Technical notes
On this page:
About the Australian Burden of Disease Study
The Australian Burden of Disease Study (ABDS) includes estimates of disease burden of more than 200 diseases and injuries in Australia. Burden of disease analysis is a way of measuring the impact of diseases and injuries on a population. It is the difference between a population’s actual health and its ideal health, where ideal health is living to old age in good health (without disease or disability).
Information and reports about burden of disease in Australia, including for Aboriginal and Torres Strait Islander (First Nations) people, are available on Burden of disease.
Avoidable fatal burden
Fatal burden is a measure of the years of life lost (YLL) due to dying prematurely (that is, before the expected life span), 1 YLL is 1 year of life lost. Fatal burden is based on 2 factors: the age at which a death occurs and the number of remaining years that a person would, on average, expect to live from that age. In the ABDS, the remaining life expectancy varies at each age but starts as a life expectancy at birth of 86.02 years. This ideal life span is based on the lowest observed death rates at each age group from multiple countries (Murray, Ezzati et al. 2012).
At a population level, the total fatal burden for a disease is the sum of the number of deaths from the disease at each age multiplied by the ideal remaining life expectancy for each person who died. For example, if for a certain cause:
- 2 people died at age 0
- 1 person died at age 15
- 3 people died at age 32
- 5 people died at age 70.
The total fatal burden for that cause would be the sum of:
- 2 deaths x 86.02 (ideal remaining life expectancy at age 0) = 172.04 YLL
- 1 death x 71.29 (ideal remaining life expectancy at age 15) = 71.29 YLL
- 3 deaths x 54.49 (ideal remaining life expectancy at age 32) = 163.47 YLL
- 5 deaths x 18.93 (ideal remaining life expectancy at age 70) = 94.65 YLL.
For a total population fatal burden of 501.45 YLL for this cause.
Diseases that usually cause deaths at younger ages (for example, birth trauma & asphyxia and cardiovascular defects) have a much higher average YLL per death than diseases that tend to cause deaths at older ages (for example, stroke and chronic kidney disease). Therefore, a similar amount of fatal burden can result from a small number of deaths occurring at young ages or a large number of deaths occurring at older ages.
Avoidable fatal burden is the fatal burden (YLL) due to potentially avoidable deaths among people aged under 75. Potentially avoidable deaths are deaths from conditions that are potentially preventable through individualised care and/or treatable through existing primary or hospital care. The under 75 age threshold for avoidable deaths is the general criteria that is used in avoidable mortality analyses.
