Summary
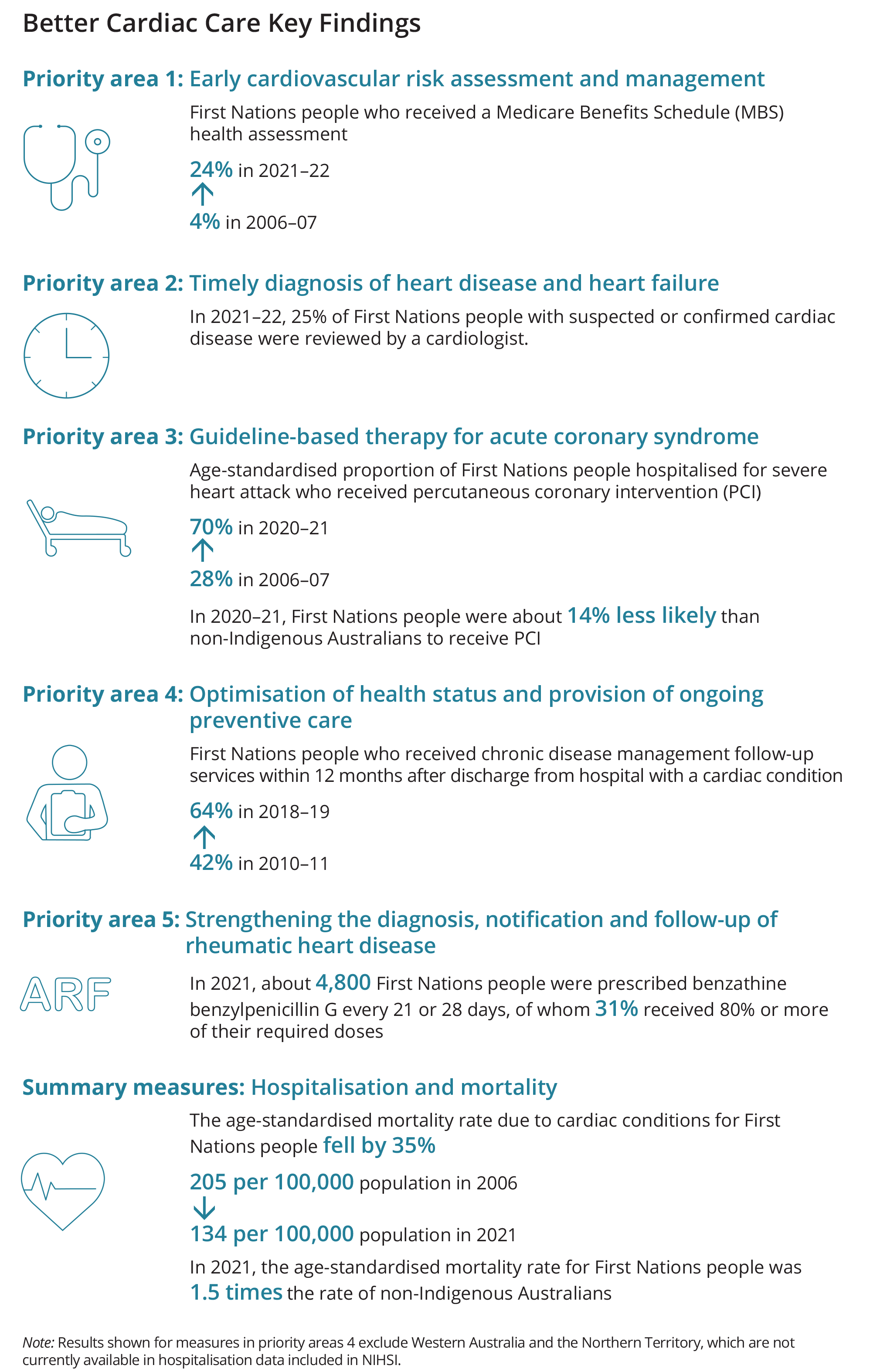
The Better Cardiac Care for Aboriginal and Torres Strait Islander People project is an initiative of the former Australian Health Ministers’ Advisory Council. It aims to reduce deaths and ill health from cardiac conditions among Aboriginal and Torres Strait Islander (First Nations) people.
