Changing trends
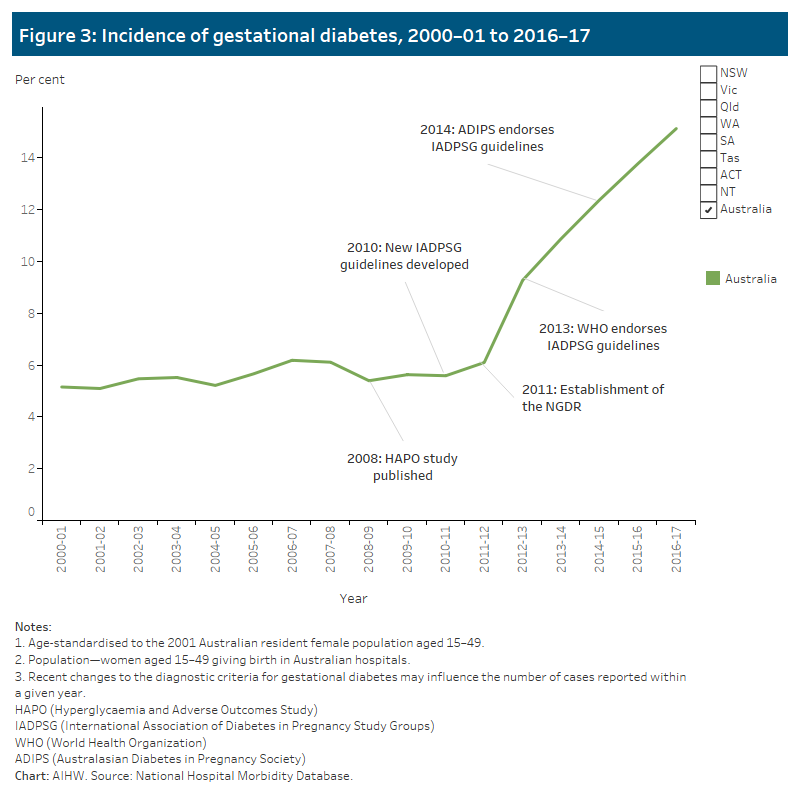
Between 2000–01 and 2016–17, the rate of women being diagnosed with gestational diabetes in Australia, tripled from 5% to 15% with steep increases recorded from 2012–13 (Figure 3).
This pattern of increase was seen across all age groups and all states and territories. Caution should be taken when comparing rates over time however, as a number of factors are likely to have affected the incidence of gestational diabetes in Australia in recent years. These include the introduction of new diagnostic guidelines and increasing risk factors in the population. Refer to Trends discussion for more information.
Trends discussion
Several factors are likely to have influenced the trend in the incidence of gestational diabetes in Australia in recent years, with notable increases recorded from 2012–13.
Changing guidelines for the testing and diagnosis of gestational diabetes
The Australasian Diabetes in Pregnancy Society (ADIPS) originally formulated national guidelines for the testing and diagnosis of gestational diabetes in 1991, based on expert opinion.
Publication of the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study in 2008 resulted in the development of new consensus guidelines for the testing and diagnosis of gestational diabetes in 2010, by the International Association of Diabetes and Pregnancy Study Groups (IADPSG) with Australasian representation. The HAPO study, a multinational observational study involving more than 23,000 women, found significant associations between adverse pregnancy outcomes and increasing maternal glucose levels, within what had previously been considered a non-diabetic range (HAPO Study Cooperative Research Group 2008).
Whilst the IADPSG guidelines were not endorsed by ADIPS until 2014, establishment of the National Gestational Diabetes Register (NGDR) by Diabetes Australia in 2011 (to assist in the post-natal support of women diagnosed with gestational diabetes and to remind them to have regular diabetes screening) and endorsement of the IADPSG guidelines by the World Health Organisation in 2013, may have had an impact on awareness and screening in Australia.
The endorsement of the IADPSG guidelines by ADIPS in 2014 represented a significant change to the practice of testing and diagnosing gestational diabetes in Australia. The guidelines were implemented across most jurisdictions by mid-2016. Reflecting international trends, Australian studies found increases in the number of women diagnosed with gestational diabetes, following the introduction of the IADPSG guidelines, of between 20% (Laafira et al. 2015), 35% (Moses et al. 2011) and 74% (Cade et al. 2019).
ADIPS guidelines: 1991–2014
The diagnostic pathway outlined in the 1991 ADIPS guidelines, involved a 2-step approach:
- Step 1: all women were screened for gestational diabetes using the non-fasting Glucose Challenge Test (GCT) at 24–28 weeks gestation, with high-risk women screened earlier in pregnancy.
- Step 2: women testing positive with the GCT were sent for diagnostic testing using the fasting Oral Glucose Tolerance Test (OGTT).
ADIPS diagnostic criteria: 1991–2014
- Fasting plasma glucose ≥5.5mmol/L; or
- Two-hour plasma glucose or random glucose ≥8.0mmol/L
As a screening test, the GCT had a high false-negative rate which may have resulted in women being under-diagnosed (van Leeuwen et al. 2012).
