Medicare-subsidised palliative medicine attendance and case conference services
On this page:
In 2021–22, 14,500 people received 69,100 Medicare Benefits Schedule (MBS)-subsidised palliative medicine attendance and palliative medicine case conference services provided by palliative medicine physicians/specialists. This section provides information related to these services and the characteristics of the people who received them (see Data sources section for further information on these services).
The information in this section was last updated in May 2023.
The data presented in this section relate only to palliative medicine attendances/consultations and case conferencing services that are both provided by palliative medicine physicians/specialists and are claimed under specialist palliative care MBS item numbers. Information is also provided on the settings where the attendances were provided – in hospital/consulting room or in other settings (such as a person’s place of residence, including home, residential aged care or institution). For case conferencing, it refers to community case conference and discharge case conference. For further details on the MBS items included on this page refer to the Data sources: Medicare Benefits Schedule (MBS) data.
Patients who are referred to specialists or physicians in palliative medicine usually have:
- intermediate and fluctuating needs that might result in unplanned use of hospital and other services, and/or
- complex and persistent needs (physical, social, emotional, or spiritual) that are not effectively managed through established protocols (PCA 2018).
It should be noted that a patient may access more than one type of these specific MBS items provided by palliative medicine physicians/specialists during the reporting period and that each service is counted separately in this report.
Palliative care physicians/specialists may at times use other MBS item numbers when attending to palliative care patients. These items are not included in the data on this page, as they are not claimed specifically as a palliative care-related service under the MBS. Further, other medical practitioners (general practitioners and medical specialists) and health professionals also attend to terminally ill patients and provide palliative care, without the service being eligible to be claimed specifically as a palliative care-related service under the MBS.
In other words, the reported number of patients who receive a palliative care-related service under the MBS is a known underestimate of total palliative care activity. Further, the data does not include referred attendances by palliative medicine physicians/specialists to: public patients in public hospitals; public hospital outpatients; or patients covered by Department of Veterans’ Affairs arrangements.
The MBS data presented in this section (2021–22 and trend data) are based on the date the service was provided rather than the date of service processing, as this more accurately reflects the date an attendance occurred. Note that in reports released prior to 2022, the data was based on the date the service was processed by Services Australia and as a result the data presented in the 2022 and 2023 releases are not comparable with previous releases.
Key points
- 69,100 services were provided, at a national rate of 270 services per 100,000 population
- 14,500 people received these services, at an average of 4.8 services per person
- 3 in 4 (77%) were provided to people aged 65 and over, including 23% for those aged 85 years and over
- those living in Major cities were 3.4 times as likely to receive these services as those living in Remote and very remote areas combined (62 compared with 18 per 100,000 population, respectively)
- 4 in 5 services (55,900 or 81%) were for attendances in a consulting room or hospital, 6.3% (4,300) were for attendances in other settings and 13% (8,900) were for case conferences
- $5.6 million was paid in benefits for these services, at an average of $390 per patient.
Data downloads
Who received these services?
In 2021–22, 14,500 people received at least one MBS-subsidised palliative medicine attendance or case conference service provided by palliative medicine physicians/specialists, at a rate of 56 people per 100,000 population. Among people receiving these services (Figure MBS.1):
- Slightly more were males – 7,300 males compared with 7,200 females (or 57 compared with 55 per 100,000 population, respectively).
- 3 in 4 (77%) were aged 65 and over – the population rate increased steeply from age 55, from 65 to 617 per 100,000 between the age groups 55–64 and 85 and over. Only 4 in 100 (4.0%) were aged under 45.
- Those living in Major cities were 3.4 times as likely to receive these services as those living in Remote and very remote areas – 62 per 100,000 population in Major cities compared with 18 per 100,000 in Remote and very remote areas combined. It should be noted that the vast majority of employed palliative medicine physicians and nurses work in Major cities (see Palliative care workforce for further details).
- Queensland had the highest population rate at 73 per 100,000 population, followed by Western Australia (71 per 100,000 population) and Australian Capital Territory and Northern Australia had the lowest at 15 per 100,000 population.
- The population rates varied across the Primary Health Network (PHN) areas, ranging from 6.4 per 100,000 in New South Wales Nepean Blue Mountains PHN area to 169 per 100,000 population in the Northern Sydney PHN area (Table MBS.2).