Potentially avoidable deaths are classified using a nationally agreed definition (and ICD-10 codes) (AIHW 2022) (Table A1).
| Cause of death | ICD-10 Codes | Limits (age, sex) |
|---|---|---|
| Selected invasive infections(a) | A38–A41, A46, A48.1, G00, G03, J02.0, J13–J16, J18, L03 | |
| Viral pneumonia and influenza | J10–J12 | |
| HIV/AIDS | B20–B24 | |
| Colorectal cancer | C18–C21, C26.0 | |
| Skin cancer | C43, C44 | |
| Breast cancer | C50 | Female |
| Cervical cancer | C53 | |
| Prostate cancer | C61 | |
| Kidney cancer | C64 | |
| Thyroid cancer | C73 | |
| Hodgkin's disease | C81 | |
| Acute lymphoid leukaemia/ Acute lymphoblastic leukaemia | C91.0 | 0–44 years |
| Diabetes(a) | E10–E14 | |
| Rheumatic and other valvular heart disease | I00–I09, I33–I37 | |
| Hypertensive heart and renal disease(a) | I10–I13 | |
| Ischaemic heart disease | I20–I25 | |
| Cerebrovascular diseases | I60–I69 | |
| Heart failure(a) | I50, I51.1, I51.2, I51.4, I51.5 | |
| Pulmonary embolism | I26 | |
| Renal failure(a) | N17–N19 | |
| Chronic obstructive pulmonary disease (COPD) | J40–J44 | |
| Asthma | J45, J46 | |
| Peptic ulcer disease | K25–K27 | |
| Complications of the perinatal period | P00–P96 | |
| Complications of pregnancy, labour or the puerperium(a) | O00–O99 | |
| Falls | W00–W19 | |
| Fires, burns | X00–X09 | |
| Suicide and self-inflicted injuries | X60–X84, Y87.0 | |
| Misadventures to patients during surgical and medical care | Y60–Y69 | |
| Medical devices associated with adverse incidents in diagnostic and therapeutic use | Y70–Y82 | |
| Surgical and other medical procedures as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure | Y83, Y84 | |
| Transport accidents | V01–V99 | |
| Exposure to inanimate mechanical forces | W20–W49 | |
| Exposure to animate mechanical forces | W50–W64 | |
| Accidental drowning and submersion | W65–W74 | |
| Other accidental threats to breathing | W75–W84 | |
| Exposure to electric current, radiation and extreme ambient air temperature and pressure | W85–W99 | |
| Contact with heat and hot substances | X10–X19 | |
| Contact with venomous animals and plants | X20–X29 | |
| Exposure to forces of nature | X30–X39 | |
| Accidental poisoning by and exposure to noxious substances | X40–X49 | |
| Overexertion, travel and privation | X50–X57 | |
| Accidental exposure to other and unspecified factors(a) | X58, X59 | |
| Assault | X85–Y09 | |
| Event of undetermined intent(a) | Y10–Y34 | |
| Legal interventions and operations of war | Y35, Y36 | |
| Drugs, medicaments, and biological substances causing adverse effects in therapeutic use | Y40–Y59 | |
| Sequelae of external causes of morbidity and mortality(a) | Y85, Y86, Y87.1–Y89 |
(a) Some of the ICD-10 codes in this cause were assigned for redistribution in the ABDS2018, see the Australian Burden of Disease Study 2018: methods and supplementary material (AIHW 2021) for more information on redistribution.
