Use of health services
On this page:
Key points
- While the primary source of health services for serving personnel is Defence funded health services, nearly 1 in 4 of those who died by suicide (23%) used a Medicare-subsidised or DVA-funded health service in the year prior to death.
- From 2001 to 2018, the majority of ex-serving males (88%) and reserve males (85%) who died by suicide used at least one Medicare-subsidised or DVA‑funded health service in the year before death.
- Over half (53%) of ex-serving males who died by suicide in 2014 to 2018 had a mental health‑related service (subsidised by Medicare, DVA or Defence) in the year before death, compared with the Australian male population who died by suicide (38%).
- Among ex-serving DVA clients who received hospital-based (secondary) care between 2001 and 2018, 25% received care for mental and behavioural disorders.
- Between 2001 and 2018, 20% of the DVA clients who died by suicide received admitted patient care
- From 2015 to 2018, 6% of ex-serving DVA clients presented to emergency departments, most commonly for injury, poisoning and other consequences of external causes (31%).
ADF members are able to access a variety of different health services, engaging with different systems over their lifetime. This chapter examines access to health services by the study cohort: ADF members who have died by suicide with at least 1 day of service since 1 January 2001.
The analysis covers:
- Medicare claims data and DVA-funded services for the period 2001 to 2018 for the ex-serving population.
- Medicare claims data and DVA-funded services for the period 2000 to 2018 for those who died by suicide between 2001 and 2018 to understand patterns of use 1 year prior to death.
- Defence Health Service Contracts (HSC) off-base data from 2013 to 2018 which provides information on health services used by ADF members who died by suicide between 2014 and 2018 to understand patterns of use 1 year prior to death.
- Information on other Defence funded health services include Health Hotline is presented for the period 2012 to 2018.
Broadly, serving personnel primarily access Defence funded health services although they may access Medicare-subsidised and DVA-funded health services. Ex-serving and reserve ADF members can access both Medicare-subsidised and DVA funded health services for approved claims (Table 15).
All current and ex-serving ADF members may also access public hospitals, emergency departments and specialised non-admitted services (not funded by DVA), ancillary private health services (‘extras’), or pay for services entirely out-of-pocket. Data on these health services are not available for this report.
| Serving | Reserve | Ex-serving |
|---|---|---|
|
Defence-funded health services Serving and reserve ADF members can access health services through Health Service Contracts (HSC) off-base (data available for 2013 – 2018), Health Hotline (data available for 2012 – 2018) and Defence Electronic Health Systems (data not presented in this report). |
|
|
|
|
DVA-funded health services Data available for 2000 – 2018 (Emergency data for 2015 – 2018) DVA clients can access general practitioner (GP), specialist, allied health, hospital and emergency department services. |
|
|
Medicare-subsidised health services Data available for 2000 – 2018 Australia’s universal health insurance scheme, Medicare, subsidises access to a range of treatments and diagnostic tests for Australians (and some overseas visitors). These services include general GP and medical specialist services, hospital treatments for private patients, selected diagnostic imaging and pathology services, and some allied health services. |
||
Health services accessed by veterans who died by suicide
Between 2001 and 2018, the proportion of ex-serving (88%) and reserve males (85%) who used Medicare-subsidised or DVA-funded health services in the year before death was similar to Australian males who died by suicide (85%). A similar proportion of ex-serving females used a Medicare-subsidised or DVA‑funded health service in the year before death (96%), compared with Australian females who died by suicide (94%). While the primary source of health services for serving ADF members is Defence funded health services, nearly 1 in 4 of those who died by suicide (23%) used a Medicare-subsidised or DVA-funded health service in the year prior to death.
Between 2014 and 2018, 198 ADF members died by suicide. Of these, 57 (29%) had a Medicare-subsidised, DVA-funded or Defence-funded Health Service Contracts (HSC) off-base health service provided in the week before death, and 109 (55%) had a service in the 30 days before death. Most serving members (97%) used at least one health service in the year before death, particularly in the 60 days before death with 84% having used a health service compared with 62% of ex-serving and 57% of reserve members (Figure 14).
Figure 14: Percentage of ADF members(a) and Australians(b) who died by suicide who used a Medicare-subsidised(c), DVA-funded or Defence-funded HSC off-base health service(d), by time before death(e), sex and service status, 2014 to 2018

Notes:
- The ADF cohort includes members who served at least one day from 1 January 2001 to 31 December 2018, and died by suicide between 1 January 2014 and 31 December 2018.
