Unstable angina
Angina is a chronic condition in which intermittent episodes of chest pain can occur when the heart has a temporary deficiency in blood supply. Unstable angina can be dangerous due to the changing severity in transient coronary narrowing. Of the acute coronary syndrome (ACS) cohort, 29% had a diagnosis of unstable angina.
- People with unstable angina were the most likely to not have followed any of the 3 treatment pathway measurement points, which was the least comprehensive treatment pathway.
- The rate of emergency CVD readmissions among people with unstable angina was the highest compared to the other diagnosis groups.
- People with unstable angina had the least variation in treatment pathways, 60% followed the same pathway of no interventional procedures undertaken, not initiated to the guideline recommended medications, and not persistent.
- Compared to other ACS subtypes, there was less variation in health outcomes among those who did and did not undergo procedures.
Explore the treatment pathways for the people with this diagnosis in Figure 8 and information about the people who followed theses pathways in Figure 9.
A summary of these pathways and the people who followed them is below.
Figure 8: Treatment pathways and outcomes, among those with unstable angina
The Sankey shows the proportion of people who followed different treatment pathways illustrated with the 3 measurement points and survival at 3 years.
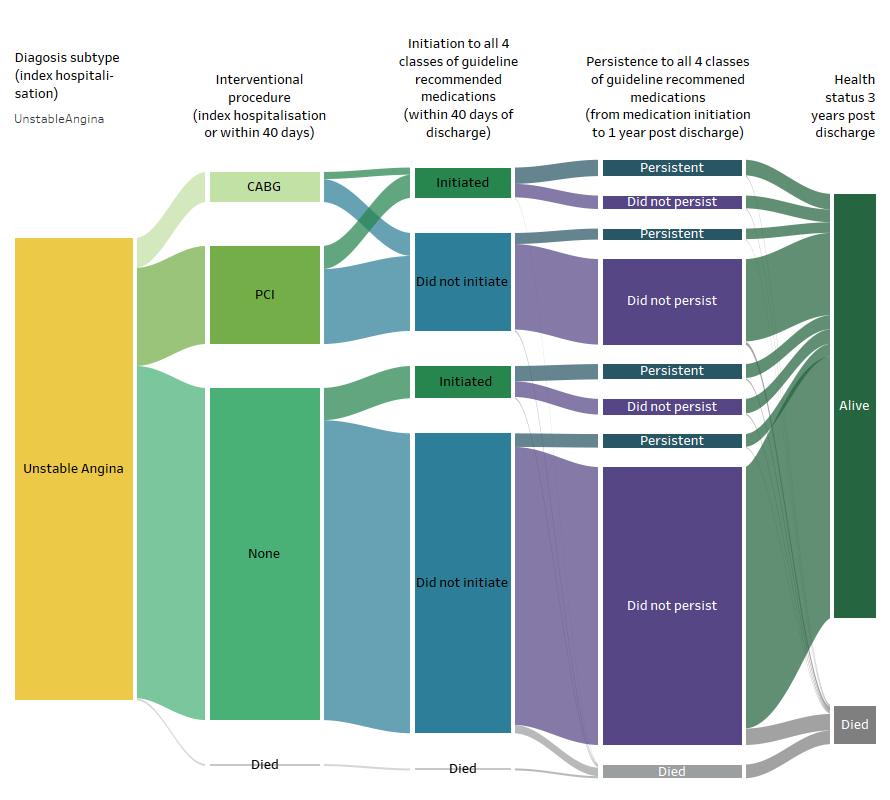
Source: AIHW NIHSI 2016–17 to 2019–20, analysis of NIHSI
Figure 9: Age group, sex, comorbidities, and health outcomes among those with unstable angina, by treatment subgroup
Figuresshow that among those with unstable angina, the most common age group is 55-64and comorbidity is a prior diagnosis of coronary heart disease.
