Pharmaceutical Benefits Scheme prescriptions data
About the data source
Data on prescriptions dispensed are sourced from the Pharmaceutical Benefits Scheme (PBS) data collection.
The Commonwealth government subsidises the cost of a wide range of prescription medicines through two separate schemes, the Pharmaceutical Benefits Scheme (PBS), available to current Medicare card holders and other eligible people, and the Repatriation Pharmaceutical Benefits Scheme (RPBS), for eligible war veterans and their dependants.
Most prescriptions for General Schedule medicines are dispensed through community pharmacies, but PBS is also available through private hospitals and eligible public hospitals to patients on discharge and day patients. In addition, a number of drugs are distributed under alternative arrangements when the usual supply through community pharmacies is unsuitable. Examples are the highly specialised drugs program and General Schedule medicines that are supplied directly to Indigenous patients via Aboriginal Health Services in remote areas of Australia (RAAHS program).
PBS data includes all prescriptions dispensed under the PBS and RPBS and processed for subsidy by Services Australia, including prescriptions that were not eligible for subsidy (referred to as ‘under co-payment’ prescriptions). Data excludes some PBS programs where patient-level details are not available, for example the RAAHS program. The PBS data collection accessed for this report is maintained by the Commonwealth Department of Health and Aged Care.
PBS data contains information about the medication supplied and details about the patient, prescriber and supplier of the medication.
The PBS does not cover medicines supplied to public hospital in-patients, over-the-counter medicines or private prescriptions.
Any future reference to PBS data in this document will include both PBS and RPBS prescriptions (PBS accounting for over 95% of the total by volume).
Methodology
PBS data were extracted for the variables shown in Table 8.
Type of information | Data item | Description |
|---|---|---|
PBS prescription | ATC code | ATC code of the PBS item as listed in the Schedule of Pharmaceutical Benefits. |
PBS prescription | Number of prescriptions | The total number of times that a pharmaceutical benefit is supplied to the patient. |
PBS prescription | Date of supply | The date the prescription was supplied to the patient. |
Patient | Patient postcode | Patient’s Medicare enrolment postcode at date of supply. |
ATC = Anatomical Therapeutic Chemical; PBS = Pharmaceutical Benefits Scheme
Data were extracted for categories of medicines associated with treating the following types of health conditions, according to the following broad groupings of Anatomical Therapeutic Chemical (ATC) codes:
- Respiratory – R03, H02AB06/07
- Mental health – N05, N06A/B
- Cardiovascular – C, B01.
See Table 9 for a more detailed breakdown of the codes. For more information on the ATC classification, please see: WHO Collaborating Centre for Drug Statistics.
PBS ATC classification versus WHO classification
There are a small number of cases where the therapeutic use of the drug as listed by the Therapeutic Goods Administration, and hence by PBS, differs from the WHO classification. In these cases the drug may be classified to a different group that more accurately reflects the therapeutic use of the drug in Australia, see: Pharmaceutical Benefits Scheme (PBS) – Body system.
A representation of the items is shown in Figure 8.
The data were aggregated by prescription group, week and SA4.
- Week was based on the date of supply, with weeks (Monday to Sunday) being identified by their start date and forming a continuous time series over the duration of the data set.
- SA4 was derived from the postcode of the patient’s residential address. Postcodes were mapped to SA4 based on an ABS population-based correspondence. Where the area of a postcode crossed more than one SA4 the data were proportionally allocated to SA4 according to the population proportions. Note that for around 85% of the data the postcode was contained wholly within an SA4, requiring no proportional allocation.
Records with missing patient details were excluded from the final data set. These accounted for less than 1% of the selected data.
The constructed data set reports the count of prescriptions dispensed associated with each of these groupings. The crude rate is also reported. Rates were calculated by dividing the count data by the estimate of population for the relevant week and geographical area derived as described in the Population data section.
