the welfare workforce, including its size, growth, and structural changes from 2012 to 2022, as well as notable features in 2022. It also highlights which occupations and industries within the welfare workforce experienced significant changes in their workforce during the period of 2012–2022.
Volunteering is also an important part of the welfare workforce, with a significant proportion of welfare-related services provided by adult Australians in an unpaid capacity (25% in 2020 (ABS 2021)) participating in this workforce. Volunteering in welfare-related services is separately reported and is not discussed on this page. For more information on volunteering, please see Volunteers and the Australian Bureau of Statistics (ABS) General Social Survey – summary results, Australia. Also see Philanthropy and charitable donations for more information on the volunteer workforce and voluntary financial contributions.
Defining the welfare workforce
The welfare workforce is difficult to quantify and study, particularly due to diverse range of roles and sectors involved. Overlapping responsibilities between education, social, and community assistance settings, as well as the mobility of workers between settings, further create challenges. Additionally, there is a lack of dedicated data collection focus on this professional group. Given these limitations, the AIHW uses data from the ABS Labour Force Survey (ABS 2023) and identifies individuals working in specific occupations and industries related to community services as the best approximation for the welfare workforce.
The AIHW derives estimates of the Australian welfare workforce, which encompasses individuals in community service occupations and working in community service industries. Community service occupations are defined from a group of 17 4-digit ANZSCO occupations, including age and disable carers, child carers and teachers in pre-school. Community service industries consist of a group of 4 3-digit ANZSIC industries: residential care services, childcare services, preschool education, and other social assistance services (see glossary).
This definition excludes some people in community service occupations who do not work in a community service industry. For example, a registered nurse working in a hospital would not be classified as part of the welfare workforce, though a registered nurse working in a residential aged care setting would be. Similarly, a teacher working in childcare or preschool would be included while a teacher working in a school would be excluded. According to the classification of ABS, teachers in preschool education only include those in purely preschool units, not those in units where pre-primary school education is provided in conjunction with normal primary school education.
Data presented on this page are based on sample survey data from the ABS and may be subject to errors arising from sampling or non-sampling issues. For more information on sample sizes, please refer to the ABS Labour Force, Australia methodology.
For more detailed information on the welfare workforce, including demographics, education attainment, earnings, and the impact of COVID-19, see 'Chapter 9 Welfare workforce: demand and supply' in Australia's welfare 2023: data insights.
Welfare workforce overview
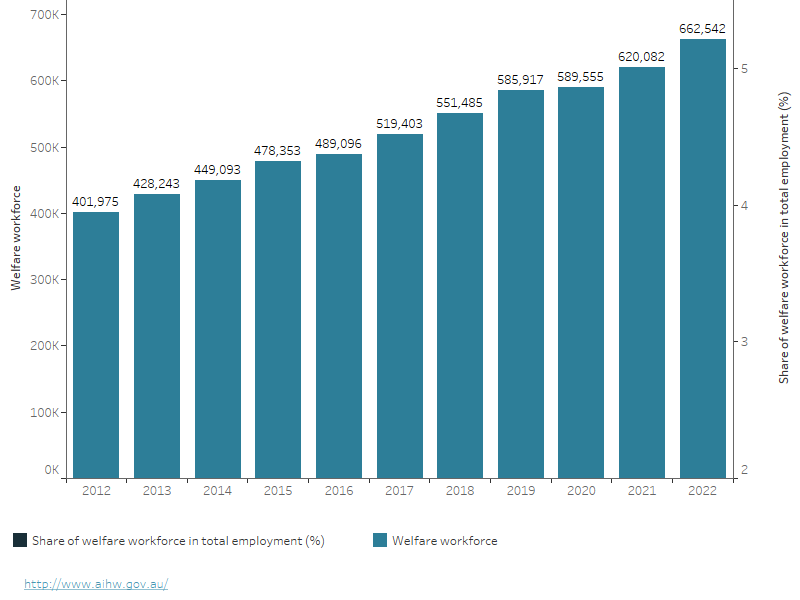
In 2022, the welfare workforce accounted for 4.9% of total employment; up from 3.6% in 2012 (Figure 1). Over the decade from 2012 to 2022, the welfare workforce in Australia grew by 65%, reaching over 662,542 people (Table 1). During the same period, the total employment increased by 20%.