ADIPS guidelines: 2014–current
The new ADIPS guidelines (based on IADPSG) introduced two main changes to the diagnostic pathway for gestational diabetes:
- Firstly, the 2-step approach was replaced with a universal single-step 75g OGTT at 24–28 weeks gestation for all women, with high-risk women tested earlier in pregnancy.
- Secondly, new diagnostic criteria were introduced for the diagnosis of gestational diabetes with a lowering of the fasting, introduction of a one-hour and raising of the two-hour blood glucose thresholds.
IADPSG (ADIPS-endorsed) diagnostic criteria: 2014-current
- Fasting plasma glucose ≥5.1mmol/L; or
- One-hour post ≥10.0mmol/L; or
- Two-hour post ≥8.5mmol/L
Other factors
A number of other factors may influence gestational diabetes incidence rates. In particular, changes in the population associated with key risk factors, including:
Increasing overweight and obesity rates
Overweight and obesity is a known risk factor both for gestational (Nankervis et al. 2014) and type 2 diabetes (Ganz et al. 2014). National overweight and obesity rates in Australia have increased in recent decades, up from 56.3% in 1995 to 67% in 2017–18, largely driven by the increase in the proportion of those categorised as obese. Whilst a greater proportion of men than women are classified as overweight and obese, the pattern of increase is similar, with overweight and obesity rates for women increasing from 49.4% in 1995 to 59.7% in 2017–18 (ABS 2011, 2019). Among mothers who gave birth in 2017, one-fifth (20%) were classified as obese while just over a quarter (25.6%) were overweight (AIHW 2019).
Increasing maternal age
While the average age of women giving birth continues to rise from 29.9 years in 2007 to 30.6 years in 2017 (AIHW 2019), the influence of this factor has been controlled for in this report with age-standardisation of the data.
Immigration
Overseas migration continues to be a major contributor to Australia’s overall population growth. The country profile for those born overseas has changed significantly in recent decades with Asian countries comprising six of the top ten countries of birth in 2016 (ABS 2017).
Ethnicity is a known risk factor for gestational diabetes, with incidence higher among Asian, Indian subcontinent, Aboriginal, Torres Strait Islander, Pacific Islander, Maori, Middle Eastern, non-white African women (Nankervis et al. 2014). Using country of birth as a proxy for ethnicity, the results from this web report found in 2016–17, women born in Southern and Central Asia, South-East Asia and North Africa and the Middle East were more likely to be diagnosed with gestational diabetes than Australian born women.
References
ABS (Australian Bureau of Statistics) 2011. Overweight and Obesity in Adults in Australia: A Snapshot, 2007–08. ABS cat. no. 4842.0.55.001. Canberra: ABS.
ABS 2017. Cultural Diversity in Australia, 2016. ABS cat. no. 2071.0. Canberra: ABS.
ABS 2019. National Health Survey: First Results, 2017–18. ABS cat. no. 4364.0.55.001. Canberra: ABS.
AIHW (Australian Institute of Health and Welfare) 2019. Australia’s mothers and babies 2017—in brief. Perinatal statistics series no. 35. Cat. no. PER 100. Canberra: AIHW.
Cade TJ, Polyakov A & Brennecke SP 2019. Implications of the introduction of new criteria for the diagnosis of gestational diabetes: a health outcome and cost of care analysis. BMJ Open 2019:9:e023293. doi:10.1136/bmjopen-2018–023293.
Ganz ML, Wintfeld N, Li Q, Alas V, Langer J & Hammer M 2014. The association of body mass index with the risk of type 2 diabetes: a case-control study nested in an electronic health records system in the United States. Diabetology & Metabolic Syndrome 2014 6:50.
HAPO Study Cooperative Research Group, Metzger BE & Lowe LP 2018. Hyperglycemia and adverse pregnancy outcomes. New England Journal of Medicine 2008 358(19):1991–2002.
International Association of Diabetes and Pregnancy Study Groups Consensus Panel 2010. IADPSG recommendations for the Diagnosis and Classification of Hyperglycemia in Pregnancy. Diabetes Care 33(3):676–682.
Moses GR, Morris JG, Petocz P, San Gil F & Garg D 2011. The impact of potential new diagnostic criteria on the prevalence of gestational diabetes mellitus in Australia. The Medical Journal of Australia 194(7):338–340.
Nankervis A, Mclntyre H, Moses R, Ross G, Callaway L, Porter C et al. 2014. Australasian Diabetes in Pregnancy Society consensus guidelines for the testing and diagnosis of gestational diabetes mellitus in Australia. Sydney: ADIPS.
Van Leeuwen M, Louwerse MD, Opmeer BC, Limpens J, Serlie MJ, Reitsma JB et al. 2012. Glucose challenge test for detecting gestational diabetes mellitus: a systematic review. BJOG An International Journal of Obstetrics and Gynaecology 119(4):393–401.


