How did dementia death rates during 2020 compare to recent years (2015-19)?
Key findings
The age-standardised death rate with dementia was lower overall during the first 10 months of 2020, compared to the average age-standardised death rate for 2015–19; this was true for both men and women and for both age-groups examined (75–84 and 85+ years)
The age-standardised death rate due to dementia:
- over the first 10 months of 2020 was similar to the average rate for 2015–19
- was slightly higher among people aged 85 and over during wave 1 of the pandemic compared with the average rate for 2015–19
- was much lower during wave 2 of the pandemic compared to the average rate for 2015–19, which may indicate that public health measures to contain the virus had a positive effect on reducing deaths among people with dementia.
COVID-19 is a disease caused by a new type of coronavirus – a large group of viruses known to cause respiratory infections. About 99% of COVID-19 deaths in Australia have been confirmed by laboratory testing (ABSa 2020). The data used in this report include both medical doctor and coroner certified deaths due to COVID-19.
Due to the public health importance of COVID-19, the WHO has directed that the new coronavirus strain be recorded as the underlying cause of death, that is, the main disease or condition causing death, when it is recorded as having caused or contributed to death. In Australia, it is rare for COVID-19 to be coded as an associated cause of death (ABS 2020b).
Data and period of analysis
This report uses ABS provisional mortality data, covering deaths that occurred in the first 10 months of 2020 (between 1 January and 27 October). This includes most deaths that occurred from the beginning of the pandemic in Australia to the end of the second Victorian outbreak in 2020.
This report refers to 2 ‘waves’ of the COVID-19 pandemic in Australia – by this we mean a rapid increase in the number of infections, a peak, and then a decline in the number of infections:
- wave 1 (from 4 March to 26 May) occurred mostly in New South Wales, was shorter than wave 2, and resulted in fewer COVID-19 deaths than wave 2
- wave 2 (from 24 June to 27 October) occurred mostly in Victoria, led to extended lockdown measures particularly in Greater Melbourne, and was when most of Australia’s COVID-19 deaths occurred.
People who died due to or with dementia
People with dementia may die due to their dementia or from other conditions or injuries (such as influenza or a fall), so dementia may be recorded as an underlying or an associated cause of death on death certificate. In this report, people with dementia are looked at in two groups based on where dementia was recorded in the death certificate:
- deaths due to dementia refer to deaths where dementia was the underlying cause of death
- deaths with dementia refer to deaths were there was any record of dementia (as the underlying cause or an associated cause of death). About 3 in 5 of these deaths were deaths due to dementia.
Most of the information in this report relates only to deaths that were certified by a medical doctor. At the time of writing, coroner-certified deaths were only available when a person died due to COVID-19 (and these are included in this report). However, roughly 1–2% of deaths where dementia is recorded as an underlying cause of death are usually certified by a coroner. While the analyses in this report are unlikely to be significantly affected by missing coroner certified deaths, the data are considered preliminary and subject to change, and results should be interpreted with caution. In an unknown proportion of cases, dementia may not be recorded at all, either because it is incorrectly missed from the death certificate or because the dementia legitimately did not contribute to death. As a result, the number of people with dementia recorded on their death certificate will not capture every person with dementia who died during the pandemic.
In this section, the short-term impacts of the COVID-19 pandemic on people who died during the first 10 months of 2020 and had dementia recorded on their death certificate, is assessed by comparing the age-standardised death rate in the first 10 months of 2020 with the average age-standardised rate over the same months in previous years (2015–19).
The average of 2015–19 was selected because in Australia, the age-standardised rate of deaths among people with dementia recorded on their death certificate has remained relatively stable over this period. Increases in the number of people who die from dementia over time is mainly a result of the ageing Australian population. The section below presents information on recent trends in deaths data on dementia and other common causes of deaths in Australia.
In Australia, death rates usually vary by demographic and socioeconomic characteristics of the population for most conditions, including dementia. For example, death rates tend to be slightly higher for people with dementia living in the lowest socioeconomic areas compared with the highest socioeconomic areas. As we aim to assess the impact of the COVID-19 pandemic on dementia mortality and not just to describe known patterns of dementia mortality, our key findings focus on describing mortality patterns among people who died with dementia recorded on their death certificate in 2020 relative to average trends in recent years (2015–19). For more information about demographic patterns in dementia mortality in Australia before the COVID-19 pandemic, refer to the AIHW report: Mortality over regions and time (MORT) books.