Figure MBS.1: People who received MBS-subsidised palliative medicine attendance and/or case conference services provided by palliative medicine physicians/specialists, 2021–22
Figure 1.1: This interactive data visualisation shows the number and rate (per 100,000 population) of people receiving MBS-subsidised palliative medicine attendance and/or case conference services provided by palliative medicine physicians/specialists by sex in 2021–22. The number and rate (per 100,000 population) of males receiving these services were slightly higher than females.
Figure 1.2: This interactive data visualisation shows the age distribution of people receiving MBS-subsidised palliative medicine attendance and/or case conference services provided by palliative medicine physicians/specialists, both the number and rate (per 100,000 population) in 2021–22. The number of people receiving these services increased with age to age 75–84 and then declined for those aged 85 and over. The age-specific rate (per 100,000 population) of people receiving these services also increased steeply with age, with the highest rate for those aged 85 and over.
Figure 1.3: This interactive data visualisation shows the number and rate (per 100,000 population) of people receiving MBS-subsidised palliative medicine attendance and/or case conference services provided by palliative medicine physicians/specialists by remoteness areas of usual residence in 2021–22. Major Cities had the highest number and rate (per 100,000 population) of people receiving these services.
Figure 1.4: This interactive data visualisation shows the number and rate (per 100,000 population) of people receiving MBS-subsidised palliative medicine attendance and/or case conference services provided by palliative medicine physicians/specialists by states and territories in 2021–22. New South Wales had the highest number of people receiving these services, while Northern Territory had the lowest. Queensland had the highest rate of people (per 100,000 population) receiving these services while Australian Capital Territory had the lowest.

How many services were provided?
In 2021–22, 69,100 MBS-subsidised palliative medicine attendance and case conference services were provided by palliative medicine physicians/specialists, at an average of 4.8 services per person. Among these services (Figure MBS.2):
- Males and females received similar number of services, on average – 4.7 and 4.8 services per males and females, respectively.
- The number of services per person was relatively similar for those aged 25 and over – ranging from 4.4 to 5.3, except for those aged 35–44 where it dipped to 3.4 services per person, which was the same as that for those aged 15–24. For those aged under 15, the number of services per person was considerably lower, at 1.3 services per person.
- 4 in 5 services were for attendances/consultations in a consulting room or hospital – 55,900 or 81% with a further 6.3% (4,300) for consultations in other settings (such as in person’s place of residence) and 13% (8,900) for case conferences.
- People living in Major cities were 4 times as likely to receive attendance services and 12 times as likely to receive case conference services than those living in Remote and very remote areas combined (264 vs 60 per 100,000 for attendances and 42 vs 3.7 per 100,000 for case conferences). The average number of services for attendances was also higher for those in Major cities than in other areas (5.6 declining to 3.5 in Remote and very remote areas), while for case conferences, the number of services were relatively similar across remoteness areas (1.4–1.8 services per person).
- Western Australia had the highest population rate of services, including for attendances, almost double the national average rate – 480 and 268 per 100,000 and 442 and 234 per 100,000 population for attendances, respectively. The Australian Capital Territory had the lowest rate of services (34 per 100,000 population). The highest rate for case conferences was recorded in Queensland (48 per 100,000 population), and the lowest rate was in South Australia (1.2 per 100,000 population). Note that data for palliative medicine attendances and palliative medicine case conferences in Tasmania, Australian Capital Territory and Northern Territory are not presented due to small numbers (see Table MBS.4).
Figure MBS.2: MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists, 2021–22
Figure 2.1: This interactive data visualisation shows the number, rate (per 100,000 population) and services per person of MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists, by sex in 2021–22. The number and rate (per 100,000 population) of these services for males were slightly higher than females. While the services per person was slightly higher in females compared to males.
Figure 2.2: This interactive data visualisation shows the age distribution of MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists, including number, rate (per 100,000 population) and services per person in 2021–22. The number of these services increased with age to age 75–84 and then declined for those aged 85 and over. The age-specific rate (per 100,000 population) of these services also increased steeply with age, with the highest rate of services for those aged 85 and over. The highest number of services per person was for age 55-64 years.
Figure 2.3: This interactive data visualisation shows the number and proportion of MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists by MBS item groups in 2021–22. Attendance in a consulting room or hospital was the most common MBS item for palliative medicine attendances, while organising and coordinating a discharge case conference was the most common MBS item for palliative medicine case conferences.
