Burden among Indigenous Australians
Due to the very small number of cases of some vaccine preventable diseases (VPD), it was not possible to produce estimates for Indigenous Australians of the burden of all 17 diseases covered under the Australian National Immunisation Program schedule.
Estimates of the burden among Indigenous Australians are provided for 13 VPD: chickenpox, haemophilus influenzae type b (Hib), hepatitis A, hepatitis B, human papillomavirus (HPV), influenza, measles, meningococcal disease, mumps, pneumococcal disease, rotavirus, shingles and whooping cough.
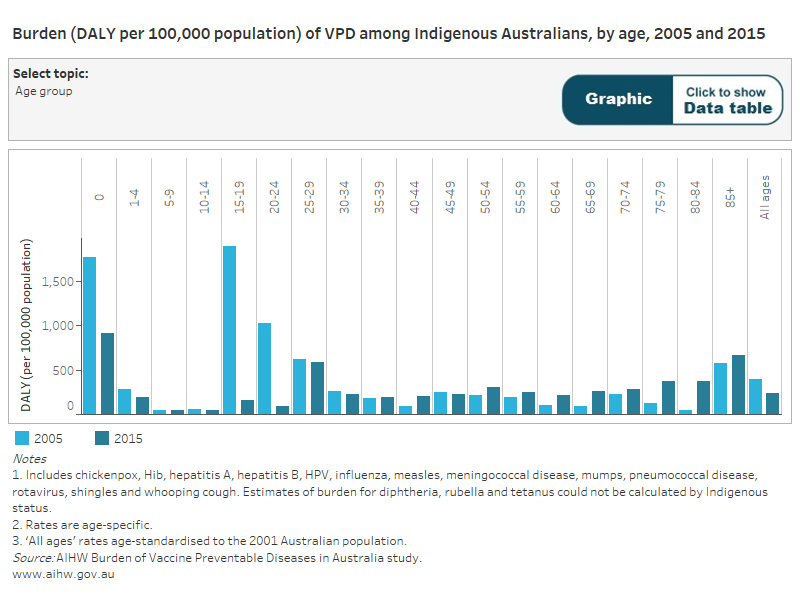
As a group, the 13 VPD noted above were responsible for 1,552 DALY among Aboriginal and Torres Strait Islander people in 2015 (237 DALY per 100,000 population). Premature loss of life accounted for 85% of the total burden of VPD among Indigenous Australians.
Between 2005 and 2015, the age-standardised rate of burden among Indigenous Australians decreased by 41%, largely due to a decrease in the burden due to HPV. Decreases in the rate of burden between 2005 and 2015 were also seen for hepatitis A, rotavirus, Hib, meningococcal disease, hepatitis B and chickenpox. Vaccines for some of these disease were added to, or vaccine eligibility extended on, the NIP schedule during the past 20 years.
Which VPD caused the most burden among Indigenous Australians?
The top 3 contributors to the VPD burden among Indigenous Australians in 2015 were:
- HPV (39%)
- pneumococcal disease (30%)
- influenza (15%).
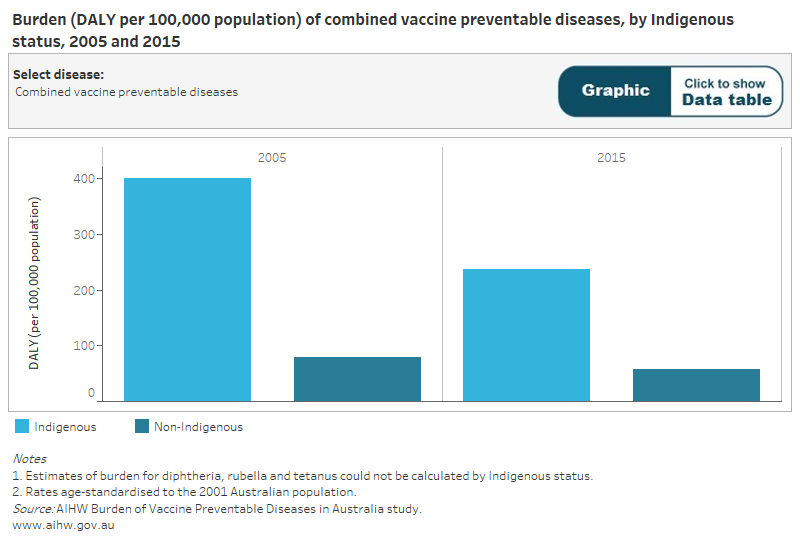
Gap in VPD burden between Indigenous and non-Indigenous Australians
In 2015, VPD among Indigenous Australians accounted for 10% of the burden due to the 13 specified VPD. After adjusting for differences in population age structure, the Indigenous burden rate was 4.1 times that for non-Indigenous Australians.
In 2015, HPV and pneumococcal disease had the largest absolute differences between Indigenous and non‑Indigenous rates. Although HPV infection rates are similar for Indigenous and non-Indigenous women, the higher incidence of cervical cancer and poorer survival rates among Indigenous women result in a greater burden associated with HPV.