How do we measure the short-term effects of the pandemic?
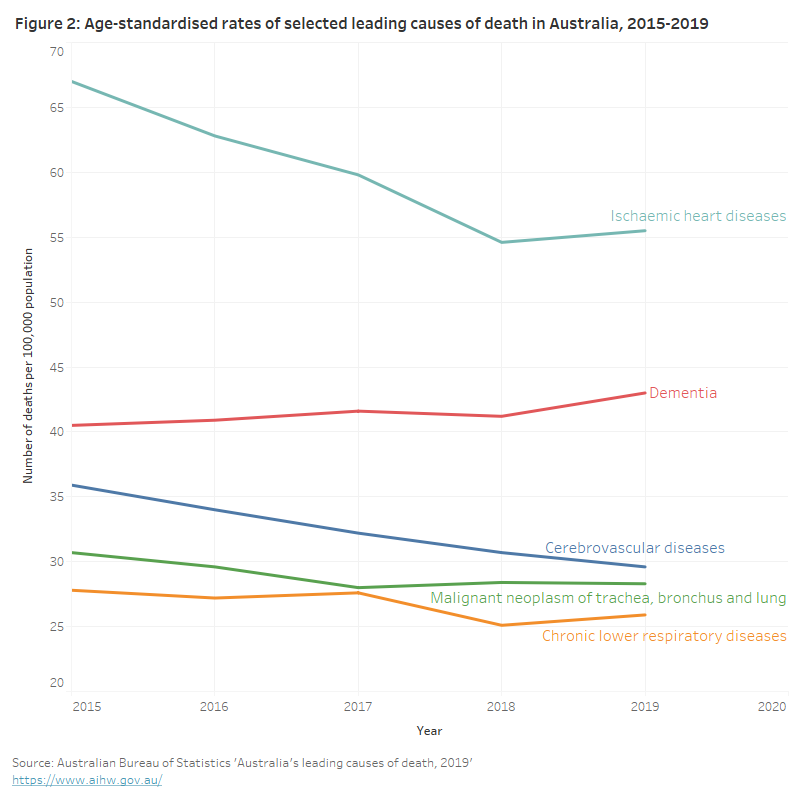
In Australia, the number of people who die due to dementia has been steadily increasing (AIHW 2020a). However, the age-standardised death rates due to dementia over time – which account for population growth and ageing – has remained relatively stable in recent years (between 2015 and 2019). This suggests that the increasing number of deaths due to dementia is mainly due to Australia’s ageing population. In contrast, for other leading causes of death, such as ischaemic heart diseases and cerebrovascular diseases, the rate of deaths has been falling in recent years (see Figure 2).
This line graph shows annual age-standardised rates of leading causes of death in Australia over the period 2015 to 2019. While the rate for dementia remained relatively steady over this period, the rates for ‘ischaemic heart diseases’, ‘cerebrovascular diseases’, ‘malignant neoplasm of trachea, bronchus and lung’, and ‘chronic lower respiratory diseases’, all declined during this period.
Comparisons of the age-standardised rates of death among people with dementia recorded on their death certificate during the first 10 months of 2020 with the average age-standardised rates for the same months in previous years (2015–2019) are used to approximate the short-term effects of the pandemic on dementia mortality. This report does not however aim to estimate excess mortality during the pandemic.
Excess mortality refers to additional deaths that occurred during a given period of time (such as in a pandemic), relative to what would have been expected based on modelling historical deaths data (ABS 2020d). While the development of a model to quantify excess mortality is outside the scope of this report, we can still illustrate the short-term effects of the pandemic by making comparisons between age-standardised rates of deaths.
These comparisons have limitations, particularly for health conditions where rates have increased or decreased over time, and should be interpreted with caution.
More information on excess mortality during the COVID-19 pandemic can be found in the Australian Bureau of Statistics report: Measuring excess mortality in Australia during the COVID-19 pandemic.