Figure 2.4: This interactive data visualisation shows the number, rate (per 100,000 population) and services per person of MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists, by service group and remoteness areas of usual residence in 2021–22. Major cities had the highest number and rate (per 100,000 population) of palliative medicine attendances and case conferences, followed by Inner regional areas. Major cities had the highest services per person for the palliative medicine attendances and Outer regional areas had the highest services per person for the palliative medicine case conferences.
Figure 2.5: This interactive data visualisation shows the number, rate (per 100,000 population) and services per person of MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists, by service group and states and territories in 2021–22. Queensland had the highest number of services for palliative medicine attendances and New South Wales had the highest number of services for palliative medicine case conferences. Western Australia had the highest rate (per 100,000 population) of services for palliative medicine attendances and Queensland had the highest rate (per 100,000 population) of services for palliative medicine case conferences. Western Australia had the highest number of services per person for palliative medicine attendances and case conferences.

How have these services changed over time?
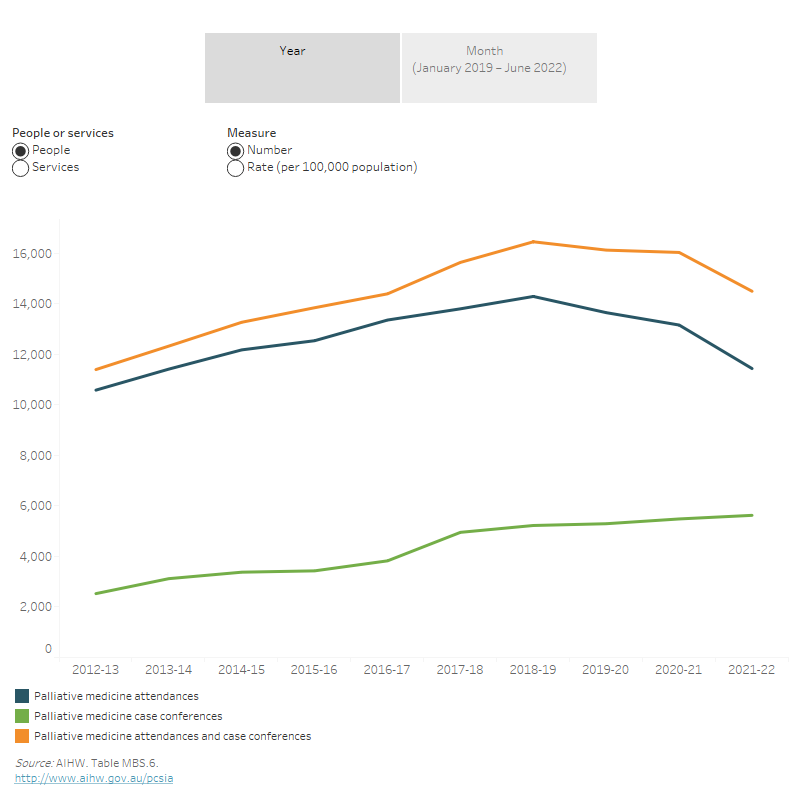
The number of people receiving MBS-subsidised palliative medicine attendances and case conferences increased between 2012–13 and 2018–19 (44% increase, or from 11,400 to 16,500 people), remained relatively stable in 2019–20 and 2020–21, and then declined by 9.6% in the 12 months to 2021–22 to 14,500 (Figure MBS.3). This equates to an increase of 50 to 65 per 100,000 people receiving these services between 2012–13 to 2018–19 and then declining to 56 per 100,000 in 2021–22, which was similar to the rate in 2014–15. This was broadly consistent with the pattern observed for the number of services for palliative medicine attendances and case conferences over this period – increasing from 63,900 to 90,600 (42% increase) between 2012–13 and 2018–19, before declining by 7% in each of the following 2 years and then declining steeper by 12% in the 12 months to 2021–22.
These patterns were driven by trends in the number of people receiving palliative medicine attendances (35% increase between 2012–13 and 2018–19 and 13% decline in 12 months to 2021–22), given that these services accounted for the vast majority (87%) of palliative medicine attendance and case conference services in 2021–22. For case conferences a different pattern emerged, with the number of people receiving case conferences increasing each year – more than doubling from 2,500 to 5,600 or increasing from 11 to 22 per 100,000 population between 2012–13 and 2021–22. This steep increase in case conferences resulted in the number of people receiving palliative medicine attendances declining from 92% to 87% of all palliative medicine attendance and case conference services over this period.