Source: AIHW 2022
Mapping avoidable deaths to the ABDS
Of the 219 diseases and injuries defined for fatal burden analysis in the 2018 ABDS:
- 45 included only avoidable death ICD-10 codes
- 18 included both avoidable and non-avoidable death codes with no additional limitations (part-avoidable causes type 1)
- 2 contained only avoidable death codes with additional limitations (part-avoidable causes type 2)
- acute lymphoblastic leukaemia deaths were only classified as avoidable for ages 0–44
- breast cancer deaths were only classified as avoidable for females.
For reporting purposes in the 2018 ABDS, 2 of the 20 part-avoidable causes were combined, resulting in 19 part-avoidable causes used in the avoidable mortality analysis. Table A2 and Table A3 show the ABDS causes which included potentially avoidable ICD-10 codes, including notes about any limitations.
| ABDS cause code | ABDS cause name(s) | ICD-10 codes in ABDS cause |
|---|---|---|
| A01 | HIV/AIDS | B20–B24, O98.7 |
| A21 | Haemophilus influenzae type–b | G00.0 |
| A22 | Pneumococcal disease | G00.1, A40.3, J13 |
| A23 | Meningococcal disease | A39 |
| B01 | Pre-term birth and low birthweight complications | P01.0, P01.1, P05, P07, P22, P25–P28, P52, P61.2, P77 |
| B03 | Birth trauma and asphyxia | P01.7, P01.8, P01.9, P02, P03, P08, P10–P15, P20, P21, P24, P90, P91 |
| B05 | Neonatal infections | P23, P35.1–P35.9, P36, P37.1, P37.2, P37.5, P37.8, P37.9, P38, P39 |
| B07 | Other disorders of infancy | P00, P01.2–P01.6, P04, P29, P50, P51, P53–P60, P61.0–P61.1, P61.3–P61.9, P70–P72, P74–P76, P78–P81, P83, P92–P96 |
| C05 | Bowel cancer | C18–C20, C26.0 |
| C11 | Melanoma of the skin | C43 |
| C12 | Non–melanoma skin cancers | C44 |
| C14 | Cervical cancer | C53 |
| C17 | Prostate cancer | C61 |
| C20 | Kidney cancer | C64 |
| C22 | Thyroid cancer | C73 |
| C24 | Hodgkin Lymphoma | C81 |
| D01 | Coronary heart disease | I20–I25 |
| D02 | Stroke | I60–I69 |
| D03 | Rheumatic heart disease | I00–I02, I05–I06, I08.0–I08.1, I08.3, I09 |
| D05 | Hypertensive heart disease | I11 |
| E01 | Asthma | J45, J46 |
| E02 | Chronic obstructive pulmonary disease (COPD) | J40–J44 |
| I02(a) | Type 1 Diabetes | E10 (excluding E10.2), O240 |
| I03(a) | Type 2 Diabetes | E11 (excluding E11.2), O241 |
| I04(a) | Other Diabetes | E12–E13 (excluding E12.2 and E13.2), O242 |
| K01 | Maternal haemorrhage | O44.1, O45–O46, O67, O72 |
| K02 | Maternal infections | O41.1, O85–O86 |
| K03 | Hypertensive disorders of pregnancy | O10–O16 |
| K04 | Obstructed labour | O64–O66 |
| K05 | Early pregnancy loss | O00–O08 |
| K06 | Gestational diabetes | O24.4 |
| K98 | Other maternal conditions | O20–O23, O24.9, O25–O26, O28–O36, O40, O410, O41.8, O41.9, O42–O43, O44.0, O47–O48, O60–O63, O68–O71, O73–O75, O80–O84, O87–O92, O95–O97, O99 |
