Technical notes
On this page:
- Population and expanded suicide monitoring period
- How does the expanded study population affect the results?
- ADF suicide deaths in the period 1 January 1985 to 31 December 1996
- Active and standby reserves
- Limitations in the study population
- Changes to previously published suicide information
- Australian Bureau of Statistics (ABS) changes to mortality coding over the study period
- Rates based on small numbers
- Suicide incidence rates
- Rehires
- Potential disparity due to dates mismatch between study cohort and suicide monitoring
- Standardised mortality ratios
- Age-standardised rates
- Cox proportional hazards model
- Confidence Intervals
- Using confidence intervals to test for statistical significance
- About the psychosocial risk factors coding work
- How is psychosocial and other risk factor coding conducted?
- Scope of psychosocial risk factor coding
- Revisions of risk factor coding
- Limitations in coding of risk factors
- ADF member specific risk factors
- Acronyms
- Data sources
Population and expanded suicide monitoring period
The population used in this report includes all ADF members who have served at least one day since 1 January 1985. As of 31 December 2020, almost 379,000 Australians had served at least one day in the ADF between 1 January 1985 and 31 December 2020. Of these, just over 362,000 were still alive, comprising 60,000 permanent, 39,000 reserve, and 263,000 ex-serving.
Since 1985, the ex-serving population with at least one day of service since 1 January 1985 has increased each year as permanent and reserve ADF members separate. At the end of 1985, almost 6,100 members had separated and by the end of 2020 this had grown to 277,000. Due to the method used to assemble the study population, as members leave the permanent and reserve service, they are counted as members of the ex-serving study population until they die.
The previous version of the report included ADF members who had served at least one day since 1 January 1985 with a suicide monitoring period of 1 January 2001 to 31 December 2019 with rates of suicide reported from 1 January 2002 to 31 December 2019. This discrepancy was due to data quality concerns in the national deaths index (NDI) data pre-2001. However, after further investigations it was determined that it was analytically sound to extend the monitoring period from 1 January 1997 to 31 December 2020. Concerns about NDI completeness prevent accurate detection via linkage of deaths by suicide before 1997.
For more information on the demographics of this population, see the report Serving and ex-serving Australian Defence Force members who have served since 1985: population characteristics 2019.
How does the expanded monitoring period affect the results?
The expanded monitoring period for reporting and analysis with the addition of those who died by suicide between 1997 to 2001 and in 2020 has resulted in an increase in the number of deaths by suicide reported relative to the previous report. This publication reported a total of 1,273 suicide deaths occurring between 2001 and 2019, whereas 1,600 suicides deaths are reported here (between 1997 and 2020). However, it is important to understand that this increased suicide count does not reflect a higher risk of suicide to the ADF population. Rather, the number of deaths by suicide identified has increased because we are reporting on deaths within an expanded monitoring period.
Care should be taken in comparing data in this report with previous AIHW publications. When comparing the results published here to those released in earlier updates, it is more useful to focus on suicide rates, as these give a better indication of the risk of suicide to different groups within the ADF population. As shown in Figure 24, the suicide rates have not significantly changed due to the expanded monitoring period, compared to those reported in the previous report.
Figure 24: Suicide rates by service status group and sex, of ADF members who have served at least one day since 1 January 1985 and have died by suicide from 1997–2020 and 2002–2019.
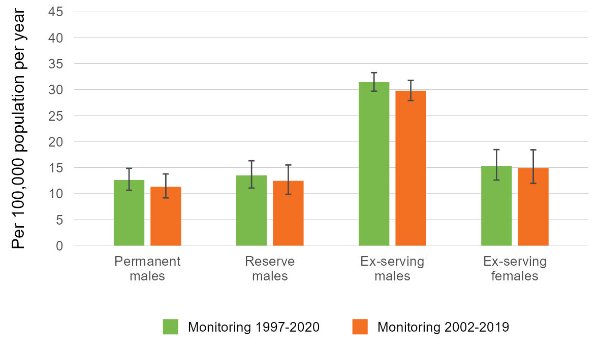
Source: AIHW analysis of linked Defence Historical Personnel data–PMKeyS–NDI data 1985–2020; NMD 1997–2020; Defence population snapshots, 2002–2020.