The decline in services for palliative medicine attendances in the 4 years to 2021–22, differed from the trend observed for all specialist attendances (including palliative medicine specialists/physicians) which had increased each year, except for a slight fall in 2021–22 (5.1% decline for palliative medicine specialists/physicians and 4.1% decline for all specialists). The decline in palliative medicine attendance services since 2018–19 may reflect the increasing use of telehealth services by palliative medicine physicians/specialists in recent years – increasing from 4,900 in 2019–20 to 14,700 in 2021–22, or a total of 30,900 services over this period (refers to all attendances provided by palliative medicine physicians/specialists, not just those for specialist palliative care). It may also reflect that palliative medicine specialists/physicians are increasingly using other MBS items – in 2012–13, 84% of attendance services from palliative medicine specialists/physicians were claimed to palliative medicine attendances, which had declined steeply to 48% in 2021–22 (Table MBS.6).
The large falls in people receiving palliative medicine attendances or case conferences since 2019–20 may also reflect the effect of the public health measures (such as lockdowns and restrictions) to contain the spread of the coronavirus and its variants during 2020 and 2022. Coinciding with these measures, the number of people receiving palliative medicine attendances fell steeply, more so than for all specialist attendances. Compared with the corresponding months in 2019, the number of people receiving palliative medicine attendance and/or case conference services fell in April 2020 (by 33%), in May (by 23%), in August–October 2020 (by 21–23%), in October 2021 (by 30%), with even larger falls in January 2022 (by 39%) and April 2022 (by 38%). While for people receiving all specialist attendances the levels only dipped below 2019 levels and with more modest falls in March–May 2020 (3.0%–17% lower), August 2020 (2.6% lower), and in January 2022 (8.8% lower) and April 2022 (3.6% lower; Table MBS.7). For more information see: Impacts of COVID-19 on Medicare Benefits Scheme and Pharmaceutical Benefits Scheme (AIHW 2022).
Figure MBS.3: Trends in MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists and people receiving them, 2012–13 to 2021–22
Figure 3.1: This interactive data visualisation shows the number and rate (per 100,000 population) of MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists and people receiving them by service group each year between 2012–13 and 2021–22. It showed that the number and rate (per 100,000 population) of palliative medicine attendances and people receiving them increased between 2012–13 and 2018–19 and then declined to 2020–21 and 2021–22. However, palliative medicine case conferences and people receiving them gradually increased between 2012–13 and 2021–22.
Figure 3.2: This interactive data visualisation shows the number and rate (per 100,000 population) of MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists and people receiving them by service group each month from January 2019 to June 2022. It showed that the number of palliative medicine attendances and case conferences and people receiving them had the largest drop between March and April 2020 and a second largest drop in January and April 2022. While the number of palliative medicine attendances and case conferences and people receiving them increased between April 2020 and March 2021.
How much was spent on these services?
The Australian Government’s expenditure through the MBS for palliative medicine attendances and case conferences provided by palliative medicine physicians/specialists are based on allocating a unique item number to each service, as well as indicating the scheduled payment amount (see Medicare Benefits Schedule Book (DHAC 2022) for further details).
In 2021–22, for these MBS-subsidised palliative medicine attendances and case conferences:
- over $5.6 million was paid in benefits, equivalent to an average of $389 per patient; 81% of these benefits were for palliative medicine attendances (Table MBS.8)
- the benefits paid accounted for 0.2% of benefits paid for all MBS-subsidised specialist attendances ($2.8 billion; Table MBS.7)
- Northern Territory had the highest average benefits per patient at $639, followed by Western Australia ($513 per patient), while the Australian Capital Territory had the lowest average benefits per patient ($200). This was largely consistent with the rate of services in each state and territory, where Western Australia had the highest (480 per 100,000) and Australian Capital Territory had the lowest service rate (34 per 100,000; Figure MBS.4).
Trends
Between 2012–13 and 2018–19, MBS benefits paid for palliative medicine attendance and palliative medicine case conference services increased by 51% (from $4.7 million to $7.1 million) and then declined by 21% in 2021–22 ($5.6 million). However, after adjusting for inflation, this represented a 35% increase in the 6 years to 2018–19 (from $5.6 million to $7.6 million) and a 26% decline in the 3 years to 2021–22 (Figure MBS.4).
A similar pattern was also observed for benefits paid for palliative medicine attendances – 45% increase between 2012–13 to 2018–19 (from $4.2 million to $6.0 million) and then declining by 24% to reach $4.6 million in 2021–22. For case conferences, the growth was steeper and decline slower over this period – benefits paid doubled between 2012–13 and 2017–18 (from $547,400 to $1.17 million) and then fell slightly by 8.9% in 2021–22 ($1.06 million).