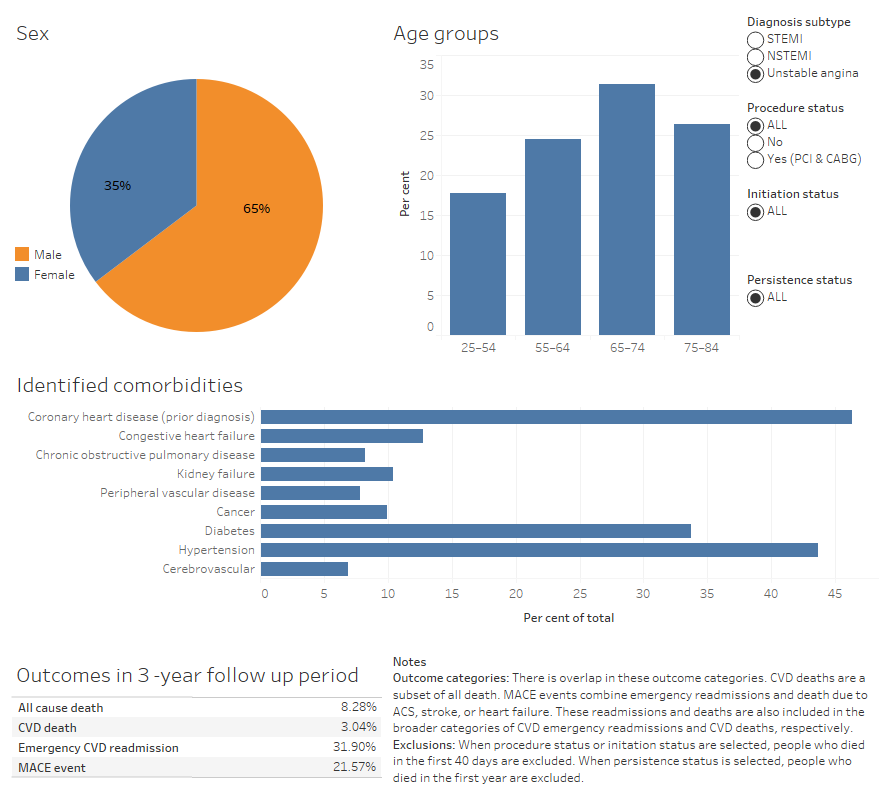
Source: AIHW NIHSI 2010–11 to 2019–20, analysis of NIHSI
People’s treatment pathways after an unstable angina hospitalisation
Peoples’ treatment pathways are described using 3 measurement points during or after their initial ACS hospitalisations (referred to as the index hospitalisation).
Note that differences in health outcomes experienced by people following different treatment pathways should not be interpreted as causal. Many factors, impact both treatment decisions and the risk of experiencing poor health outcomes.
Measurement point 1: Interventional procedure
Twenty eight percent of people with unstable angina had a procedure during the index stay or in the 40 days following hospital discharge. Noting, procedures undertaken after the index stay will be underestimated due to limited availability of private hospital data in the analysis. One in 14 people with unstable angina had a CABG procedure and 1 in 5 underwent a PCI procedure. Among those who underwent a CABG or PCI procedure, 17% and 23% were women, respectively. Forty one percent of those who did not have a procedure were women.
A slightly higher proportion of those who did not have a procedure were aged 25-54 years (19%) when compared to those who underwent CABG (11%) or PCI (16%).
When compared to other ACS subtypes, there was less variation in health outcomes among those who did and did not undergo procedures.
Measurement point 2: Medication initiation
Fourteen percent of those with unstable angina initiated all 4 classes of medicines at 40 days. Initiation to guideline indicated medications was higher among those who underwent a procedure (24%) compared with those who didn’t (10%).
Seventy one percent of those who did not undergo a procedure but initiated all 4 classes of medications had a prior CHD diagnosis compared with 45% in those who did not initiate medications. The proportion with a prior CHD hospitalisation was substantially lower among those who underwent a procedure (did not initiate: 43%, did initiate: 48%)
Those who underwent a procedure but did not initiate all guideline-indicated medications had the lowest proportion of people who experienced poor health outcomes (CVD readmission: 29%, MACE: 19%, all cause death: 5.2%). In contrast, those who did not have a procedure, but initiated 4 drug classes within 40 days, had the highest proportion of poor health outcomes when compared to other treatment subgroups (CVD readmission: 46%, MACE: 36%, all cause death: 12%). This group had a substantially higher proportion of people with identified comorbidities when compared to other treatment subgroups, which is likely to have impacted both treatment decisions and risk of experiencing adverse health outcomes.
Measurement point 3: Persistence to medication
Note, persistence measures are only estimated for those who were alive at 1 year. All comparisons below exclude people who died in the first year after index hospitalisation.
Of people with unstable angina, 61% did not have a procedure and did not initiate or persist with guideline indicated medicines.
Those with unstable angina who had a procedure but did not initiate or persist with guideline indicated medications at 1 year post hospitalisation had the lowest rate of adverse health outcomes (CVD readmission: 28%, MACE: 17%, all cause death: 3.7%). When compared to other treatment subgroups, this group had a lower proportion of women (20%), First Nations people (1.7%), and had a greater proportion of people living in higher socioeconomic areas (see supplementary table S5b).
In contrast, those who had no procedure, did not initiate medications at 40 days, but were classified as persistent at 1 year had the highest proportion of people with an emergency CVD readmission (58%) or MACE (46%). This group had a high proportion of people with prior CHD (74%) and other identified comorbidities (for example, diabetes: 50% and hypertension: 65%).
The subgroup with the highest rate of death was those who did not have a procedure but initiated and persisted with medications (8.7%). Two in 3 people in this subgroup were aged 65-74 years, and a high proportion of people had identified comorbidities when compared with other subgroups. For example, 3 in 4 had a prior CHD diagnosis, 1 in 4 had congestive heart failure, and 1 in 2 had diabetes.
See Figure 9 for comparisons of age group, sex, comorbidities and health outcomes among treatment groups.