ADF suicide deaths in the period 1 January 1985 to 31 December 1996
This publication reports 1,600 confirmed suicide deaths that occurred between 1 January 1997 to 31 December 2020 among ADF members who have served at least one day since 1 January 1985.
It should be noted that an additional 330 confirmed suicide deaths were discovered by analysis of the period 1 January 1985 and 31 December 1996, meaning a total of 1,930 confirmed suicide deaths that occurred between 1 January 1985 to 31 December 2020 among ADF members who have served at least one day since 1 January 1985.
Confirmed suicide deaths prior to 1997 were not included in this analysis as these are under reported compared to the suicides identified post-1997, due to the quality and completeness National Death Index (NDI) dataset, as there are gaps in identifying data in the NDI which limits the ability to link to Defence personnel data. Therefore, while we are confident that all the confirmed suicides included are true ADF member confirmed suicides, there may be more unlinked and unknown. As such any population study analysis of suicide deaths during this period would be misleading.
For completeness, the number of discovered suicides per year 1985-1997 is given below in Table 13.
| Year | Permanent and reserve | Ex-serving | Total in all ADF service groups(a) |
|---|---|---|---|
|
1985 |
n.p. |
n.p. |
13 |
|
1986 |
n.p. |
n.p. |
7 |
|
1987 |
n.p. |
n.p. |
11 |
|
1988 |
n.p. |
n.p. |
11 |
|
1989 |
9 |
15 |
24 |
|
1990 |
7 |
16 |
23 |
|
1991 |
11 |
17 |
28 |
|
1992 |
11 |
22 |
33 |
|
1993 |
14 |
31 |
45 |
|
1994 |
8 |
35 |
43 |
|
1995 |
9 |
39 |
48 |
|
1996 |
13 |
31 |
44 |
|
Total(b) |
112 |
218 |
330 |
n.p. Not available for publication but included in totals where applicable, unless otherwise indicated. In this case this is a result of low numbers being potentially identifying.
Notes:
- Consists of deaths by suicide in males and females for permanent, reserve and ex-serving ADF members.
- Suicide numbers are likely to be under-reported for this period 1985 to 1996 as there are gaps in identifying data in the National Deaths Index (NDI) which limits the ability to link to Defence personnel data. Therefore, while we are confident that all the confirmed suicides included are true ADF member confirmed suicides, there may be more unlinked and unknown.
Source: AIHW analysis of linked Defence historical personnel data–PMKeyS–NDI data 1985–2020.
Active and standby reserves
The active and standby reserve cohorts were aggregated in this report. Despite having difference levels of commitment to the ADF (see Box 1) the suicide rates for these subgroups are statistically similar.
Figure 25 below demonstrates this for males. The values for females are not reported due to low numbers of suicides.
Figure 25: Suicide rates for active and standby reserve males who served 1 January 1985 and have died by suicide between 1997 and 2020.
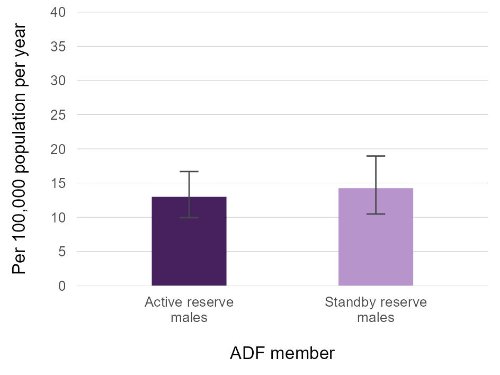
Source: AIHW analysis of linked Defence historical personnel data–PMKeyS–NDI data 1985–2020.
Limitations in the study population
The study population does not include ADF members with service prior to 1 January 1985. The analysis is constrained by technical limitations in Department of Defence systems and information infrastructure for records before 1985.