Broad category | Prescription group | ATC codes | Description |
|---|---|---|---|
Respiratory-related items | Respiratory items | R03 | Drugs for obstructive airway disease |
| Relievers | R03AC02, R03AC03 | R03AC02 – Salbutamol Belonging to a common class of medications (short-acting beta2-agonists (SABA)) dispensed and used to relieve breathlessness and wheeze due to airway narrowing and to prevent exercise-induced airway narrowing in people with asthma. |
| Preventers | R03AK, R03BA, R03DC | R03AK1 – combination medications which include an inhaled corticosteroid and a long-acting beta2 agonist (LABA). R03BA – Inhaled corticosteroids used as a long-term maintenance treatment for asthma to reduce symptoms and prevent exacerbations. R03DC – Leukotriene receptor antagonists (LTRA) are the first-line preventer in the management of asthma in children aged 2–14. They are provided as tablets and may be used as an alternative or adjunct to inhaled corticosteroids. |
| Other (including COPD-specific treatments, other asthma) | Remainder of R03 | For a more detailed description of respiratory medications see: Using PBS and MBS data to report on the treatment and management of chronic respiratory conditions 2016–17 |
| Oral corticosteroids | H02AB06, H02AB07 | Oral corticosteroids are used for short-term treatment of exacerbations of asthma and COPD to reduce the duration and severity of episodes. Note that these medications can also be used for the treatment of other conditions such as arthritis, colitis and allergic/inflammatory conditions. |
Mental health-related items | Mental health items | N05A, N05B, N05C, N06A, N06B | See below |
| Anxiolytics | N05B | N05B – This group comprises preparations used in the treatment of neuroses and psychosomatic disorders associated with anxiety and tension, for example benzodiazepines. |
| Antidepressants | N06A | This group comprises preparations used in the treatment of endogenous and exogenous depressions. The group is subdivided mainly according to mode of action. The various antidepressants have different modes of action, and the classification will not reflect the exact mode of action of the various antidepressants. |
| Other mental health | Residual | N05A – Antipsychotics: this group comprises drugs with antipsychotic actions (that is, neuroleptics). N05C – Hypnotics and sedatives. Hypnotic drugs are used to induce sleep and treat severe insomnia. Sedative drugs are prescribed to reduce excitability or anxiety. NO6B – Psychostimulants, agents used for ADHD and nootropics. Agents used for Attention-Deficit Hyperactivity Disorder (ADHD) and to improve impaired cognitive abilities (nootropics). |
Cardiovascular-related items | Cardiovascular items | B01, C01, C02, C03, C04, C05, C07, C08, C09, C10 | See below. For further details on cardiovascular medicines see Medicines for cardiovascular disease |
| Anti-thrombotic agents | B01 | Antithrombotic medicines prevent blood clots forming or dissolve existing blood clots. These medicines help to reduce the risk of heart attack among people with coronary heart disease and reduce the risk of further strokes among patients with a history of ischaemic stroke. |
| Blood pressure lowering medicines | C03, C07, C08, C09 | C03 – Diuretics These medicines are used to treat high blood pressure. Combinations of blood pressure lowering medicines are often used because this increases their effectiveness and allows lower doses of each drug to be used. |
| Lipid-modifying agents | C10 | Lipid-modifying medicines control blood cholesterol levels. They are effective in preventing heart attacks and reducing coronary heart disease deaths |
| Other cardiovascular medicines | C01, C02, C04, C05 | C01 – Cardiac therapy: is a therapeutic subgroup of the ATC classification system. The subgroup includes cardiac glycosides, antiarrhythmics and cardiac stimulants, which are used to regulate the rhythms of the heart. They may also be used to treat angina and heart failure. The subgroup also includes vasodilators, which open the main blood vessels of the body, as well as other cardiac preparations used in treating coronary heart disease C02 – Antihypertensives2 suppress signals to the heart that make it beat harder, or open and relax peripheral arteries. These have largely been replaced by newer medicines to control blood pressure. C04 – Peripheral vasodilators: open blood vessels in outer parts of the body, such as the arms and legs, making it easier for the heart to pump blood and lowering blood pressure. Overall, these make up a very small proportion of cardiovascular-related prescriptions. C05 – Vasoprotectives: act to relieve certain conditions of the blood vessels such as haemorrhoids and varicose veins. Overall, these make up a very small proportion of cardiovascular-related prescriptions. |
Notes
- Single Maintenance and Reliever Therapy involves the use of inhaled corticosteroid and a long-acting beta-2 agonist combination inhaler (budesonide/formoterol) for both maintenance and as a reliever.
- Antihypertensives can also be considered blood pressure lowering medications, though they have largely been replaced by newer medicines.