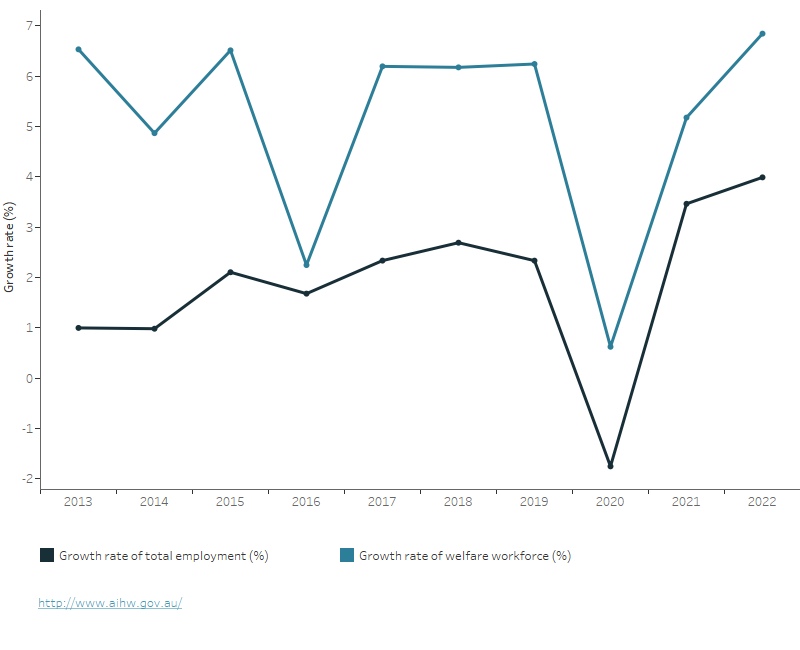
The welfare workforce's contribution to the growth of the total employment was approximately 11% for the period 2012 to 2022. The average annual growth rate of the welfare workforce was 5.1% while the growth rate of the total employment was 1.9% over this period. The highest growth level during this period was recorded in 2022, with an approximate increase of 7% (Figure 2).
| Community service occupations | Other occupations | Total | |
|---|---|---|---|
| Community service industries | 662,542 people employed in community service occupations in community service industries (for example, child care workers in the child care services industry)(a) | 242,704 people employed in other occupations in community service industries (for example, as administrators, accountants, tradespersons and labourers) | 905,246 |
| Other industries | 621,673 people employed in community service occupations in other industries (for example, nurses working in hospitals and counsellors in the education industry) | ||
| Total | 1,284,215 |
(a) People employed in community service occupations in community service industries (for example, childcare workers in the child care services industry) are considered to be the welfare workforce of Australia, for this page.
Note: Annual average of quarterly data from original series estimates.
Source: ABS 2023.
Figure 1: Welfare workforce proportion, 2012 to 2022
This graph displays the number of people employed in the welfare workforce over time, with values represented on the left axis, and the proportion of the welfare workforce in the total employment, with values indicated on the right axis. In 2012, the number of welfare workers was approximately 402,000, whereas in 2022, it increased to 663,000. The proportion of the welfare workforce in the total employment has shown an upward trend over time, rising from 3.6% in 2012 to 4.9% in 2022.
Source: ABS 2023.
Figure 2: Welfare workforce growth, 2013 to 2022
The figure shows the growth rate of the welfare workforce and the total employment over time. On average, from 2012 to 2022, the growth rate of the welfare workforce was approximately three percentage points higher than that of the total employment. In 2020, the growth level of the welfare workforce experienced a significant decline, with a growth rate of 0.6%. This was a sharp drop from the growth rate of 6.2% observed in 2019. Nevertheless, in the following two years, the growth rate of the welfare workforce once again increased sharply.
Source: ABS 2023.