Changes to previously published suicide information
An additional 327 suicide deaths are reported here compared to the 2021 report. The breakdown of changes in the number of suicide deaths reported is as follows:
- 241 suicide deaths between 1997 and 2000 in members who separated between 1 January 1985 and 31 December 2001 (and were therefore previously out of scope)
- 79 suicide deaths that occurred in 2020
- 7 additional suicide deaths identified in 2019 due to a lag in reporting cause of death
- 7 additional suicide deaths identified in 2010 (2), 2014 (2), and 2018 (3) due to newly identified linkages
- 6 fewer deaths in 2008 (1), 2011 (1), 2012 (1), 2014 (2) and 2015 (1) due to the omission of Defence Suicide Database (DSD) identified deaths (see Data Sources for further information)
- 2 fewer deaths in 2007 (1) and 2015 (1) due to updates in cause of death information in the National Death Index (NDI)
- 1 additional suicide that occurred between 2001 and 2007 that was previously not reported where precise date of death year was not recorded in the NDI.
As well as the expansion of the suicide monitoring period and addition of a new year of cause of death data, there are three main reasons for changes to previously published suicide results, as described below.
Analysis in this study is based on year of occurrence of death. The NDI is the source of information on fact of death in this study. Fact of death information from the NDI is supplemented with cause of death information from the National Mortality Database (NMD). Results published in the report Serving and ex-serving Australian Defence Force members who have served since 1985: suicide monitoring 2001 to 2019 for deaths that occurred in 2019 were based on preliminary cause of death information from the NMD. This was the most recent version of cause of death information at the time of reporting.
Analysis of the NMD for all Australian deaths shows that between 4% and 7% of deaths are not registered until the next year (ABS 2018). These deaths are not captured in cause of death information, until data for the next year become available. This means that while fact of death information was complete for 2019 at the time of publishing the report Serving and ex-serving Australian Defence Force members who have served since 1985: suicide monitoring 2001 to 2019, cause of death information was missing for a number of deaths included in the analysis at that time. Additional suicides that occurred in 2019 but that were not registered until 2020 have now been identified with the inclusion of preliminary 2020 cause of death information in the current results.
Cause of death information for the Serving and ex-serving Australian Defence Force members who have served since 1985: detailed analysis from 1997 to 2020 release is based on final cause of death information for the years 2001 to 2018. Revised data are used for 2019 and preliminary data for 2020. Cause of death for a small number of records linked to the 2019 (revised) and 2020 (preliminary) cause of death data may change where a death is being investigated by a coroner and more up-to-date information becomes available as a result of the ABS revisions process. This may have a small effect on the number of deaths attributed to suicide in these years, as some deaths currently coded as ‘undetermined intent’ could later be identified as ‘intentional self-harm’ (or vice-versa).
Although this method likely captures the vast majority of suicides, there is potential for some to be missed if coronial findings take longer than four years and the finding results in an update to the initial coded intent of death.
Care needs to be taken when interpreting data derived from deaths registered in Victoria. Following investigations between the ABS and the Victorian Registry of Births, Deaths and Marriages, 2,812 additional registrations from 2017, 2018 and 2019 were identified that had not previously been provided to the ABS. A time series adjustment has been applied to these deaths to enable a more accurate comparison of mortality over time. Affected deaths are presented in the year in which they were registered (i.e. removed from 2020 and added to 2018 or 2019). For detailed information on this issue please refer to Technical note: Victorian additional registrations and time series adjustments in Causes of death, Australia (ABS cat. no. 3303.0) available from the ABS website.
Changes to previously published results may also occur as additional information becomes available to the study.
For example, differences in data collection methods and policy around timing of death registration can affect when and how the data is recorded in the ABS collection. Data users should note the potential impact of these changes when making comparisons between reference periods. While such changes will not explain all differences between years, they are a factor that may influence the magnitude of any changes in suicide numbers as revisions are applied (ABS 2018).
Improvements in available information and linkage processes over time have also resulted in additional suicides being identified for periods previously reported on.
Australian Bureau of Statistics (ABS) changes to mortality coding over the study period
The following information on mortality coding is sourced from the ABS. For further information, see the ABS Causes of death, Australia report (ABS 2018).