- The Australian cohort are people who died by suicide between 1 January 2014 and 31 December 2018, excluding deaths by suicides by ADF members. The cohorts are restricted to the age range of ex-serving male and female study populations.
- Use of health services for the Australian cohort is based on Medicare-subsidised services.
- Use of Defence HSC off-base services may be slightly underestimated for members who died by suicide in 2014 due to data quality issues for 2013 data.
- The time before suicide is inclusive of the person’s death date, and excludes services that occurred after their date of death. Services that occurred before a person was hired or terminated are included (provided they occurred within the time period being examined).
Source: AIHW analysis of PMKeyS-NDI-MBS-DVA-HSC off-base, 2014-2018
Mental health-related services
Over half (53%) of ex-serving males who died by suicide between 2014 and 2018 had a mental health-related service in the year before death. In comparison, over a third (38%) of Australian males who died by suicide in the same period received a Medicare‑subsidised mental health-related service in the year before death (Figure 15). Among serving and reserve male and female ADF members who died by suicide, around 2 in 5 (40%) had a mental health-related service in the year before death.
Of those ADF members who died by suicide between 2014 and 2018, 21% of ex‑serving males and 47% of ex-serving females used a mental health-related service in the 30 days before death compared with 15% of Australian males and 26% of Australian females, respectively.
Figure 15: Percentage of ADF members(a) and Australians(b) who died by suicide and used a Medicare-subsidised(c), DVA-funded or Defence-funded HSC off-base(d) mental health-related service before death, by time before death(e), sex and service status, 2014 to 2018

n.p. – not published due to small numbers.
Notes
- The ADF cohort includes members who served at least one day from 1 January 2001 to 31 December 2018, and died by suicide between 1 January 2014 and 31 December 2018. Results are not reported for reserve and serving females due to small numbers.
- The Australian cohort are people who died by suicide between 1 January 2014 and 31 December 2018, excluding deaths by suicides by ADF members. The cohorts are restricted to the age range of ex-serving male and female study populations.
- Use of health services for the Australian cohort is based on Medicare-subsidised services.
- Use of Defence HSC off-base services may be slightly underestimated for members who died by suicide in 2014 due to data quality issues for 2013 data.
- The time before suicide is inclusive of the person’s death date, and excludes services that occurred after their date of death. Services that occurred before a person was hired or terminated are included (provided they occurred within the time period being examined).
Sources: AIHW analysis of linked PMKeyS–NDI–MBS–DVA–HSC off-base data 2014–2018.
Medicare-subsidised and DVA-funded health services
This section looks at use of Medicare-subsidised and DVA-funded health services by those ex-serving ADF members who accessed services at least once a year in the period from 2001 to 2018.
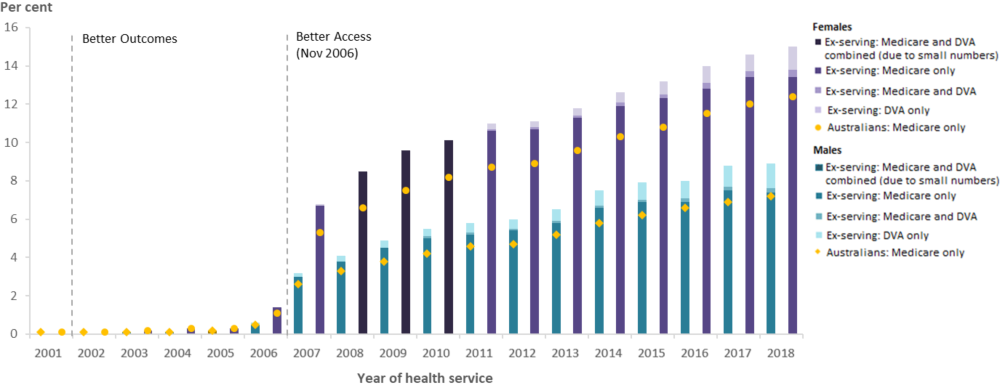
Overall, the proportion of ex-serving ADF members who used Medicare-subsidised and DVA-funded health services increased from 59% in 2001 to 84% in 2018 for males, and 77% to 92% for females. From 2001 to 2018, a lower proportion of ex-serving males (from 59% to 84%) and ex-serving females (from 77% to 92%) used Medicare-subsidised services and DVA‑funded services compared with the Australian male (from 83% to 87%) and female population (from 94% to 95%) (Figure 16 and Figure 17). While the Australian male and female population groups are restricted to the age range of the male and female ex-serving study group respectively, there are differences in the age structure within these ranges that may account for differences in service use.
