Explore the treatment pathways
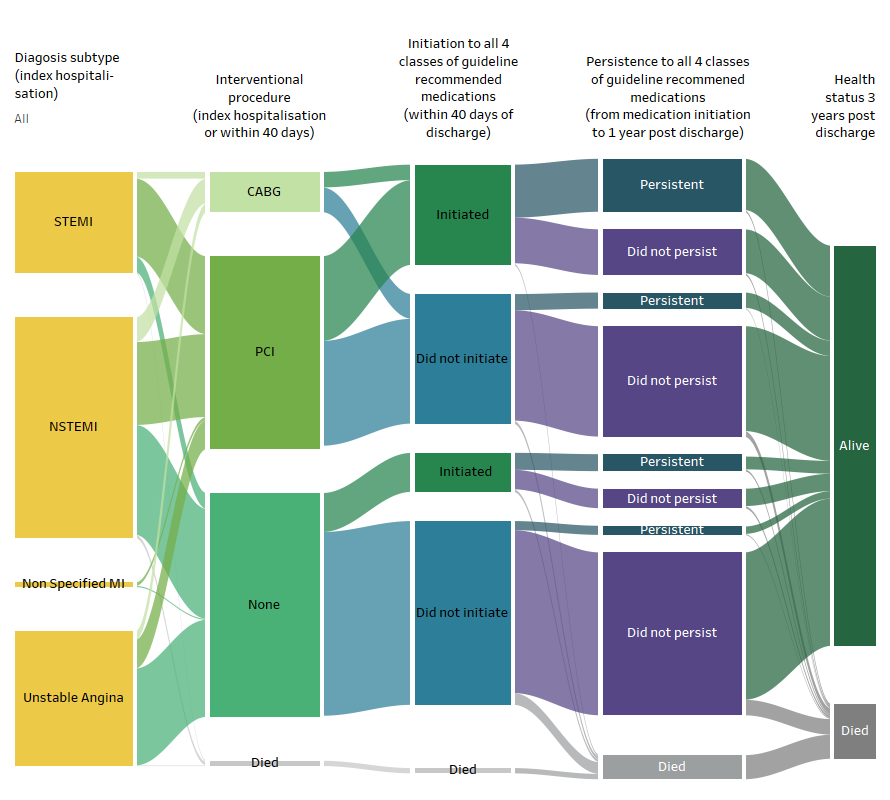
Treatment pathways of almost 35,800 people who survived an acute coronary syndrome (ACS) event are illustrated in Figure 3.
Figure 3: Treatment pathways and outcomes, by ACS subtype
The Sankey shows the proportion of people who followed different treatment pathways illustrated with the 3 measurement points and survival at 3 years.
Source: AIHW NIHSI 2016-17 to 2019-20, analysis of NIHSI
Peoples’ treatment pathways are described using 3 measurement points during or after their initial acute coronary syndrome hospitalisations (referred to as the “index hospitalisation” in this report). These measurement points were:
- Was an interventional procedure (percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG)) undertaken in the index hospitalisations or within 40 days of discharge? Interventional procedures were not measured for people who died within 40 days of discharge.
- Were all 4 classes of guideline recommended medications initiated (defined as being supplied) within 40 days of discharge from the index hospitalisation? Initiation was not measured for people who died within 40 days of discharge.
- Were all 4 classes of guideline recommended medications taken persistently, (defined as continuation without a gap in medication supply of 60 days or more) from first supply after hospitalisation until one year after? The first supply could be at any time in the first year, and at least 2 supplies were required. Persistence was not measured for people who died within 1 year of discharge.
Together, each of these measurement points were used to describe a person’s treatment pathway. For example, a treatment pathway may involve having an interventional procedure, being initiated to all 4 classes of medications but then not taking these persistently.
Outcomes reported include death within 40 days, 1 year and 3 years post index hospitalisation, emergency cardiovascular disease (CVD) hospital readmission, major adverse cardiac event (MACE), and CVD-specific death.
For details about the definitions used see About this project: Key variables.
Common treatment pathways
The most common pathway (taken by 36% of the ACS cohort) was that no interventional procedures were undertaken, they were not initiated to the guideline recommended medications, and at 1 year were alive but not persistent. Only 1 in 9 people (12%) received the most comprehensive treatment pathway (having an interventional procedure and medication initiation within 40 days, and at one year were alive and persistence to all 4 classes guideline recommended medications), however these varied considerably by diagnosis subtype.
Initiation to all 4 classes of guideline recommended medications was higher for people who had a procedure across all diagnosis groups in the cohort. (See Medication use for secondary prevention after coronary heart disease hospitalisations (AIHW, 2022) for detailed analysis of factors associated with medication initiation and persistence).
Variation in treatment pathways by diagnosis subtype
For people with ST segment elevation myocardial infarction (STEMI) (22% of the cohort), the 3 most common treatment pathways all involved an interventional procedure. The most comprehensive treatment pathway of an interventional procedure, initiation and persistence to all 4 classes of guideline recommended medications was taken by 27% of people with a STEMI diagnosis.
The two most common treatment pathways for people with a diagnosis of NSTEMI were either a procedure or no procedure followed by no initiation and no persistence to all 4 classes of guideline recommended medications.
People with unstable angina had the least variation in treatment pathways: 60% followed the pathway of no interventional procedures undertaken, not initiated to the guideline recommended medications, and not persistent.
The people who followed treatment pathways
People who did not have a procedure were more likely to be women, be aged 75-84, live in Outer regional, Remote and Very remote areas and have identified prior coronary heart disease (CHD), compared to those who had a procedure. This was consistent across all diagnosis groups.
The group who experienced the most comprehensive treatment pathway (an interventional procedure, initiation and persistence to all 4 classes of guideline recommended medications) and were alive at one year, compared to the group who had the least comprehensive treatment pathway (no interventional procedure, and no initiation or persistence) and also alive at one year, had:
- a higher proportion of men and people aged 45 to 65 years
- a higher proportion of people who lived in Major cities and areas of less socioeconomic disadvantage (in the STEMI cohort)
- a lower proportion of people with identified prior CHD and other comorbidities (in the STEMI and NSTEMI cohorts).
The outcomes experienced during and after treatment pathways
In the 3 years following the index hospitalisation, 21% of the cohort experienced a MACE, an outcome which involved an emergency readmission to hospital and/or death due to ACS, stroke, or heart failure. Thirty percent of the cohort had an emergency readmission due to cardiovascular disease (CVD) more broadly, and of the 12% of the total cohort who died in this period, 40% of these deaths were due to CVD (death with an underlying cause of CVD (ICD-10: I chapter)).
The groups who had interventional procedures generally experienced less adverse health outcomes, although there was less variation in health outcomes among those who did and did not undergo procedures for those with a diagnosis of unstable angina compared to other ACS subtypes.
For those with a STEMI diagnosis and alive at 1 year:
- adverse health outcomes were lowest among those who had the most comprehensive treatment pathways (an interventional procedure, initiation and persistence to all 4 classes of guideline recommended medications) (MACE: 12%).
- emergency readmissions and MACE were highest among those who did not undergo a procedure, and initiated medications at 40 days but were non-persistent at 1 year post discharge (32% and 25% for CVD readmissions and MACE respectively).