Substantial changes to ABS cause of death coding were undertaken in 2006, improving data quality by enabling the revision of cause of death for open coroner’s cases over time. Deaths that are referred to a coroner (including deaths due to suicide) can take time to be fully investigated. To account for this, all coroner-certified deaths registered after 1 January 2006 are subject to a revisions process. This allows cause of death for open coroner’s cases to be included at a later stage where the case is closed during the revision period. Cause of death data are deemed preliminary when first published, with revised and final versions of the data being historically published 12 and 24 months after initial processing. Between 2001 and 2005, revisions did not take place and as such it is recognised by the ABS that deaths by suicide may have been understated during this period (ABS 2018).
As well as the above changes, new coding guidelines were applied to deaths registered from 1 January 2007. The new guidelines improve data quality by enabling deaths to be coded as suicide by ABS mortality coders if evidence from police reports, toxicology reports, autopsy reports and coroners’ findings indicates the death was due to suicide. Previously, coding rules required a coroner to determine a death as due to suicide for it to be coded as suicide.
The combined result of both changes has been the more complete capture of deaths by suicide, and a reduced number of deaths coded as ‘undetermined intent’, within Australian mortality data. The NCIS also continually makes improvements and enhancements to their system which allows for ABS coding to be accessed in a more timely fashion.
Detailed information on coding guidelines for intentional self-harm, and administrative and system changes that can have an impact on the mortality data set, can be found in Explanatory Notes 91-100 of Causes of death, Australia report (ABS 2018).
Rates based on small numbers
Rates based on small numbers of events can fluctuate from year to year for reasons other than a true change in the underlying risk of the event.
In this report, rates are not reported when there are fewer than 5 events, as rates produced using small numbers can be sensitive to small changes in counts of deaths over time.
Suicide incidence rates
This report uses incidence rates to measure how often suicide occurs amongst the three ADF service groups, as well as in the Australian population. The incidence rate is the total number of deaths by suicide in a population over a specific period of time, divided by population time at risk during this time. In this study, the sum of the population at 30 June in each year of the relevant period is used as a proxy for population time at risk. Suicide incidence rates are expressed as the number of deaths per 100,000 population per year.
Rehires
In previous years, a complex procedure was used to identify rehires between Defence personnel (PMKeyS) data extracts, and include these individuals in the ex-serving population in the time between re-hires. This was not possible this year, so it may be that the total ex-serving population is slightly underestimated.
Potential disparity due to dates mismatch between study cohort and suicide monitoring
The study population used in this report comprises of all members with ADF service since 1 January 1985, whereas suicide rates are calculated from 1997 to 2020. This gap between the beginning of the study period (1985) and the monitoring period (1997), meaning there are suicides from the period 1985 to 1996 that are not captured in this analysis.
This approach risks introducing uncertainty, since the suicide rates before 1997 are unknown, and unable to be determined due to the data limitations. While regrettable, ultimately the study gains a lot by including this cohort.
This is not an issue for the Cox Proportional Hazards section, where the study population only includes those who separated during or after 1997 (or 2003).
Standardised mortality ratios
Age-adjusted comparisons between the suicide rate in each of the three ADF service status groups and the Australian population were calculated using Standardised Mortality Ratios (SMRs). The SMR is a widely recognised measure used to account for differences in age structures when comparing death rates between populations. This method of standardisation can be used when analysing relatively rare events, that is, where number of deaths is less than 25 for the analysed time period. The SMR is used to control for the fact that the three ADF service status groups have a younger age profile than the Australian population, and rates of suicide vary by age in both the study populations and the Australian population. The SMRs control for these differences, enabling comparisons of suicide counts between the three service status groups and Australia without the confounding effect of differences in age.
The SMR is calculated as the observed number of events (deaths by suicide) in the study population divided by the number of events that would be expected if the study population had the same age and sex specific rates as the comparison population. SMRs greater than 1.0 indicate a greater number of suicides in the ADF population than expected; and SMRs less than 1.0 indicate a lower number of suicides than expected in the ADF population.
Unlike suicide rates, SMRs only provide information about the two populations the statistic is based on. Comparing SMRs cannot be used to draw conclusions about the relative adjusted mortality rates of the study populations. This is because each SMR measure provides a comparison that is specific to the two populations involved.