Of ex-serving members who used health services, almost all accessed a Medicare‑subsidised service at least once in the year, especially females (around 99%). The proportion of ex‑serving ADF members who used at least one DVA-funded health service increased steadily between 2001 and 2018, ranging from 7% to 20% for males, and 2% to 15% for females (Figure 16 and Figure 17).
Figure 16: Percentage of ex-serving female ADF members(a) who used at least one Medicare-subsidised or DVA-funded health service, and Australians(b) who used a Medicare-subsidised service, by sex and year, 2001 to 2018
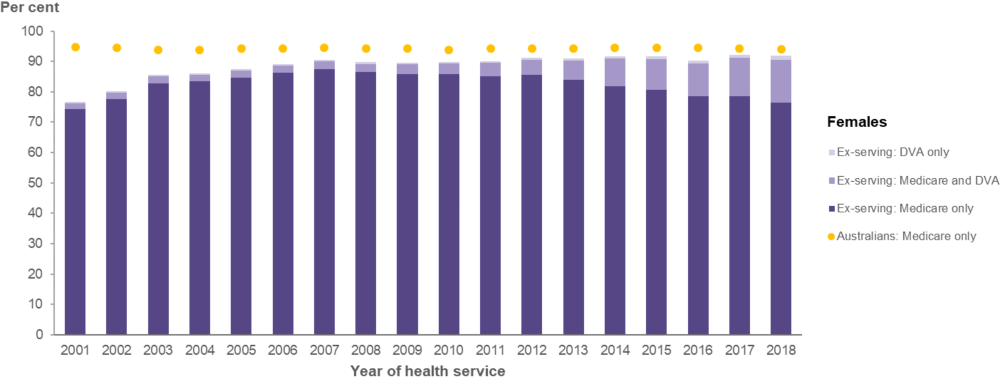
Notes
- The ex-serving cohort are females who served at least one day from 1 January 2001 to 31 December 2018. Medicare and DVA services provided to ex-serving members before they were terminated were excluded from the analysis (i.e. while they were serving or before they were hired). The denominator is the total number of ex-serving female members who were ex-serving for at least one day in the reporting year. Note, in 2016, approximately 6,600 reservists separated from the ADF, resulting in a marked increase of ex-serving members.
- The Australian cohort is restricted to the age range of ex-serving female study group, noting that there are differences in the age structure within these ranges that may account for differences in service use.
Source: AIHW analysis of PMKeyS-NDI-MBS, 2001-2018; Department of Health MBS claims data, 2001-2018; Australian Bureau of Statistics (ABS) Estimated Resident Population (ERP) 2001-2018.
Figure 17: Percentage of ex-serving male ADF members(a) who used a Medicare-subsidised or DVA-funded health service, and Australians(b) who used a Medicare-subsidised service, by sex and year, 2001 to 2018
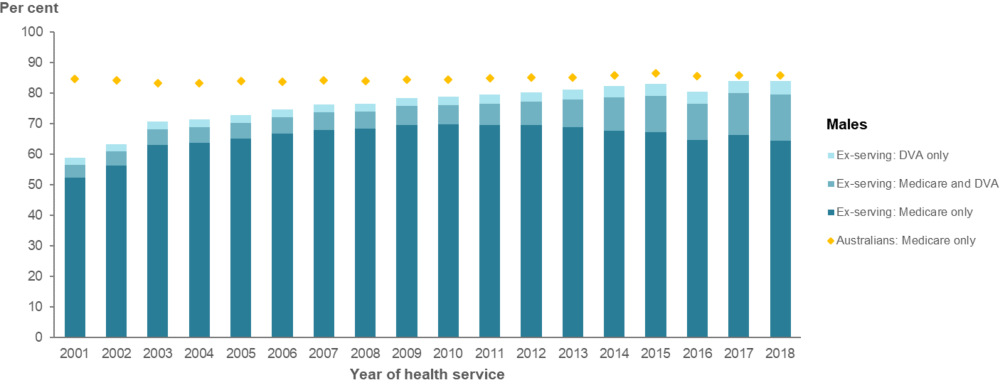
Notes
- The ex-serving cohort are males who served at least one day from 1 January 2001 to 31 December 2018. Medicare and DVA services provided to ex-serving members before they were terminated were excluded from the analysis (i.e. while they were serving or before they were hired). The denominator is the total number of ex-serving male members who were ex-serving for at least one day in the reporting year. Note, in 2016, approximately 6,600 reservists separated from the ADF, resulting in a marked increase of ex-serving members.