Increase in welfare workforce driven by disability support and aged care services
Welfare workforce by industry
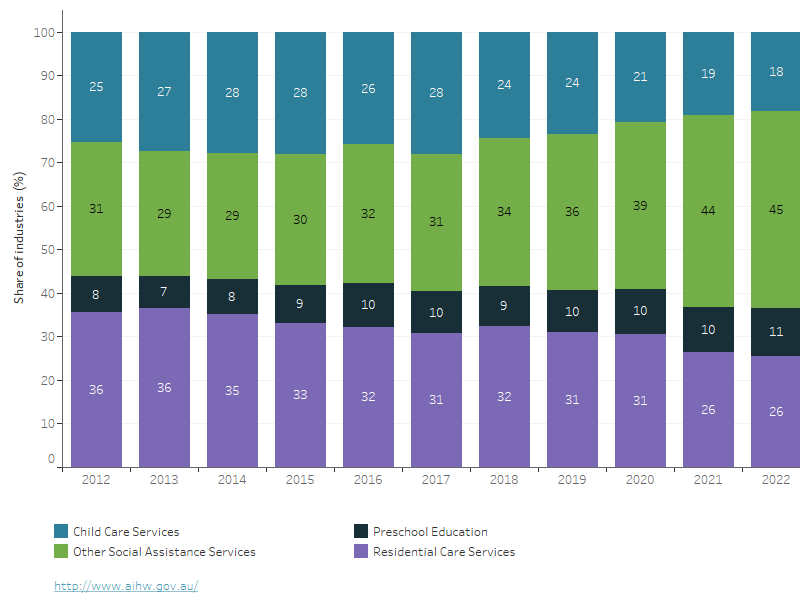
Changes in the structure of industries in the welfare workforce:
- The Other Social Assistance Services industry (ANZSIC-879), which includes disabilities and aged care services (excluding residential care services), continued to increase its share in the welfare workforce, reaching 45% in 2022 compared with 44% in the previous year. This industry has been the largest within the welfare workforce since 2018, when its share was 34%.
- The Residential Care Services industry, which was previously the largest with shares above 31% in previous years, began to decline from 2018 and reached 26% by 2022.
- The Preschool Education industry has been gradually increasing and had a share of 11% in 2022, which was one percentage point higher than in 2021, and 3 percentage points higher than in 2012.
- The Child Care Services industry experienced a decrease in recent years (Figure 3).
Figure 3: Share of industries in welfare workforce, 2012 to 2022
The figure illustrates changes in the proportion of each industry within the welfare workforce over time. Notably, the Other Social Assistance Services industry (ANZSIC-879), which provides services for the elderly and individuals with disabilities, has experienced a significant increase since 2018. Until 2017, this industry accounted for 31% of the welfare workforce. However, in 2018, this proportion increased to 34%, and by 2022, it had risen to 45%. These findings indicate that nearly half of the welfare workforce was employed in the Other Social Assistance Services industry in 2022, highlighting its growing importance in the welfare sector in recent years.
Note: refer to glossary for full list of inclusions for ‘Other Social Assistance Services’.
Source: ABS 2023.
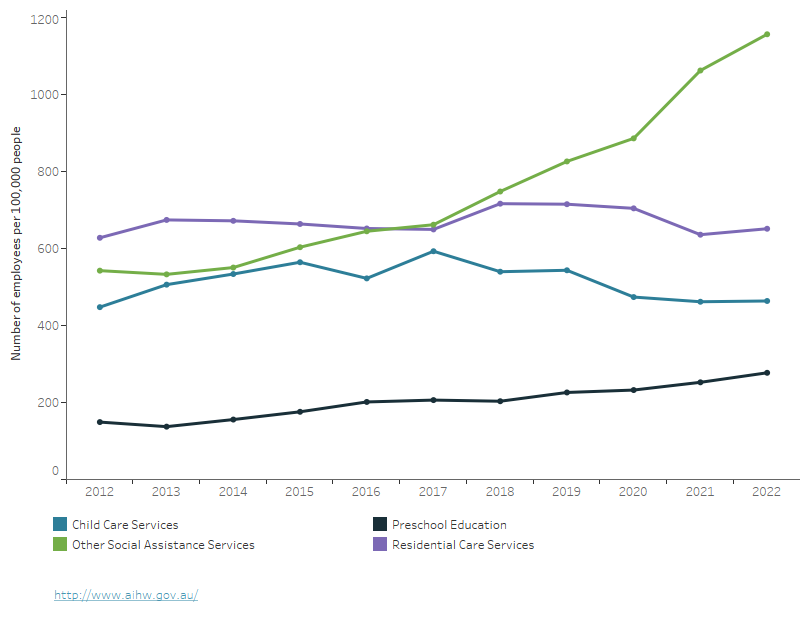
Changes in the number of employees of industries in the welfare workforce:
- The Other Social Assistance Services industry saw a significant increase in employment, with the number of employees in 2022 increasing by 113% from 2012 and 61% from 2018. The number of employees per 100,000 population increased from 543 in 2012, to 749 in 2018 and 1157 in 2022.