| Q01 | Road traffic injuries - motorcyclists | V20.3–V20.9, V21.3–V21.9, V22.3–V22.9, V23.3–V23.9, V24.3–V24.9, V25.3–V25.9, V26.3–V26.9, V27.3–V27.9, V28.3–V28.9, V29.4–V29.9 |
| Q02 | Road traffic injuries- motor vehicle occupants | V30.4–V30.9, V31.4–V31.9, V32.4–V32.9, V33.4–V33.9, V34.4–V34.9, V35.4–V35.9, V36.4–V36.9, V37.4–V37.9, V38.4–V38.9, V39.4–V39.9, V40.4–V40.9, V41.4–V41.9, V42.4–V42.9, V43.4–V43.9, V44.4–V44.9, V45.4–V45.9, V46.4–V46.9, V47.4–V47.9, V48.4–V48.9, V49.4–V49.9, V50.4–V50.9, V51.4–V51.9, V52.4–V52.9, V53.4–V53.9, V54.4–V54.9, V55.4–V55.9, V56.4–V56.9, V57.4–V57.9, V58.4–V58.9, V59.4–V59.9, V60.4–V60.9, V61.4–V61.9, V62.4–V62.9, V63.4–V63.9, V64.4–V64.9, V65.4–V65.9, V66.4–V66.9, V67.4–V67.9, V68.4–V68.9, V69.4–V69.9, V70.4–V70.9, V71.4–V71.9, V72.4–V72.9, V73.4–V73.9, V74.4–V74.9, V75.4–V75.9, V76.4–V76.9, V77.4–V77.9, V78.4–V78.9, V79.4–V79.9, V89.2, Y85.0 |
| Q04 | Other land transport injuries | V01.0, V02.0, V03.0, V04.0, V05.0, V06.0, V09.0, V09.1, V10.0–V10.2, V11.0–V11.2, V12.0–V12.2, V13.0–V13.2, V14.0– 14.2, V15.0–V15.2, V16.0–V16.2, V17.0–V17.2, V18.0–V18.2, V19.0–V19.3, V20.0–V20.2, V21.0–V21.2, V22.0–V22.2, V23.0–V23.2, V24.0–V24.2, V25.0–V25.2, V26.0–V26.2, V27.0–V27.2, V28.0–V28.2, V29.0–V29.3, V30.0–V30.3, V31.0–V31.3, V32.0–V32.3, V33.0–V33.3, V34.0–V34.3, V35.0–V35.3, V36.0–V36.3, V37.0–V37.3, V38.0–V38.3, V39.0–V39.3, V40.0–V40.3, V41.0–V41.3, V42.0–V42.3, V43.0–V43.3, V44.0–V44.3, V45.0–V45.3, V46.0–V46.3, V47.0–V47.3, V48.0–V48.3, V49.0–V49.3, V50.0–V50.3, V51.0–V51.3, V52.0–V52.3, V53.0–V53.3, V54.0–V54.3, V55.0–V55.3, V56.0–V56.3, V57.0–V57.3, V58.0–V58.3, V59.0–V59.3, V60.0–V60.3, V61.0–V61.3, V62.0–V62.3, V63.0–V63.3, V64.0–V64.3, V65.0–V65.3, V66.0–V66.3, V67.0–V67.3, V68.0–V68.3, V69.0–V69.3, V70.0–V70.3, V71.0–V71.3, V72.0–V72.3, V73.0–V73.3, V74.0–V74.3, V75.0–V75.3, V76.0–V76.3, V77.0–V77.3, V78.0–V78.3, V79.0–V79.3, V80–V88, V89.0, V89.1, V89.3, V89.9, Y85.9 |
| Q05 | Poisoning | X40–X49 |
| Q06 | Falls | W00–W19 |
| Q07 | Fire, burns and scalds | X00–X06, X08–X19 |
| Q08 | Drowning | V90, V92, W65–W70, W73–W74 |
| Q09 | Other unintentional injuries | V91, V93–V99, W20–W46, W49–W60, W64, W75–W81, W83–W94, W99, X20–X39, X50–X54, X57–X58, Y35–Y36, Y86, Y89.0, Y89.1 |
| Q10 | Suicide and self–inflicted injuries | X60–X84, Y87.0 |
| Q11 | Homicide and violence | X85–X99, Y00–Y09, Y87.1 |
| Q21 | Road traffic injuries – pedal cyclists | V10.3–V10.9, V11.3–V11.9. V12.3–V12.9, V13.3–V13.9, V14.3–V14.9, V15.3–V15.9, V16.3–V16.9, V17.3–V17.9, V18.3–V18.9, V19.4–V19.9, |
| Q22 | Road traffic injuries – pedestrians | V01.1, V01.9, V02.1, V02.9, V03.1, V03.9, V04.1, V04.9, V05.1, V05.9, V06.1, V06.9, V09.2, V09.3, V09.9, |
| Q99 | All other external causes of injury | Y40–Y66, Y69–Y84, Y88 |
(a) In the 2018 ABDS, deaths coded to ICD-10 code E14 (unspecified diabetes), excluding E14.2, were redistributed to either Type 1, Type 2 or Other diabetes (ABDS cause codes I02, I03 or I04).