Figure 8: Representation of relationship between item groupings in Pharmaceutical Benefits Scheme data
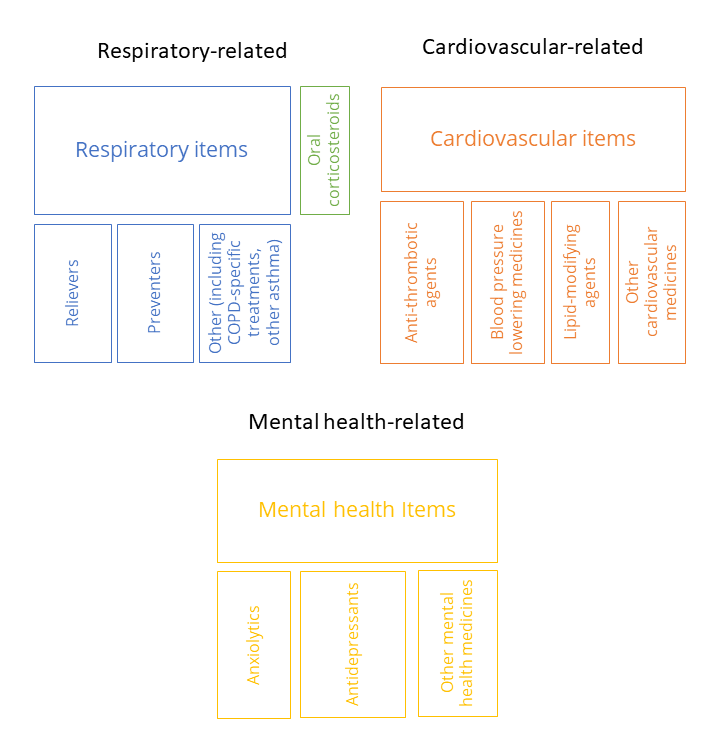 Note: The size of the boxes does not indicate the volume of medicines dispensed.
Note: The size of the boxes does not indicate the volume of medicines dispensed.
Reporting of results
In line with AIHW Policy on reporting to manage confidentiality as well as data management protocols for this data set, some data have been suppressed. In particular, where prescription counts on a given week in a given SA4 for a given groups of drugs were less than 6, the data were not reported. Secondary suppression was also applied throughout in the event that a suppressed cell could be identified from a higher-level aggregation.
Data considerations and limitations
Association with health conditions
PBS data do not generally include the reason a medicine has been prescribed. However, the restriction requirements of a drug as listed in the Schedule of Pharmaceutical Benefits can give some information about the reasons for prescribing, depending on the level of authority required. For more details about Authority requirements see PBS for prescribers – Services Australia.
Scope
Data are based on prescriptions that were dispensed.
Specifications of geolocation
The geolocation of the data is based on patients’ Medicare enrolment address, and not the place the prescription was dispensed. The patient’s address may differ from the location of the patient at the time of condition onset, and any exposure to an environmental influence.
Quality of geolocation data
All the data in this release are presented according to a common geographical structure – 2016 ASGS SA4. However, in the source PBS data, geographical area is identified by the patients’ Medicare enrolment address postcode. A single mapping file from 2016 is used to map from postcodes to 2016 ASGS SA4s, based on the distribution of the population within the postcode in 2016, and the intersection of its boundaries with the boundaries of the SA4.
In this context, quality of the data is not affected where postcodes completely fall within a single SA4. However, quality will be affected for postcodes which are divided across SA4s, and for which the geographical distribution of the population has changed over time.
Seasonality
Data for this report were based on the date a prescription was supplied. When comparing data over time, the impact of public holidays on the volume of prescriptions dispensed should be considered. Other examples of potential seasonal effects include the influence of the timing and severity of the annual ‘flu season’ on respiratory medications.
Also see the PBS safety net scheme section.
Respiratory medications
- Note that asthma reliever medication salbutamol inhalers (R03AC02) and terbutaline (R03AC03) inhalers can be purchased over the counter at a pharmacy without a prescription. These sales are not included in PBS data.
- The Single Maintenance and Reliever Therapy (SMART) regimen is the use of budesonide/eformoterol combined (Symbicort) as a single inhaler for both preventer and reliever therapy. Only certain form and strengths of budesonide/eformoterol are eligible for SMART therapy. These Item codes amount to 50% of use by volume. Given that only 50% of the scripts for this drug qualify for SMART therapy, and it is impossible to tease out how much of that 50% may be for reliever use rather than preventer, it was decided to categorise this drug as preventer only.
- Oral corticosteroids may also be used to treat conditions other than respiratory related conditions.
For specific notes and known issues relating to the data, see Table 10.
PBS under co-payment prescriptions
On 1 April 2012, the PBS data collection expanded in scope to include under co-payment prescription data. Prior to April 2012, PBS prescription data were only collected for subsidised prescriptions.