These patterns were broadly consistent with that for MBS benefits paid for all specialist attendances, except benefits increased each year between 2012–13 and 2020–21 (47% increase over this period) and then fell slightly by 2.9% in 2021–22 (Table MBS.9).
In terms of average benefits paid per person, this had declined since 2018–19 for palliative medicine attendances (from $365 to $316 per person; Figure MBS.4). In contrast, average benefits per person for case conferences had increased over this period, consistent with the patterns observed for all specialist attendances (Table MBS.9). These patterns reflected the trends in people/services reported in the previous section.
Figure MBS.4: Benefits paid for MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists, 2021–22
Figure 4.1: This interactive data visualisation shows the benefits ($) and average benefits per patient ($) for MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists across the Australia’s states and territories in 2021–22. Queensland had the highest benefits ($) for palliative medicine attendances, and New South Wales had the highest benefits ($) for palliative medicine case conferences. Western Australia had the highest average benefit per patient ($) for palliative medicine attendances and Victoria had the highest average benefit per patient ($) for palliative medicine case conferences.
Figure 4.2: This interactive data visualisation shows the benefits in current prices ($), benefits in real terms ($) and average benefits ($) for patients for MBS-subsidised palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists, by service groups between 2012–13 and 2021–22. It showed that benefits in current prices ($) and benefits in real terms ($) for palliative medicine attendances increased between 2012–13 and 2018–19 and then dropped between 2020–21 and 2021–-22. Whereas benefits in current prices ($) and benefits in real terms ($) slightly declined for the palliative medicine case conferences between 2017–18 and 2021–22, after initial increase between 2012–13 and 2017–18. Average benefits ($) for patients slightly declined for palliative medicine attendances despite fluctuations between 2012–13 and 2017–18. While average benefits ($) for patients gradually increased from $48 to $73 for case conferences during the same period.
AIHW (Australian Institute of Health and Welfare) (2022) Impacts of COVID-19 on Medicare Benefits Scheme and Pharmaceutical Benefits Scheme: quarterly data, Canberra: AIHW, Australian Government, accessed 10 February 2023.
DHAC (Department of Health and Aged Care) (2022) Medicare Benefits Schedule Book, operating from 1 July 2022, Canberra: Department of Health and Aged Care, Australian Government, accessed 30 January 2023.
PCA (Palliative Care Australia) (2018) Palliative Care Service Development Guidelines, Canberra: Palliative Care Australia.
Medicare Benefits Schedule data
Services Australia (formerly the Australian Government Department of Human Services) collects administrative data in processing claims for benefits under the Medicare Benefits Schedule (MBS) and provides this information to the Australian Government Department of Health and Aged Care. Information collected includes the type of service provided (MBS item number) and the benefit paid by Services Australia for the service. The item number and benefits paid by Services Australia are based on the Medicare Benefits Schedule Book (DHAC 2022).
Table 1: List of all MBS items that have been defined as palliative medicine attendance and case conference services provided by palliative medicine physicians/specialists
|
MBS item |
MBS group and subgroup |
MBS item number |
|---|---|---|
|
Palliative medicine attendances |
|
|
|
Attendance in a consulting room or hospital, initial brief video conference |
Group A24 |
3003* |
|
Attendance in a consulting room or hospital, initial visit |
Group A24 |
3005 |
|
Attendance in a consulting room or hospital, subsequent visit, minor, after initial attendance |
Group A24 |
3014 |
|
Attendance in a consulting room or hospital, subsequent visit, other than a minor attendance |
Group A24 |
3010 |
|
Attendance in a consulting room or hospital, video conference |
Group A24 |
3015* |
|
Attendance in a place other than consulting rooms or hospital, initial visit |
Group A24 |
3018 |
|
Attendance in a place other than consulting rooms or hospital, subsequent visit |
Group A24 |
|
|
Attendance in a place other than consulting rooms or hospital, subsequent visit, minor, after initial attendance |
Group A24 |
3028 |
|
Palliative medicine case conferences |
|
|
|
Organise and coordinate a community case conference 15–<30 minutes |
Group A24 |
3032 |
|
Organise and coordinate a community case conference 30–<45 minutes |
Group A24 |
3040 |
|
Organise and coordinate a community case conference >=45 minutes |
Group A24 |
3044 |
|
Participate in a community case conference 15–<30 minutes |
Group A24 |
3051 |
|
Participate in a community case conference 30–<45 minutes |
Group A24 |
3055 |
|
Participate in a community case conference >=45 minutes |
Group A24 |
3062 |
|
Organise and coordinate a discharge case conference 15–<30 minutes |
Group A24 |
3069 |
|
Organise and coordinate a discharge case conference 30–<45 minutes |
Group A24 |
3074 |
|
Organise and coordinate a discharge case conference >=45 minutes |
Group A24 |
3078 |
|
Participate in a discharge case conference 15–<30 minutes |
Group A24 |
3083 |
|
Participate in a discharge case conference 30–<45 minutes |
Group A24 |
3088 |
|
Participate in a discharge case conference >=45 minutes |
Group A24 |
3093 |
* Items 3003 and 3015 ceased on 31 December 2021, with telehealth services now claimed against relevant item numbers in Group A40.