| ABDS cause code | ABDS cause name(s) | ICD-10 codes in ABDS cause | Notes |
|---|---|---|---|
| A02 | Tuberculosis | A15–A19, B90, N33.0, N74.0, N74.1, O98.0, P37.0 | Only O98.0 and P37.0 classed as avoidable deaths |
| A03 | Syphilis | A50–A53, N29.0, N74.2, O98.1 | Only O98.1 classed as avoidable deaths |
| A05 | Gonorrhoea | A54, N74.3, O98.2 | Only O98.2 classed as avoidable deaths |
| A06 | Other sexually transmitted infections | A57–A60, A63–A64, O98.3 | Only O98.3 classed as avoidable deaths |
| A11 | Upper respiratory tract infections | J00–J06 | Only J02.0 classed as avoidable deaths |
| A19 | Rubella | B06, P35.0 | Only P35.0 classed as avoidable deaths |
| A24 | Other meningitis and encephalitis | A83–A87, B94.1, G00.2–G00.9, G01–G02, G03–G05 | Only G00.2–G00.9 and G03 classed as avoidable deaths |
| A28 | Malaria | B50–B54, P37.3–P37.4 | Only P37.3–P37.4 classed as avoidable deaths |
| A98(a) | Lower respiratory infections (including influenza and pneumonia) | J09–J12, J14–J18, J20–J22, J85, J86 | Only J10–J12, J14–J16 and J18 classed as avoidable deaths |
| A99 | Other infections | A20–A32, A38, A42–A44, A48.1, A48.2, A48.4–A49, A65–A70, A74–A80, A81.0, A81.2– A81.9, A82, A88–A89, A92.0– A92.7, A92.9, A93–A99, B00, B03–B04, B07, B08.0, B08.2–B08.3, B08.5–B08.8, B09, B17.2, B25, B27–B30, B33.0, B33.2–B33.8, B34–B49, B55–B85, B87–B89, B91–B92, B94.8–B94.9, B95–B99, G06, G07, O98.4–O98.6, O98.8–O98.9 | Only A38, A48.1 and O98.4–O98.6, O98.8–O98.9 classed as avoidable deaths. |
| C13(b) | Breast cancer | C50 | Only females classed as avoidable deaths |
| C46(b) | Acute lymphoblastic leukaemia | C91.0 | Only deaths among 0–44 year-olds classed as avoidable |
| C98 | Other malignant neoplasms (cancers) | C17, C21, C30–C31, C37–C38, C40–C41, C46–C49, C51–C52, C57–C58, C60, C63, C65–C66, C68–C69, C74–C75 | Only C21 classed as avoidable deaths. |
| D04 | Non–rheumatic valvular disease | I07, I08.2, I08.8–I08.9, I34–I39 | Only I34–I37 classed as avoidable deaths. |
| D07 | Inflammatory heart disease | I30–I33, I40–I41 | Only I33 classed as avoidable deaths. |
| D99 | Other cardiovascular diseases | G45, I26–I28, I44–I45, I47, I49.1–I49.9, I51–I52, I77–I84, I86–I89, I95, I97–I99 | Only I26, I51.1, I51.2, I51.4 and I51.5 classed as avoidable deaths. |
| F01 | Gastroduodenal disorders | K22.1, K25–K27, K29 | Only K25–K27 classed as avoidable deaths. |
| J01 | Chronic kidney disease | E10.2, E11.2, E12.2, E13.2, E14.2, I12, N02–N08, N13–N16, N18, N39.1–N39.2, Q61 | Only E10.2, E11.2, E12.2, E13.2, E14.2, I12 and N18 classed as avoidable deaths. |
| N05 | Skin infections (including Cellulitis) | A46, B08.1, B08.4, H00.0, H60.0, H60.1, J34.0, L00–L03, L08 | Only A46 and L03 classed as avoidable deaths. |
(a) Two ABDS causes (A13 and A14) were combined into A98 for reporting purposes.
(b) All ICD-10 codes in ABDS causes Breast cancer (cause code C13) and Acute lymphoblastic leukaemia (C46) are considered avoidable under restricted conditions. Breast cancer is considered avoidable only for females, and Acute lymphoblastic leukaemia is considered avoidable only for those aged 0–44 years.
Data from the National Mortality Database (NMD) were used to derive the avoidable fatal burden component for each of the 19 part-avoidable causes. Deaths were grouped into the 19 causes based on ICD-10 codes and ‘avoidable percentages’ were calculated. For each cause, avoidable percentages were based on the number of deaths occurring before age 75 which were classified as avoidable, divided by the total number of deaths before age 75 for that cause (see Table A4 for selected examples). Separate avoidable percentages were calculated for First Nations people and total Australians.