- Preschool Education saw an increase in the number of employees, with a rise of 86% from 2012 to 2022, or from 149 employees per 100,000 population to 277 employees, respectively.
- The number of employees per 100,000 population in the Child Care Services and Residential Care Services industries has decreased in recent years. In 2022, these industries had 464 and 652 employees per 100,000 population, respectively. Although these numbers were slightly higher compared to their respective levels of 462 and 636 in 2021, they remained lower than the peak levels observed in previous years, 593 in 2017 for Child Care Services and 717 in 2018 for Residential Care Services (Figure 4).
This decline can be attributed to a decrease in the overall number of employees within these industries. Specifically, the number of employees in the Child Care Services industry decreased from over 145,900 in 2017 to over 120,500 in 2022. Similarly, the number of employees in the Residential Care Services industry decreased from over 178,900 in 2018 to over 169,300 in 2022.
Figure 4: Welfare workforce per 100,000 population for industries, 2012 to 2022
The figure illustrates the number of welfare workers per 100,000 population across various industries in the welfare workforce. The data shows a significant increase in employment in the Other Social Assistance Services industry compared to other sectors since 2018. Although prior to 2018, the workforce in this industry was lower than that of Residential Care Services, from 2018 onwards, employment in Other Social Assistance Services surpassed that of Residential Care Services. In 2022, the number of workers in Other Social Assistance Services was 1,157 per 100,000 population, while that in Residential Care Services was 652. Employment in Preschool Education has also been on the rise, increasing from 149 workers per 100,000 population in 2012 to 277 workers per 100,000 population in 2022. The numbers in the other industries did not change significantly.
Source: ABS 2023.
Welfare workforce by occupation
Changes in the structure of occupations in the welfare workforce:
- In 2022, the occupation structure of the welfare workforce continued to shift towards the Aged and Disabled Carers occupation (ANZSCO-4231). The proportion of employees in this occupation increased to 40% of the welfare workforce, up from 37% in 2021 and 25% in 2012. The Aged and Disabled Carers' share of the welfare workforce began to expand in 2019 when it was at 31%.
- In contrast, the Child Carers occupation had shares almost similar to that of the Aged and Disabled Carers before 2018, but its share has since decreased. As of 2022, the Child Carers' share was 19%, less than half of the Aged and Disabled Carers' share.
- Among occupations with smaller shares, only Early Childhood Teachers saw an increasing trend in recent years, with a share of 8% in 2022 (Figure 5).
Figure 5: Share of occupations in welfare workforce, 2012 to 2022
The figure depicts changes in the occupational composition of the welfare workforce over time. Between 2012 and 2019, the proportion of Aged and Disabled Carers (ANZSOC-4231) increased by an average of 1 percentage point per year. However, starting in 2019, there was a significant increase in this occupation's proportion, with an average annual increase of over 2 percentage points. From 2012 to 2019, the share of employment in the Aged and Disabled Carers occupation increased from 25% to 29%, but by 2022, this proportion had risen to 40%. In addition, the share of Early Childhood Teachers in the welfare workforce increased from 5% in 2012 to 8% in 2022.