- The Australian cohort is restricted to the age range of ex-serving male study group, noting that there are differences in the age structure within these ranges that may account for differences in service use.
Source: AIHW analysis of PMKeyS-NDI-MBS, 2001-2018; Department of Health MBS claims data, 2001-2018; ABS ERP 2001-2018.
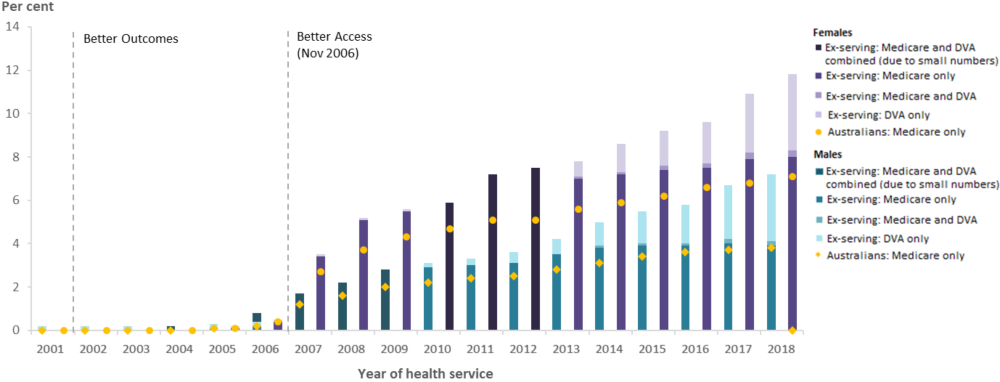
Mental health-related Medicare and DVA services
Mental health‑related services subsidised through Medicare and DVA may be provided by psychiatrists, general practitioners (GPs), psychologists and other allied health professionals.
The proportion of all ex-serving members who used a Medicare-subsidised or DVA-funded mental health-related service increased steadily between 2001 and 2018 for both males (3% to 16%) and females (3% to 22%) (Figure 18). This pattern is broadly reflective of the increase in use of Medicare-subsidised services by the Australian population, which can be largely attributed to the introduction of the Better Access program for all Australians (Box 1).
In recent years, the use of Medicare-subsidised mental health-related service were similar between ex-serving ADF members (9% for males and 17% for females in 2018) and the Australian population (9% for males and 15% for females in 2018). However, the higher overall use by ex-serving members was largely attributable to additional members who used DVA-funded services, adding 6.5 percentage points for ex-serving males and 5.2 percentage points for ex-serving females in 2018.
Figure 18: Percentage of ex-serving ADF members(a) who used a Medicare-subsidised or DVA-funded(b) mental health-related service; and Australians(c) who used a Medicare-subsidised mental health-related service, by sex and year, 2001 to 2018
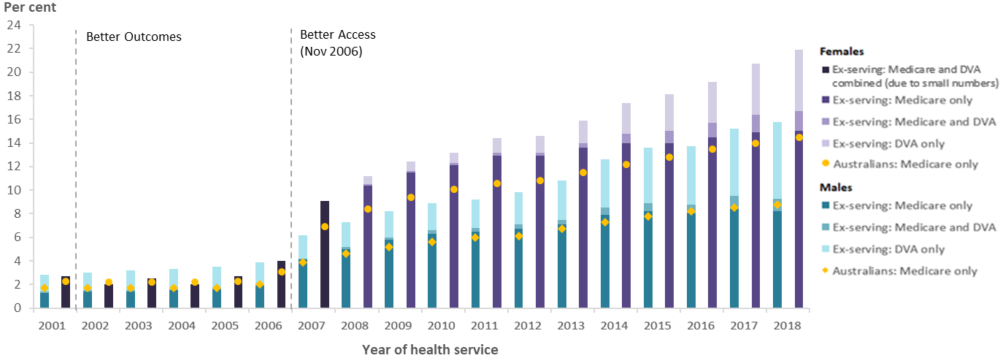
Notes
- The ex-serving cohort are those who served at least one day from 1 January 2001 to 31 December 2018. Medicare and DVA services provided to ex-serving members before they were terminated were excluded from the analysis (i.e. while they were serving or before they were hired). The denominator is the total number of ex-serving members who were ex-serving for at least one day in the reporting year.