Comparisons with the Australian population are not calculated for other breakdowns such as by rank and reason for separation as only adjusting for age and sex does not account for all the differences in the populations. In addition, it is considered more useful to compare between the different levels of these groups rather than with the Australian population.
Age-standardised rates
Age-standardised rates are incidence rates that enable comparisons between populations that have different age structures and over time as the age structure of the population of interest may change. This effectively removes the influence of the age structure on the summary rate—it is the overall death rate that would have prevailed in the standard population if it had experienced at each age the death rates of the population under study.
Direct standardisation was used in this report. To calculate age-standardised rates, age-specific rates were multiplied against a standard population. Directly age-standardised rates were adjusted using the current Australian standard population (that is, the non-recast Australian estimated resident population (ERP) as at 30 June 2001).
Rates are expressed as per 100,000 per population years (AIHW 2022).
Cox proportional hazards model
Survival analysis models the time it takes for an ‘event’ to occur after some ‘intervention’, termed ‘survival time’. The Cox proportional hazards regression model (Cox 1972) is the most common tool for studying the dependency of survival time on one or more predictor variables.
In this report the event measured is death by suicide, and the intervention is separation from the ADF. Each individual enters the model on their separation date, and is censored from further contribution at the point of their death (not by suicide) or on data extract date (31 December 2020) if they are alive. Calculations are then made based on the occurrences of suicide among the model population.
The ‘survival’ package in the statistical computing software R was used to fit the Cox models presented in this study (Fox 2018).
The purpose of modelling is to evaluate simultaneously the effect of multiple factors on the risk of death by suicide at a point in time. This risk is referred to as the hazard rate. The hazard ratios (HRs) that are reported in this study compare hazard rates between groups within a variable relative to a reference group.
- A HR > 1 indicates that a group is associated with a higher occurrence of suicide
- HR < 1 indicates that a group is associated with a lower occurrence of suicide
- HR = 1 suggests no effect.
If the HR 95% CI includes the value 1, then that suggests there is no strong evidence the group has an effect on the occurrence of suicide. HRs within models can be directly compared, giving rates of interactions between variables while holding all other values constant.
A key assumption of the Cox model is that the effect or hazard for each group within a variable remains proportional over time (the proportional hazards assumption). Tests for proportional hazards were performed on the models presented and, for each variable and each model, the proportional hazards assumption was supported.
Confidence Intervals
This report uses confidence intervals of 95% in the calculation of rates, SMRs and HRs. Broadly speaking wider CIs imply less certainty around a calculated value, and narrower CIs imply more certainty. Specifically, a CI at 95% suggests that repeated samples calculating the CI in the same manner would contain the true value 95% of the time.
Using confidence intervals to test for statistical significance
Statistical significance is based on a measure that indicates how likely it is that an observed difference, or a larger one, would occur under the conditions of the null hypothesis.
In this study, 95% confidence intervals (CIs) are provided for each standardised mortality ratio (SMR) and suicide rate to indicate the level of uncertainty around these estimates due to random fluctuations in the number of suicides over time. Estimates produced using low numbers can be sensitive to small changes in numbers of deaths over time and will therefore have wide CIs. CIs at 95% are provided within this report as they may account for the variation in absolute numbers of deaths by suicide over time (related to the small sample size). These assume that the suicide counts used in this analysis can be described by a Poisson distribution.
It is important to note that there are other sources of uncertainty, such as the linkage error, that are not captured by the provided CIs.
Use of CIs is the simplest way to test for significant differences between service groups and Australian comparison groups. For the purpose of this report, differences are deemed to be statistically significant if CIs do not overlap with each other (when comparing suicide rates) or 1.0 (in the case of an SMR). The CIs in this report cannot be used to determine the significance of differences between rates calculated for overlapping 3-year time periods.
Where the CIs are wide, for example in the case of the SMR for ex-serving females, sensitivity analysis was conducted. This analysis found that slight changes to the numbers of suicides did not significantly alter the result.