Note: Refer to the Medicare Benefits Schedule Book (MBS) July 2022 edition for full item descriptions (pages 309–313) and further information relating to MBS Palliative care (pages 109–110).
The MBS data presented in this report relate to services provided on a ‘fee-for-service’ basis for which MBS benefits were paid. Excluded are details of relevant services to public in-patients or public outpatients of hospitals and services funded from the Department of Veterans’ Affairs National Treatment Account.
In this release, year was determined from the date the service was provided, rather than the date the service was processed by Services Australia. Note that in releases prior to 2022, data were on a financial year of processing basis, while in this report data (2021–22 and trend data) were on a financial year of service basis capturing claims processed up to and including 31 December 2022.
The state or territory was determined according to the postcode of the person’s Medicare enrolment address on the last date of service record for the items in question, within the reference period. In some cases, this will not be the same as the postcode of the person’s residential address. Age and sex were determined from the last date of service within the reference period and attributed to all service claims reported for that individual.
During the COVID-19 pandemic, the Australian Government expanded MBS-subsidised telehealth service to allow Australians to access health services from their home or place of care, to help limit the potential exposure of patients and health practitioners to the virus. This included 6 new temporary MBS items (91824, 91825, 91826, 91834, 91835 and 91836) which could be used by pain and palliative medicine physicians/specialists to provide telehealth services, either by videoconference or by telephone, as a substitution for existing face to face MBS consultation services (DHAC 2022). Data on these telehealth services and other relevant telehealth items provided by specialists and consultant physicians in palliative medicine were included in this report to provide insights on how palliative care medicine attendance and case conference services provided by palliative care physicians/specialists changed in response to the COVID-19 pandemic.
References
DHAC (Department of Health and Aged Care) (2022) Medicare Benefits Schedule Book, Operating from 1 July 2022, Canberra: Department of Health and Aged Care, Australian Government, accessed 30 January 2023.
|
Key concept |
Description |
|---|---|
|
Attendance at person’s place of residence |
A professional attendance in the patient’s home, residential aged care facility (other than consulting rooms within a residential aged care facility), or other institution by a specialist, or consultant physician, in the speciality of palliative medicine following referral by a referring practitioner. |
|
Palliative medicine |
Palliative medicine is defined as the specialist care of people with terminal illnesses and chronic health conditions in community, hospital and hospice settings. Palliative medicine physicians work collaboratively with a multidisciplinary team of health professionals to provide end-of-life care, provide relief from pain and symptoms of illness, and optimise the quality of life for a patient. Palliative medicine treats the physical aspects of illness, but also integrates psychological and spiritual facets of patient care (RACP 2020). |
|
Palliative medicine physician/specialist |
Medical practitioner who, in order to be eligible for payment of MBS subsidies for palliative care services, must be a Fellow of the Royal Australasian College of Physicians who has completed the College training program in palliative medicine, or a Fellow of the Australasian Chapter of Palliative Medicine, or a Fellow of both. |
|
Specialist attendances |
A specialist attendance usually requires a referral from a general practitioner. A specialist attendance is a referred patient-doctor encounter (with Medicare funding benefits), such as a visit, consultation, and attendance (including a telehealth) with a medical practitioner who has been recognised as a specialist or consultant physician for the purposes of Medicare benefits. |
|
Telehealth |
Health services delivered using information and communication technologies, such as videoconferencing or through other communication technologies. |
References
RACP (Royal Australian College of Physicians) (2020) Australasian Chapter of Palliative Medicine, Sydney: RACP, accessed 10 February 2023.