- Interpret with caution. Similar services may be provided outside Medicare and DVA, or under different 'general' Medicare items - neither of which can be identified in the data. The proportion of mental health-related services claimed outside Medicare and DVA is unknown, and is likely to have substantially changed across the 2001 to 2018 reporting period, affecting comparability over time.
- The Australian cohort is restricted to the age range of ex-serving male and female study populations.
Source: AIHW analysis of PMKeyS-NDI-MBS, 2001-2018; Department of Health MBS claims data, 2001-2018; ABS ERP 2001-2018.
Box 1: Changes to mental health-related services subsidised by Medicare and DVA
The services that Medicare subsidises, and how similar services are coded has changed over time, particularly for mental health services provided by GPs and allied health professionals. A significant change occurred in November 2006 with the introduction of the Better Access program. As a result, key findings for mental health-related service use are mainly reported for the periods 2007 to 2018 and from 2008 to 2018 for services used 1 year prior to death.
DVA-funded healthcare includes identical Medicare items, however during this period, DVA clients were entitled to ‘uncapped’ services. DVA has also increased access to mental health services through various policy changes since 2001, most significantly in 2016 when eligibility was expanded to include all current and former ADF members with at least one day of continuous full-time service.
See Appendix A5 for information about these initatives and details about how mental health-related Medicare subsidised and DVA-funded services are grouped.
The proportion of ex-serving members using psychiatry services (Medicare or DVA) has almost doubled from 3.9% in 2011 to 7.4% in 2018 for males and 3.5% to 7.1% for females. This is mainly an increase in the number of ex-serving members who used DVA‑funded psychiatry services. Most mental health care received by ex-serving members eligible for DVA-funded services was provided by psychiatrists. In 2018, 80% of all ex-serving males and 69% of females had their psychiatry services funded by DVA (Figure 19).
Figure 19: Percentage of ex-serving ADF members(a) who used a Medicare-subsidised or DVA-funded psychiatry service; and Australians(b) who used a Medicare-subsidised psychiatry service, by sex and year, 2001 to 2018
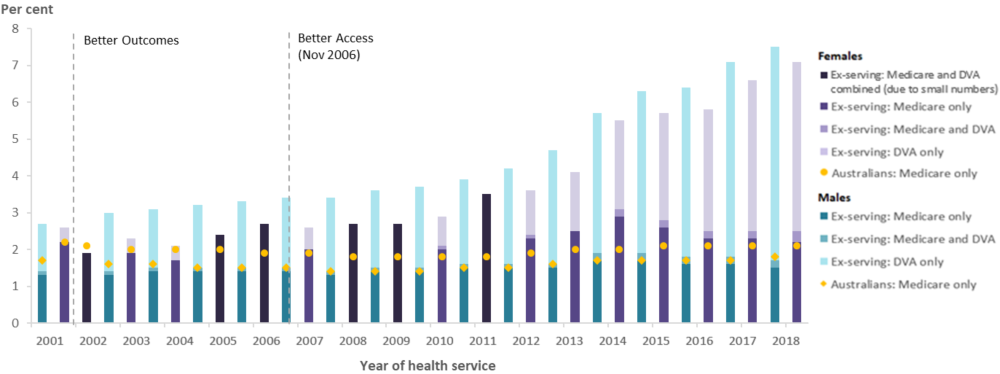
Notes
- The ex-serving cohort are those who served at least one day from 1 January 2001 to 31 December 2018. Medicare and DVA services provided to ex-serving members before they were terminated were excluded from the analysis (i.e. while they were serving or before they were hired). The denominator is the total number of ex-serving members who were ex-serving for at least one day in the reporting year.
- The Australian cohort is restricted to the age range of ex-serving male and female study populations.
Source: AIHW analysis of PMKeyS-NDI-MBS, 2001-2018; Department of Health MBS claims data, 2001-2018; ABS ERP 2001-2018.
The use of mental health related GP services and mental health related allied health services has steadily increased since 2006 for male and female ex-serving members and the general Australian population. The majority of ex-serving patients who used GP and allied mental health services claimed their services through Medicare (Figure 20 and Figure 21).
Figure 20: Percentage of ex-serving ADF members(a) who used a Medicare-subsidised or DVA-funded mental health-related GP service(b); and Australians(c) who used a Medicare-subsidised mental health-related GP service, by sex and year, 2001 to 2018
Notes
- The ex-serving cohort are those who served at least one day from 1 January 2001 to 31 December 2018. Medicare and DVA services provided to ex-serving members before they were terminated were excluded from the analysis (i.e. while they were serving or before they were hired). The denominator is the total number of ex-serving members who were ex-serving for at least one day in the reporting year.