About the psychosocial risk factors coding work
The findings presented in the psychosocial risk factors section are from analysis of data produced as an extension of causes of death coding conducted by the Australian Bureau of Statistics (ABS) (see ABS 2021a). Mortality data and statistics are produced through collaboration of multiple jurisdictions and organisations. Registries of Births, Deaths and Marriages in each State and Territory register deaths in their respective jurisdictions and supply information about the cause of death (including from medical practitioners and coroners) to the ABS. The ABS uses this information and coronial reports sourced from the National Coronial Information System (NCIS) to review and code causes of death in each case, using the International Statistical Classification of Diseases and Related Health Problems, version 10 (ICD-10) (WHO 2019). For deaths by suicide, the ABS relies on NCIS reports, including police, toxicology, autopsy and coronial findings. The causes of death codes determined by the ABS are used in reporting on Australian mortality statistics (collated in the National Mortality Database).
The ABS code multiple causes of death to codes for individual deaths, identifying one underlying cause of death as well as associated causes of death. While the underlying cause of death is the primary cause, the associated causes of death are ‘any intervening causes, and those conditions that contributed to death but were not related to the disease or condition causing death’ (ABS 2021a). Since 2017, the ABS has expanded on the associated causes captured to include psychosocial risk factors for deaths referred to a coroner, funded by the National Suicide and Self-harm Monitoring Project (see ABS 2019; AIHW 2021a).
How is psychosocial and other risk factor coding conducted?
This report presents information on risk factors which were coded by analysts at the ABS from coronial case investigation reports contained in the National Coronial Information System (NCIS). Police, toxicology, pathology and coronial finding reports were all analysed in order to assign ICD-10 codes that represent risk factors that may have affected a person’s decision to take their own life. In addition, the ABS reviewed the underlying cause of death and injury for each ADF member and updated these if necessary.
The definition of risk factors included mental and behavioural disorders, drug and alcohol use, chronic disease, chronic pain and lifestyle factors. In addition to this the underlying cause of death and injury was reviewed for each case and updated if necessary.
|
Category |
Description |
ICD Chapter Reference |
Examples |
|---|---|---|---|
|
Natural Disease |
Natural disease, as defined by the ABS, includes ‘all disease and health related conditions with the exclusion of mental and behavioural disorders, injuries, and external causes’ (ABS 2019). Excludes some terminal conditions. Note that natural disease codes cover currently active disease and that past issues with health status and care that affected lifestyle are generally captured in psychosocial risk factors. |
These correspond with the ICD‑10 codes A00-E90 and G00-R99, U071-U072, U08-U09. Excludes G93, J96, I46, I49, R688, R57, R58. |
Chronic pain, insomnia, findings of drugs and alcohol in blood. |
|
Mental and Behavioural Disorders |
Mental and behavioural disorders, defined as ‘a clinically recognizable set of symptoms or behaviours associated in most cases with distress and with interference with personal functions’ (WHO 1992). |
ICD-10 codes F00-F99. |
Depression, post-traumatic stress disorder (PTSD), anxiety disorders. |
|
Psychosocial Risk Factors |
ABS define psychosocial risk factors ‘social processes and social structures which can have an interaction with individual thought or behaviour and health outcomes’ (ABS 2019). |
ICD-10 codes Z00-Z99 |
Family disruption, employment status, legal issues. |
Note that for the Australian population, the presence of natural disease risk factors was confirmed by the assessment of ICD codes present in part 2, line 6 of an individual's death certificate. This was to ensure that natural disease ICD-10 codes were indeed associated causes of death and not modes of death. It is acknowledged that the natural disease associated causes may be recorded elsewhere on a death certificate due to the space limitations if many associated causes were recorded for an individual, and therefore would not be included in this analysis. However, this affects a small number of individual records.
For further information on the methodology developed by the ABS, in consultation with stakeholders, see Psychosocial risk factors as they relate to coroner-referred deaths in Australia | Australian Bureau of Statistics (abs.gov.au) (ABS 2019).
Scope of psychosocial risk factor coding
This report presents information on psychosocial risk factors for ADF members who died by suicide between 1 January 2001 and 31 December 2020, and who had served at least one day since 1 January 1985.