Five priority areas comprising 21 measures were developed to monitor the progress of the project. In this eighth national report, 12 measures in the earlier reports are updated and 5 new measures are included. New measures included for the first time are from the National Integrated Health Services Information (NIHSI) on ongoing preventive care and medication adherance for patients discharged from hospital with cardiac condtions (Measures 3.4, 4.1, 4.2, 4.3, 4.4). Measure 1.3 could not be updated as newer data are not available to report. Measure 5.4 has not been reported since the 2018–19 report due to issues with data quality.
Figure 1: Summary infographic
Summary
- Key findings
1. Introduction
- Better Cardiac Care project
- Reporting on the Better Cardiac Care measures
- Data development plan
2. Results
- Priority area 1: Early cardiovascular risk assessment and management
- Measure 1.1: Annual health assessments
- Measure 1.2: Cardiovascular disease risk assessment
- Measure 1.3: Primary care practitioner follow-up
- Priority area 2: Timely diagnosis of heart disease and heart failure
- Measure 2.1: Cardiac-related diagnostic services
- Measure 2.3: Suspected or confirmed cardiac disease case reviewed by a cardiologist
- Priority area 3: Guideline-based therapy for acute coronary syndrome
- Measure 3.1: ST-segment-elevation myocardial infarction events treated by percutaneous coronary intervention
- Measure 3.3: Acute coronary syndrome events that included diagnostic angiography or definitive revascularisation
- Measure 3.4: ACS patients discharged from hospital on appropriate secondary prevention medicines
- Measure 3.5: Acute myocardial infarction in-hospital mortality rates
- Priority area 4: Optimisation of health status and provision of ongoing preventive care
- Measure 4.1: Review by a primary health-care professional after discharge from hospital with a cardiac condition
- Measure 4.2: Chronic Disease Management services after discharge from hospital with a cardiac condition
- Measure 4.3: Specialist physician review after discharge from hospital with a cardiac condition
- Measure 4.4: Patients with coronary heart disease discharged on secondary prevention medications
- Priority area 5: Strengthening the diagnosis, notification and follow-up of rheumatic heart disease
- Measure 5.1: Annual incidence of acute rheumatic fever and rheumatic heart disease
- Measure 5.2: Recurrent acute rheumatic fever
- Measure 5.3: Preventive treatment with benzathine benzylpenicillin G
- Summary measures: Hospitalisation and mortality
- Measure 6.1: Hospitalisations for cardiac conditions
- Measure 6.2: Deaths due to cardiac conditions
Appendixes
- Appendix A: Data sources
- ABS 2018–19 National Aboriginal and Torres Strait Islander Health Survey
- Proxy measures for primary care practitioner follow-up
- Medicare Benefits Schedule data
- Coverage of Medicare Benefits Schedule data
- Demographic information
- Indigenous identification
- Health assessments for First Nations and non-Indigenous Australians
- Estimate of people with a cardiac condition from Medicare Benefits Schedule data
- National Hospital Morbidity Database
- Indigenous identification
- Estimation of hospitalised episodes for Priority area 3 measures
- State and territory comparisons for Priority area 3 measures
- National Integrated Health Services Information (NIHSI)
- Admitted Patient Care (APC) data
- Medicare Benefits Schedule (MBS) data and the Pharmaceutical Benefits Scheme (PBS)/Repatriation Pharmaceutical Benefits Scheme (RPBS) data
- National Death Index (NDI) data
- Patient Demography data
- National Key Performance Indicators data collection
- National Mortality Database
- Indigenous identification
- National Rheumatic Heart Disease data collection
- Calculations of ARF recurrences per 100 patient-years
- Aboriginal and Torres Strait Islander population
- ABS 2018–19 National Aboriginal and Torres Strait Islander Health Survey
- Appendix B: Technical specifications
- Appendix C: Summary results, by measure
End matter: Acknowledgements; Abbreviations; Symbols; Glossary; References; List of tables; List of figures