- Interpret with caution. Similar GP mental health services may be provided under different 'general' Medicare items. The proportion of these services is unknown, and is likely to have substantially changed across the 2001 to 2018 reporting period, affecting comparability over time.
- The Australian cohort is restricted to the age range of ex-serving male and female study populations.
Source: AIHW analysis of PMKeyS-NDI-MBS, 2001-2018; Department of Health MBS claims data, 2001-2018; ABS ERP 2001-2018.
Figure 21: Percentage of ex-serving ADF members(a) who used a Medicare-subsidised or DVA-funded(b) mental health-related allied health service(c); and Australians(d) who used a Medicare-subsidised service, by mental health-related allied health service, by sex and year, 2001 to 2018
Notes
- The ex-serving cohort are those who served at least one day from 1 January 2001 to 31 December 2018. Medicare and DVA services provided to ex-serving members before they were terminated were excluded from the analysis (i.e. while they were serving or before they were hired). The denominator is the total number of ex-serving members who were ex-serving for at least one day in the reporting year.
- Interpret with caution. Similar services may be provided outside Medicare and DVA. The proportion of mental health-related services claimed outside Medicare and DVA is unknown, and is likely to have substantially changed across the 2001 to 2018 reporting period, affecting comparability over time.
- 'Allied Mental Health' includes services provided by clinical psychologists, other psychologists, and other allied mental health workers.
- The Australian cohort is restricted to the age range of ex-serving male and female study populations.
Source: AIHW analysis of PMKeyS-NDI-MBS, 2001-2018; and Department of Health MBS claims data, 2001-2018.
A higher proportion of ex-serving members who separated for involuntary medical reasons used Medicare-subsidised and DVA-funded mental health related services and in particular psychiatry services, compared to those who separated for other involuntary reasons or voluntarily (Figure 22).
Figure 22: Percentage of ex-serving ADF members(a) who used a Medicare-subsidised or DVA-funded mental health-related service(b), by separation reason and sex, 2018
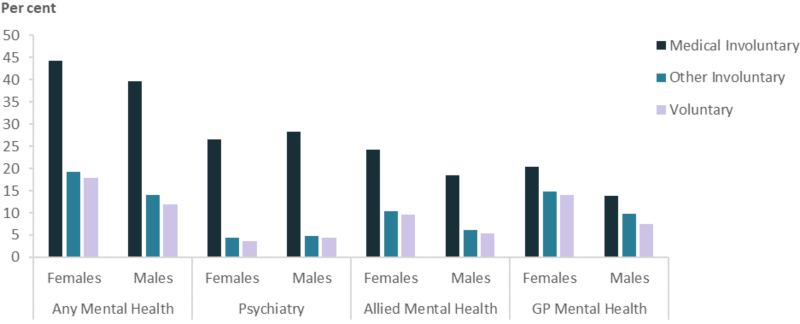
Notes
- The ex-serving cohort are those who served at least one day from 1 January 2001 to 31 December 2018, and who were ex-serving for at least one day in 2018. Medicare and DVA services provided to ex-serving members before they were terminated were excluded from the analysis (i.e. while they were serving or before they were hired).
- 'Allied Mental Health' includes services provided by clinical psychologists, other psychologists, and other allied mental health workers.
Sources: AIHW analysis of linked PMKeyS–NDI–MBS–DVA data 2018.
Use of hospital-based services funded by DVA
This section examines admitted patient and emergency department services used by ADF members (serving, reserve and ex-serving) eligible for healthcare funding by DVA (‘DVA clients’ The analysis uses administrative data from the DVA National Treatment Account, which has limited analysis to DVA clients. Future analysis could investigate the use of Australian hospital-based services by all ADF members, including those who died by suicide, and Australians who died by suicide.
ADF members are eligible for the provision of DVA-funded healthcare according to various criteria (DVA 2021). However, DVA clients can continue to access all public Medicare services and hospital-based care and may use these services, private health insurance-funded or self‑funded services independently of the DVA.
A total of 11,140 (26%) ex-serving DVA clients received overnight or day-only admitted patient care from 2001 to 2018. Most were males (90%). The care provided to these DVA clients included acute care1 (85%), rehabilitation care2 (4%) and mental health care3 (1%) (mental health care was included with acute care until 1 July 2015).