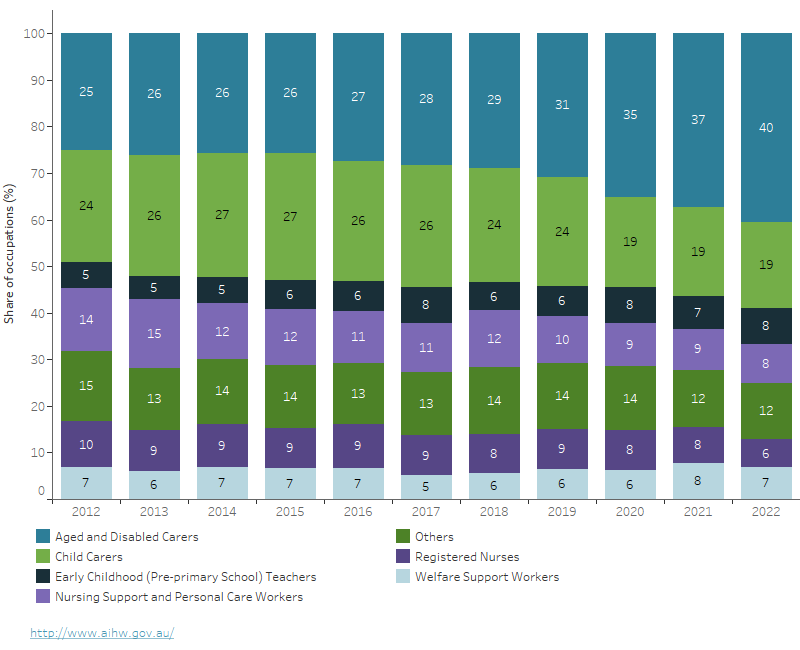
Note: 'Others' represents a combination of occupations with relatively small shares in the welfare workforce. These include Counsellors; Enrolled and Mothercraft Nurses; Other Community Service Occupations; Psychologists; Social Workers; and Welfare, Recreation and Community Arts Workers.
Source: ABS 2023.
Changes in the number of employed people in the welfare workforce occupations:
- The Aged and Disabled Carers' number of employees in 2022 increased by 166% since 2012, and by 49% since 2019. The number of employees in this occupation increased from 444 per 100,000 population in 2012 to 712 in 2019, and 1,032 in 2022.
- The Aged and Disabled Carers occupation had an average employment growth rate of 13% between 2019 and 2022, compared to 6.2% between 2012 and 2018. Additionally, the number of employees in Early Childhood (Pre-primary School) Teachers (another occupation with a relatively stable increase over time), increased from 96 to 195 per 100,000 population between 2012 and 2022 (Figure 6).
To sum up, the increase in employment in the Aged and Disabled Carers occupation (ANZSCO-4231) and the Other Social Assistance Services industry (ANZSIC-879) was the primary driver of growth in the welfare workforce from 2012 to 2022, accounting for 51% of the growth. Meanwhile, during the COVID-19 pandemic period from 2020 to 2022, this workforce contributed to 106% of the growth in the welfare workforce.
Figure 6: Welfare workforce per 100,000 population for occupations, 2012 to 2022
The shows the number of workers per 100,000 population for each occupation in the welfare workforce. Aged and Disabled Carers (ANZSOC-4231) experienced a significant increase from 2019. In 2018, this occupation had 638 workers per 100,000 population, but by 2019, it had risen to 712 workers and by 2022, it had further increased to 1032. On the other hand, Child Carers, another major occupation in the welfare workforce, experienced a slow increase or stability until 2019, but then decreased from 545 workers per 100,000 population in 2019 to 442 workers per 100,000 population in 2020. By 2022, the number had slightly increased to 474 workers per 100,000 population. Among the smaller occupations in the welfare workforce, Early Childhood Teachers increased from 96 to 195 workers per 100,000 population. The remaining occupations remained relatively stable over time. These variations are consistent with the structure shown in Figure 5.