Avoidable percentages were applied to the fatal burden before age 75 from the 2018 ABDS to determine the avoidable fatal burden (AYLL) for each of the 19 part-avoidable causes.
| Cause | First Nations deaths | First Nations avoidable deaths | First Nations avoidable percent (%) | All deaths | Avoidable deaths | Avoidable percent (%) |
|---|---|---|---|---|---|---|
| LRI including influenza & pneumonia | 53 | 39 | 73.6 | 645 | 448 | 69.5 |
| Non-rheumatic valvular disease | 14 | 9 | 64.3 | 281 | 197 | 70.1 |
| Other cardiovascular diseases | 32 | 8 | 25.0 | 791 | 182 | 23.0 |
| Chronic kidney disease | 136 | 132 | 97.1 | 793 | 713 | 89.9 |
LRI lower respiratory infections
Notes:
- These causes are not directly equivalent to ABDS causes of the same name as only some of the ICD-10 codes included in the ABDS definitions are classified as avoidable deaths.
- The number of deaths in the ABDS database for each cause are slightly different from the number of deaths in the NMD (for the same causes) due to redistribution modelling in the ABDS.
Can I compare results with other ABDS studies?
Results from this study should not be compared with results for fatal burden (YLL) from other Australian Burden of Disease Studies (ABDS). Generally, overarching methods for estimating fatal burden remain unchanged from previous ABDS studies, however, some minor changes to methodology were required to facilitate the analysis by the smaller geographical areas of Indigenous Regions (IREGs). These changes may result in different results to those presented in other ABDS studies.
Indigenous Regions
Indigenous Regions (IREGs) are large geographic areas that are part of the Australian Statistical Geography Standard (ASGS) (ABS 2016). They were originally designed based on the former Aboriginal and Torres Strait Islander Commission boundaries which are no longer maintained. IREGs are created by combining one or more Indigenous Areas and do not cross state or territory borders (Figure A1). For the 2016 ASGS 58 Indigenous Regions are defined to cover the whole of geographic Australia, including several non-spatial special purpose codes (ABS 2016).
Figure A1: First Nations population (aged under 75) by Indigenous Region, 2018
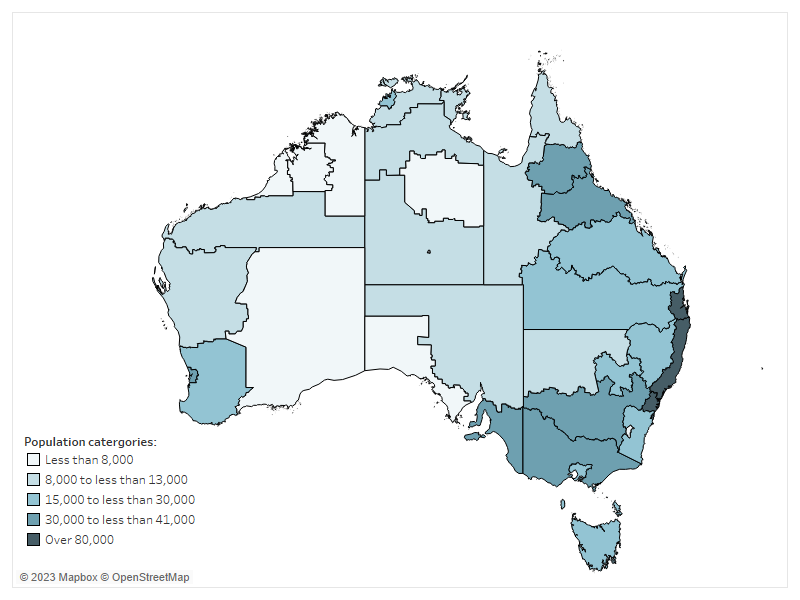
Chart: AIHW. Source: ABS 2016.
For the analyses in this report, 37 Indigenous Regions were able to be mapped to mortality and population data (Table A5).
| State/ territory | Indigenous Region |
|---|---|
| New South Wales |
|
| Victoria |
|
| Queensland |
|
| Western Australia |
|
| South Australia |
|
| Tasmania | Tasmania |
| Australian Capital Territory | ACT |
| Northern Territory |
|
Source: ABS 2016.
Mortality data
The total number of deaths come from the AIHW's National Mortality Database (NMD) which holds records for deaths in Australia from 1964 to 2021. The database comprises information about causes of death and other characteristics of the person, such as sex, age at death, area of usual residence and Indigenous status.