In terms of the number of patients, the most frequent reasons (principal diagnoses) for DVA clients to receive admitted patient care were diseases of musculoskeletal and connective tissue (50%), mental and behavioural disorders (25%), diseases of the digestive system (24%) and neoplasms (20%) (Table 16).
Notes
- Acute care is where the primary treatment goal is to cure or treat symptoms of illness, perform surgical, therapeutic or diagnostic procedures or to manage labour (obstetric)
- Rehabilitation is care where the primary treatment is to improve functioning of a patient with impairment due to a health condition (excluding mental health)
- Mental health care is care where the primary treatment goal is to improve symptoms and/or psychosocial, environmental and physical functioning related to a mental health disorder
| Principal diagnosis (ICD 10AM Chapter) | No. (%(e)) patients | No. (%(f)) episodes | Average episodes/patient |
|---|---|---|---|
|
Diseases of musculoskeletal and connective tissue (M00-M99) |
5,509 (49.5) |
15,758 (16.3) |
2.9 |
|
Mental and behavioural disorders (F00-F99) |
2,830 (25.3) |
32,161 (33.2) |
11.4 |
|
Diseases of the digestive system (K00-K93) |
2,702 (24.3) |
5,398 (5.5) |
2.0 |
|
Neoplasms (C00-C96, D00-D09, D37-D48) |
2,219 (20.0) |
5,430 (5.6) |
2.4 |
|
Diseases of the nervous system (G00-G99) |
1,569 (14.1) |
3,049 (3.1) |
1.9 |
|
Injury, poisoning and certain other consequences of external causes (S00-T98) |
1,517 (13.6) |
2,740 (2.8) |
1.8 |
|
Diseases of the circulatory system (I00-I99) |
1,277 (11.5) |
2,622 (2.7) |
2.1 |
Notes
- Overnight or day-only care at an Australian hospital (>90% private).
- Principal diagnoses only, secondary diagnoses are not included.
- The DVA client numerator is all ex-serving ADF members (all ages, all sexes) who served at least 1 day from 1 January 2001 to 31 December 2018, and received admitted patient care funded by DVA by principal diagnosis. The denominator is all ex-serving ADF members who were DVA clients for at least one day in the reporting period, and received admitted patient care funded by DVA.
- DVA clients can appear in multiple principal diagnosis groups if they have received admitted patient care for different reasons on different occasions.
- Per cent of all DVA clients receiving admitted patient care 2001 to 2018.
- Per cent of all episodes of care provided to DVA clients 2001 to 2018.
Source: AIHW analysis of PMKeyS-NDI-DVA, 2001-2018
Between 2001 and 2018, the greatest number of all episodes of care4 (33%) were provided to ex‑serving DVA clients with a mental and behavioural disorder as their principal diagnosis. During this period, the average number of episodes of care for mental and behavioural disorders for ex-serving DVA clients was 11.4 per patient.
When including principal and all secondary diagnoses in the analysis, 3,326 (30%) ex‑serving DVA clients receiving admitted patient care had at least one diagnosis related to mental health; most had multiple mental health diagnoses. The most prevalent mental health diagnosis groups (ICD 10AM) for ex-serving DVA clients receiving admitted patient care are included in Table 17.
Note: 4. An episode of care can be a total hospital stay or a portion of a hospital stay when there is a change of care type e.g. from acute care to rehabilitation care.
|
Diagnosis group (ICD 10AM ) |
No. (%(e)) patients |
No. (%(f)) episodes |
Average episodes/patient |
|---|---|---|---|
|
Stress-related disorders (F43) |
2,422 (72.8) |
25,938 (75.9) |
10.7 |
|
Depressive disorders (excluding bipolar) (F32) |
1,816 (54.6) |
10,193 (29.8) |
5.6 |
|
Drug and alcohol disorders (F10-F19, Z502-3, Z714-5) |
1,610 (48.4) |
9,508 (27.8) |
5.9 |
|
Anxiety disorders (F40-2, F44-8) |
1,080 (32.5) |
3,691 (10.8) |
3.4 |
|
Bipolar and mixed-mood disorders (F30-1, F33-9) |
727 (21.9) |
2,931 (8.6) |
4.0 |
|
Dementia (F00-3, F051, G30) |
123 (4) |
188 (1.0) |
1.5 |
|
Schizophrenia and related disorders ((F20-9) |
110 (3) |
548 (1.7) |
5.0 |
Notes
- Principal and all secondary diagnoses are included.