The ABS used information (coronial reports) from the National Coronial Information System (NCIS) for coding associated causes of death and psychosocial risk factors. The NCIS is limited in that it only includes a nationally complete set of records from 1 January 2001 onwards, there is no centralised death information available prior to this. Therefore, the ABS coding is limited to deaths after 1 January 2001.
Mortality identifiers, also known as Mortality IDs, were used to identify ADF members who died by suicide in the NCIS. Records for 1,354 of the 1,359 ADF member deaths by suicide during the period (deaths that occurred between 1 January 2001 and 31 December 2020) were available for coding, as 5 cases did not link to a record in the NCIS. Cases may not have linked to the NCIS for several reasons, including a change in NCIS ID through time. All five cases occurred between 2001 and 2005.
The ABS piloted a project (ABS 2019) analysing information from the National Coronial Information System (NCIS) to capture psychosocial risks for deaths referred to a coroner in 2017 (ABS 2019). The ABS subsequently coded psychosocial risk factors for all Australian suicides 2017–2020 which are available for analysis in the National Mortality Database (NMD) (see also ABS 2021b).
In this report risk factors are presented for Australian male and females who died by suicide where the death was registered in 2018 (sourced from the NMD). The most recent year of data for which the causes of death data are considered ‘final’ and no longer subject to revisions was 2018. Data includes 90 deaths by suicide which were registered in Victoria in 2018 but were not supplied to the ABS until 2019 due to an issue associated with the Victorian Registry's previous processing system. The causes of death information for these cases are considered revised, not final.
Revisions of risk factor coding
As with underlying cause of death information (see above technical note), some coronial cases were open at the time that the ABS initially coded psychosocial risk factors, and further psychosocial risk factors may be identified as the coronial investigation is finalised. In the ADF member cohort there were 51 open cases that could not be coded further at this time.
For Australian deaths by suicide registered since 2017, the ABS revise the coding of causes of death (including psychosocial risk factors) 2 years after a case is opened. The revised coding of causes of death may result in an increase in the proportion of suicides with psychosocial or other risk factors. Data presented for Australian males and females in this report were for deaths registered in 2018 which are considered final and no longer revised.
Limitations in coding of risk factors
The ABS used information sourced from the National Coronial Information System (NCIS) for coding associated causes of death and psychosocial risk factors. The data available in the NCIS for coding reflects the information that was recorded during the coronial investigation of deaths referred to a coroner. The information available for each case of suicide varies depending on the comprehensiveness of the information collected during the investigation. Australian jurisdictions are governed by different Coronial Acts and ‘there will be differences in the processes, type and comprehensiveness of data collection’ between different States and Territories (NCIS n.d.).
To consider a factor as an associated risk to a suicide the information must first be reported as part of the investigative process into death. Secondly for the ABS to include that information as in the ICD-10 coded datasets that information must be made available on the NCIS (ABS 2019; 2021). The coding of risk factors ‘does not necessarily reflect all causes associated with all suicides that have occurred’ (ABS 2021b)
The coded data for ADF members produced by the ABS for the current study will differ from that which is nationally available. Coding of associated causes of death (including psychosocial risk factors) for Australian males and females who died by suicide undergoes a final revision 2 years after the death was registered and is not updated further. For ADF members who died by suicide in the study scope, coding in this study was based on the most updated information recorded in the NCIS regardless of whether the death had been registered more than 2 years previously. The data produced from this project should not be directly compared with other outputs that have used only the National Mortality Database (NMD). Additionally, a specific code was used for the ADF member cohort in the current study (see below).
ADF member specific risk factors
For the purposes of this project, the ABS used a specific code to record ‘defence force related deployment’ as a risk factor in psychosocial coding. The ABS has used the code Z65.9 which is allocated as ‘Problem related to unspecified psychosocial circumstances’ in the ICD-10. The Defence force related deployment code is not used in the coding of psychosocial risk factors for suicides among the Australian population. The code ‘exposure to disaster, war and other hostilities’ in the ICD-10 is used to code risk factors for both the ADF member and the Australian cohorts to capture exposure to military operations. Where both codes are captured for the same ADF member, this indicates the defence related deployment in warlike circumstances. In the report, these codes are captured in the group ‘other problems related to psychosocial circumstances’ (Z655-Z659).