Under the PBS the cost of most prescription medicines is subsidised by the Commonwealth government. Patients are required to pay a co-payment towards the cost of their prescription with the government paying the remaining cost. To determine the amount of co-payment, patients are classified as either general (Medicare card) or concessional (Medicare card + concessional card). At 1 January 2022 the maximum co-payment fee was set at $42.50 for general and $6.80 for concessional patients. For current and historical co-payment amounts, see Pharmaceutical Benefits Scheme (PBS) | Fees & Patient Contributions.
A PBS prescription is classified as under co-payment when the dispensed price of the prescription does not exceed the patient co-payment, and the patient pays the full cost of the medication.
As a consequence of the PBS pricing structure, under co-payment prescriptions are predominantly dispensed to general non-safety net patients. The maximum co-payment for general patients was $36.10 in 2013, increasing to $42.50 in 2022.
For calendar year 2013, the first full year that under co-payment data was collected, under co-payment data accounted for around 24% of PBS prescriptions (67 million / 283 million). By 2022 this had increased to 32% (105 million/330 million).
PBS safety net scheme
The PBS safety Net scheme is designed to protect patients and their families requiring a large number of PBS or RPBS prescriptions. The safety net scheme operates over a calendar year. When eligible patient contributions of patients and families reach their safety net threshold the co-payment is reduced for the remainder of the year, with the general co-payment reduced to the concessional rate, and the concessional co-payment reduced to zero.
Safety Net entitlements can act as an incentive for repeat prescriptions to be used to obtain medicines earlier than they are needed, historically resulting in an artificial increase in prescription volume in November/December, with a consequent decrease in the early months of the following year.
This pattern has been reduced to some degree by the introduction of the following legislation:
- 1 January 2006 – the safety net 20-day rule.
For certain PBS medicines a repeat supply of the same medicine within 20 days will fall outside the Safety Net, that is, the cost will not count towards a person’s Safety Net threshold or if the Safety Net threshold has been reached, the charge will be the usual PBS contribution, not the reduced Safety Net amount.
- 1 January 2016 – the safety net early supply rule.
Expanded PBS early supply rule provisions replaced the Safety Net 20-day rule and extended early supply rules to apply to more medicines.
COVID-19 impact in 2020
In March 2020, there was an increase of 23.1% in the total number of PBS scripts dispensed for the month compared to March 2019, followed by a decrease in April. This spike was most significant for the respiratory group of medicines. In response to the increase, steps were taken to limit the over-buying of medicines (Therapeutic Goods Administration 2020).
Category | Sub-category | ATC codes | Under co-payment notes – comparison between 2011–12 and 2012–13 | Dominant drug notes |
|---|---|---|---|---|
Respiratory | Reliever | R03AC02 | There is an increase in script volumes from 2012–13 with the introduction of the under co-payment data collection, script volumes increasing by 17% in 2012–13 compared with previous year. |
|
Respiratory | Preventer (includes combinations) | R03BA (preventer + combinations less biologics) | No change, with drugs priced above the co-payment. |
|
Respiratory | Other – mainly COPD | Remainder of R03 | No change in 2012–13, with drugs priced above the co-payment. | The dominant drug has been Tiotropium (COPD), ranging from 75% of scripts for the group (up to 2013–14) and reducing to 40% in 2021–22, with new combination drugs being introduced in recent years, for example, FLUTICASONE FUROATE + UMECLIDINIUM + VILANTEROL (18% in 2021–22) |
Respiratory | Oral corticosteroids | H02AB06 | There is a significant increase in script volumes from 2012–13 with the introduction of the under co-payment data collection, script volumes increasing by 50% in 2012–13. | Prednisolone tablets have consistently accounted for over 60% of scripts over the whole period. |
Mental Health | Anxiolytics | N05B |
| There are two dominant drugs, accounting for 97% of the group in 2021–22:
|
Mental Health | Antidepressants | N06A |
| Usage is spread across a number of drugs:
|
Mental Health | Other | N05A, N05C, N06B |
|
|
Cardiovascular | Anti-thrombotic agents | B01 |
|
|
Cardiovascular | Blood pressure lowering medicines | C03, C07, C08, C09 |
| Usage is spread across many drugs in this group.
|
Cardiovascular | Lipid-modifying medicines | C10 |
| The dominant drugs in this group are the statins (atorvastatin, rosuvastatin, simvastatin), accounting for 80% of the script volume in all years. |
Cardiovascular | Other | C01, C02, C04, C05 |
| Usage is spread across a number of drugs in this group:
|
ATC = Anatomical Therapeutic Chemical
References
Therapeutic Goods Administration (2020) Coronavirus (COVID-19): Information on medicines and medical devices, Therapeutic Goods Administration website, accessed 13 December 2023.