- The DVA client numerator is all ex-serving ADF members (all ages, all sexes) who served at least 1 day from 1 January 2001 to 31 December 2018, and received admitted patient care funded by DVA for the diagnosis group. The denominator is all ex-serving ADF members who were DVA clients for at least one day in the reporting period, and received admitted patient care funded by DVA.
- DVA clients can appear in multiple diagnosis groups if they have received amitted patient care for multiple diagnoses or different diagnoses on different occasions.
- Overnight or day-only care at an Australian hospital (>90% private).
- Per cent of all DVA clients receiving admitted patient care for mental health 2001-2018.
- Per cent of all episodes of care which included at least 1 mental health-related principal or secondary diagnosis 2001-2018.
Source: AIHW analysis of PMKeyS-NDI-DVA, 2001-2018
The most common mental health diagnostic groups among ex-serving DVA clients receiving admitted patient care were:
- Stress related disorders (73%)
- Depressive disorders (excluding bipolar and mixed mood disorders) (55%)
- Drug and alcohol disorders (48%).
While the proportion of all ex-serving DVA clients receiving admitted patient care for mental health disorders is between 0.5 – 3.3%, there has been a steady increase particularly since 2010 (Figure 23).
Figure 23: Percentage of ex-serving DVA clients(a)(b) who received admitted patient care(c)(d) for mental health disorders(e), 2001 to 2018
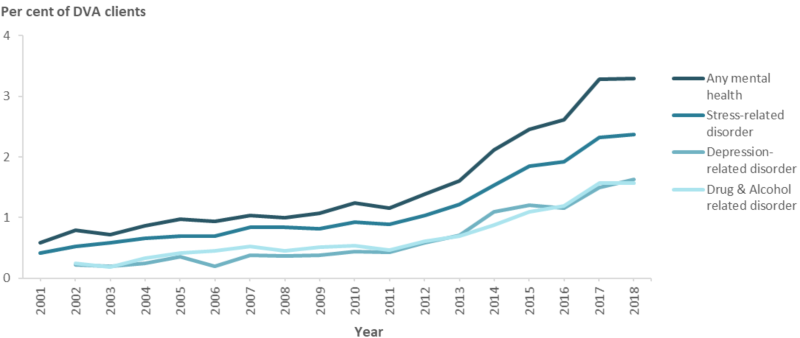
Notes
- The DVA client numerator is all ex-serving ADF members (all ages, all sexes) who served at least 1 day from 1 January 2001 to 31 December 2018, and received admitted patient care funded by DVA for at least 1 mental health diagnosis. The denominator is all ex-serving members who were DVA clients for at least one day in the reporting period
- DVA clients can appear in multiple diagnosis groups if they have received admitted patient care for multiple reasons or for different reasons on different occasions.
- Principal and all secondary diagnoses are included.
- Overnight or day-only care at an Australian hospital (>90% private).
- 2001 results for the ‘Depression-related disorder’ and ‘Drug & Alcohol related disorder’ are suppressed due to small numbers.
Source: AIHW analysis of PMKeyS-NDI-DVA, 2001-2018.
A total of 2,543 (6%) ex-serving DVA clients presented to a public emergency department (ED) between 2015 and 2018; 93% were men. During this period, the mean number of ED presentations by a DVA client was two.
The most common reasons for presentation (principal diagnosis) were injury, poisoning and other consequences of external causes (31%) followed by diseases of the circulatory system (10%), diseases of musculoskeletal and connective tissue (9%) and mental and behavioural disorders (9%).
- 31 (20%) of the DVA clients who died by suicide received admitted patient care on 261 occasions between 2001 and 2018; 24 DVA clients received care within 12 months of death.
- All female and most male (74%) DVA clients had at least one mental health-related diagnosis recorded for their hospital admission.
- 9 DVA clients presented to a public ED between 2015 and 2018.
Defence Health Hotline
The 1800 IMSICK service is a national, 24 hour, nurse triage and health support line for use by ADF Entitled Personnel if they become ill or injured after hours or are not in close proximity to a Defence health facility.
Between 2012 and 2018, Defence Health Hotline received 68,053 calls from 31,826 ADF members. Half of the callers made more than one call; thirty-five calls were received from 16 ADF members who died by suicide. During the period, the hotline received 503 mental health‑related calls from 444 ADF members, including from a small number of those who died by suicide. These calls include:
- 58 calls from 53 ADF members about suicide or homicidal behaviour
- 36 calls from 35 ADF members about suicide ideation
- 5 calls from 5 ADF members about self-harm behaviour.