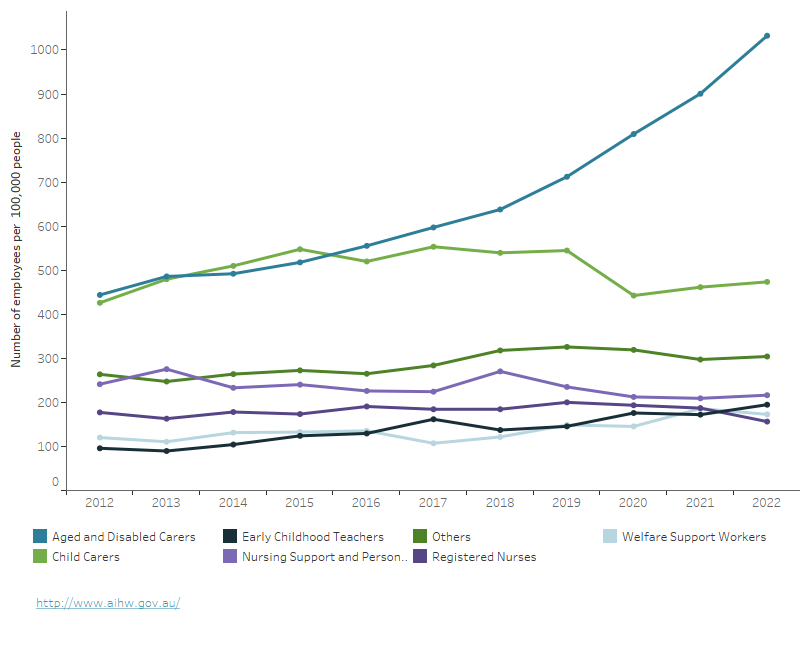
Note: "Others" represents a combination of occupations with relatively small shares in the welfare workforce. These include Counsellors; Enrolled and Mothercraft Nurses; Other Community Service Occupations; Psychologists; Social Workers; and Welfare, Recreation and Community Arts Workers.
Source: ABS 2023.
Employment status, demographics, and educational attainment for the welfare workforce
The welfare workforce has distinct characteristics compared with the overall employment, including a higher proportion of females, part-time jobs, an older average age, and lower educational attainment. In 2022, there was a significant increase in the number of employment in occupations or industries related to aged and disabled care, continuing the trend from previous years. As a result, the characteristics of the welfare workforce continued to change compared with those of the overall employment.
- In 2022, the proportion of people working part time (see glossary) in the welfare workforce was 49%, which was slightly lower than the 51% recorded in 2012 and the 53% recorded in 2021. In comparison, the proportion of people employed part time in the overall employment was 31% in 2022, representing a slight increase from 30% in 2012.
- In 2022, women made up 83% of the welfare workforce in Australia, a decrease from 88% in 2012. This trend contrasts with the representation of women in the whole employment, which increased from 46% in 2012 to 48% in 2020.
- The proportion of workers under 34 in the welfare workforce increased from 35% in 2012 to 38% in 2022, while this proportion decreased in the overall employment (39% in 2012 and 38% in 2022). The average age of the welfare workforce decreased from 41.05 years in 2012 to 40.7 years in 2022, while the average age of the overall workforce increased from 40.0 in 2012 to 40.7 in 2020.
- The proportion of Aboriginal or Torres Strait Islander (First Nations) people in the welfare workforce was 2.3% in 2022, which was a decrease from 2.6% in 2012. This proportion, however, is a slight increase in the overall workforce from 1.2% in 2012 to 1.3% in 2022.
- The proportion of welfare workers with a bachelor degree or higher increased from 21% in 2012 to 32% in 2022, which is quite similar to the increase in the overall employment (25% to 36%).
- In 2022, the proportion of overseas-trained migrant workers was 12.2%, which slightly increased from 11.7% in 2016. Comparatively, the proportion of these workers in overall employment was 10.0% in 2016 and 10.5% in 2022.
For more information, see 'Chapter 9 Welfare workforce: demand and supply' in Australia’s welfare 2023: data insights. This chapter provides a detailed analysis of Australia’s welfare workforce, including demographics, employment status, educational attainment, earnings, and the impacts of the COVID-19 pandemic on the welfare workforce.
Where do I go for more information?
For more information on the Australian workforce, see:
ABS (Australian Bureau of Statistics) (2021) General Social Survey: Summary Results, Australia, 2020, ABS, Australian Government, accessed 26 May 2023.
ABS (2023) Labour Force Survey, ABS, Australian Government, accessed 26 May 2023.
JSCNDIS (Joint Standing Committee on the National Disability Insurance Scheme) (2020) NDIS Workforce interim report General Social Survey: Summary Results, Australia, 2020, Parliament of Australia, Australian Government, accessed 26 May 2023.