The cause of death data are sourced from the Registrars of Births, Deaths and Marriages in each state and territory, the National Coronial Information System and compiled and coded by the Australian Bureau of Statistics (ABS).
The AIHW website About our data – Deaths Data provides detailed information on the registration of deaths and coding of causes of death in Australia. The completeness, accuracy and coding of these data are described elsewhere (ABS 2022). The data quality statements underpinning the AIHW NMD can be found in the ABS’s quality declaration summary for Deaths, Australia and Causes of death, Australia.
Adjusting for under-identification of First Nations people in mortality data
Every year, a number of deaths of First Nations people are not identified as such when they are registered (ABS 2018). This might arise from the non-reporting of a deceased person’s Indigenous status on the death registration form (for example, the question is never asked, or the answer is not known), or from incorrect identification of a deceased person’s Indigenous status (recording an Aboriginal and Torres Strait Islander person as non-Indigenous, and vice versa). The net effect is an under-identification of First Nations people in the deaths data.
Adjustment factors to account for under-identification of First Nations people in death registration records have been produced from national and state/ territory data linkage studies. In the 2018 ABDS, mortality adjustment factors from the ABS’s Census Data Enhancement Indigenous Mortality Study (2015–17) (ABS 2018) were used to adjust First Nations deaths for under-identification in mortality data for the 2018 reference year. To maintain consistency, these factors were also used to adjust First Nations deaths for the calculation of avoidable percentages.
Dealing with small numbers
The number of deaths due to any cause varies from year to year. These fluctuations are more noticeable for causes that are less common and in First Nations deaths that are often small in number. To reduce the impact of random fluctuations, First Nations avoidable percentages were based on the annual average of 3 years of deaths data. For the 2018 reference year, First Nations deaths were averaged from deaths occurring in 2016, 2017 and 2018.
Redistribution issues
Some ICD-10 codes are not appropriate or valid causes of death for burden of disease analysis, either because they are implausible underlying causes (for example, hypertension), they are intermediate causes that have a precipitating cause (for example, septicaemia) or occur in the final stages of dying (for example, cardiac arrest), or they are recoded as ‘ill-defined’. Deaths assigned to these codes must be reallocated to one or more of the conditions defined on the ABDS cause list – this process is referred to as redistribution. Redistribution removes deaths from some causes, and increases the number of deaths for other causes, however the overall number of deaths is kept constant. Further details regarding methods for redistribution can be found in Australian Burden of Disease Study: Methods and supplementary material 2018 (AIHW 2021).
Some of the ICD10 codes used in the definition of avoidable deaths were allocated for redistribution in the ABDS (Table A1). Due to this aspect of burden of disease methodology there may be differences in the number of deaths reported here and in other mortality data studies.
Population data
Aboriginal and Torres Strait Islander backcast and projected population estimates as at 30 June 2018 (based on the 2016 Census) (ABS 2019) were used to calculate the rates for First Nations people presented in this report.
Non-Indigenous population estimates were calculated by subtracting the Aboriginal and Torres Strait Islander population estimates from the total Australian population estimates for the same years.
ABS (Australian Bureau of Statistics) (2016) Australian Statistical Geography Standard (ASGS): Volume 2 - Indigenous Structure, July 2016, accessed 12 January 2023.
ABS (2018) Life Tables for Aboriginal and Torres Strait Islander Australians, accessed 14 February 2023.
ABS (2019) Estimates and projections, Aboriginal and Torres Strait Islander Australians 2006–2031, accessed 14 February 2023.
ABS (2022) Causes of death, Australia methodology, 2021, accessed 12 May 2023.
AIHW (Australian Institute of Health and Welfare) (2021) Australian Burden of Disease Study: Methods and supplementary material 2018, accessed 1 March 2023.
AIHW (2022) National Healthcare Agreement: PI 16–Potentially avoidable deaths, 2022, accessed 9 February 2023.
Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C et al. 2012. GBD 2010: design, definitions, and metrics. The Lancet 380:2063–6.


