A high-quality and safe health system increases the likelihood of desired health outcomes, reduces costs to patients and the health system, and keeps patients protected from preventable harm.
These pages present the latest available performance information on safety and quality in Australian hospitals, based on the measures that can be derived from the national hospitals data collections.
Safety and quality bookmark 1
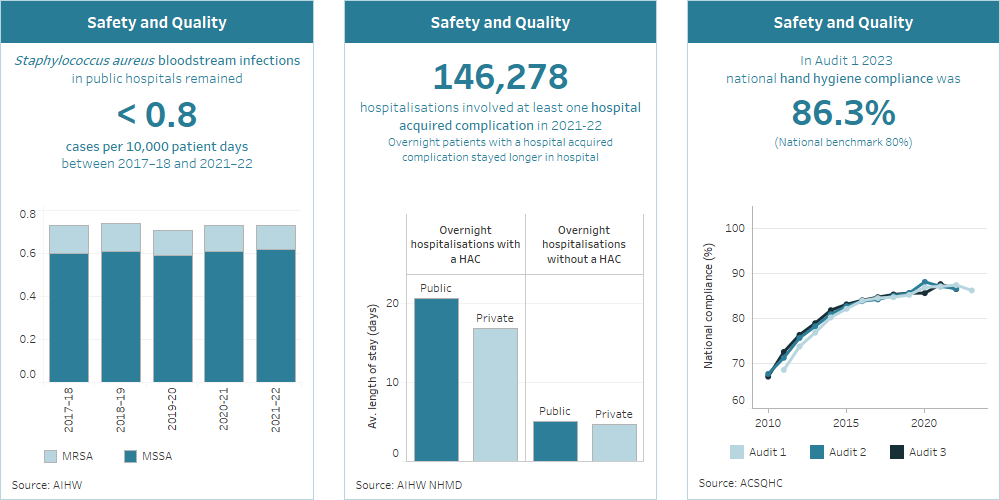
Staphylococcus aureus bloodstream infections in public hospitals have remained less than 0.8 cases per 10,000 patient days between 2018–19 and 2022–23.
Safety and quality bookmark 2
149,700 hospitalisations involved at least one hospital acquired complication in 2022–23. Patients with a hospital acquired complication stayed longer in hospital.
Safety and quality bookmark 3
In Audit 1 2023, national compliance was 86.3% (national benchmark 80%).
How is the safety and quality of care in hospitals measured?
The safety and quality of care provided to patients in hospitals can be measured in several ways. Measures reported on these pages are:
- healthcare-associated infections (Staphylococcus aureus bloodstream infections)
- hand hygiene compliance
- hospital-acquired complications
- conditions that arose during a hospital stay
- potentially preventable hospitalisations
- patients’ experiences of hospital care.
Below is a summary of the latest results for each of these safety and quality measures. Detailed information and further results, including trends over time, are presented at Admitted patient safety and quality.
Healthcare-associated infections: Staphylococcus aureus bloodstream infections (SABSI)
Healthcare-associated infections are one of the most common complications affecting patients in hospital and can prolong a patient’s hospital stay or result in death. Infections, such as Staphylococcus aureus (also known as ‘golden staph’), can be acquired as a direct or indirect result of care received in hospital. The current agreed benchmark for SABSI is no more than 1 case per 10,000 days of patient care.
In 2022–23:
- there were 1,668 cases of SABSI occurring during 22.5 million days of patient care in public hospitals – this was a rate of 0.74 SABSI cases per 10,000 patient days
- for public hospitals, all states and territories except Tasmania had rates of infection that were below the national benchmark of 1 case per 10,000 patient days
- for private hospitals that volunteered to report SABSI surveillance data to the national collection (23% of hospitals), there were 207 SABSI cases occurring during just under 5.7 million days of patient care – a rate of 0.35 cases per 10,000 patient days.
Hand hygiene compliance
Hand hygiene refers to the washing of hands or use of alcohol-based rubs. Good hand hygiene is a first-line defence against viruses and infections.
Hand hygiene compliance by healthcare workers at specific times (or ’moments’) before and after patient interactions and procedures are audited year-round and reported against the current national benchmark of 80%.
In audit period 1, 2023 (1st November 2022 to 31 March 2023):
- the national hand hygiene compliance rate was 86%
- compliance rates for each of the 5 moments varied between 81% (moment 5 – after touching a patient's surroundings) and 93% (moment 3 – after a procedure or body fluid exposure risk)
- the highest compliance rates were among dental professionals and nurses and midwives.
Hospital-acquired complications
The Australian Commission on Safety and Quality in Health Care (ACSQHC) lists 16 hospital-acquired complications (HACs) for which clinical risk mitigation strategies may reduce the risk of occurrence.
In 2022–23:
- one or more HACs were recorded in 115,000 hospitalisations in public hospitals (2.0% of hospitalisations), and 34,200 hospitalisations in private hospitals (0.8% of hospitalisations)
- the most recorded type of complication was Healthcare associated infection (37%), followed by Delirium (13%) and Cardiac complications (12%).
Conditions that arose during a hospital stay
Conditions that arise during a hospital stay include conditions which may or may not have been preventable.
In 2022–23, 988,000 hospitalisations (8.1% of hospitalisations) recorded a condition noted as arising during the episode of hospital care. Hospitalisations involving Childbirth were most likely to record a condition that arose during the hospital stay (51% of same-day hospitalisations and 70% of overnight hospitalisations).
Patients’ experience of hospital care
Patient experience captures information on patients’ views of their interactions with the healthcare system and communication with staff delivering healthcare services.
In 2022–23, among people aged 15 and over who used hospital services as an admitted patient, most reported that:
- hospital doctors and specialists spent enough time with them (73%), listened carefully (76%) and always showed respect (79%)
- hospital nurses spent enough time with them (74%), listened carefully (78%) and always showed respect (80%).
Potentially preventable hospitalisations
Potentially preventable hospitalisations are an indicator of the effectiveness of non-hospital care. These hospitalisations could have potentially been prevented through the provision of appropriate health interventions and early disease management in primary care and community-based care settings (including by general practitioners, medical specialists, dentists, nurses, and allied health professionals).
In 2022–23, there were 548,000 potentially preventable hospitalisations in public hospitals and 178,000 in private hospitals. These included:
- 273,000 hospitalisations for chronic conditions (excluding diabetes)
- 58,300 hospitalisations for diabetes complications
- 55,500 hospitalisations for vaccine-preventable conditions.



