Clients with problematic drug and/or alcohol use
There is a strong association between problematic alcohol or other drug use and experiences of homelessness (AIHW 2019). Problematic drug and/or alcohol use can be a pathway into homelessness or develop while experiencing homelessness (Robinson 2014; Johnson & Chamberlain 2008). It can lock people into homelessness and compound the effects of limited service engagement and increased social isolation. The Journeys Home project identified that people were more likely to have risky levels of alcohol and drug use, the longer they were homeless (Scutella et al. 2014).
Problematic drug and/or alcohol users are at great risk of serious and preventable health issues and death, particularly those who are homeless (AIHW 2019). They are also likely to have the most persistent and challenging problems (Johnson & Chamberlain 2008; Scutella et al. 2014).
Key findings
- In 2018–19, 1 in 10 SHS clients (10%, or almost 28,000 people aged 10 and over) were identified as having problematic drug and/or alcohol use.
- Most clients with problematic drug and/or alcohol use were known to be homeless upon presentation (55%) compared with 42% of all SHS clients.
- Clients with problematic drug and/or alcohol use received more frequent support (2.9 support periods per client) over a longer period (median support length 87 days) than other client groups.
- Almost 3 in 4 (74%) clients with problematic drug and/or alcohol use had received assistance from a SHS agency at some point since the collection began in 2011–12, with the other 26% deemed to be new clients.
- Clients with problematic drug and/or alcohol use remain one of the least likely of all SHS client groups to meet all case management goals (15%).
- At the end of support in 2018–19, almost half (46%) of clients with problematic drug and/or alcohol use were known to be experiencing homelessness, which was higher than for all other client groups.
Reporting clients with problematic drug and/or alcohol use in the Specialist Homelessness Services Collection (SHSC)
SHS clients aged 10 and over are reported in the SHSC with problematic drug and/or alcohol use if, at the beginning of or during support, the client provided any of the following information:
- recorded their dwelling type as rehabilitation facility
- required drug or alcohol counselling
- were formally referred to the SHS service from an alcohol and drug treatment service
- had been in a rehabilitation facility or institution during the past 12 months
- reported problematic drug, substance or alcohol use as a reason for seeking assistance or the main reason for seeking assistance.
The identification of clients with problematic drug and/or alcohol use may be current or recent; referring to issues at presentation, just prior to receiving support or at least once in the 12 months prior to support.
For more information see Technical notes.
Client characteristics
In 2018–19 (Table SUB.1):
- SHS agencies assisted almost 28,000 clients (aged 10 and over) with problematic drug and/or alcohol use an increase from around 24,300 in 2014–15.
- Clients with problematic drug and/or alcohol use represented 10% of all SHS clients, with little change in the proportion of clients since 2014–15.
|
|
2014–15 |
2015–16 |
2016–17 |
2017–18 | 2018–19 |
|---|---|---|---|---|---|
|
Number of clients |
24,251 |
26,562 |
27,229 |
27,158 | 27,974 |
|
Proportion of all clients |
9 |
10 |
9 |
9 | 10 |
|
Rate (per 10,000 population) |
10.3 |
11.2 |
11.3 |
11.0 | 11.2 |
|
Housing situation at the beginning of the first support period (proportion (per cent) of all clients) |
|||||
|
Homeless |
59 |
58 |
57 |
56 | 55 |
|
At risk of homelessness |
41 |
42 |
43 |
44 | 45 |
|
Length of support (median number of days) |
74 |
77 |
83 |
86 | 87 |
|
Average number of support periods per client |
2.7 |
2.9 |
2.9 |
3.0 | 2.9 |
|
Proportion receiving accommodation |
53 |
51 |
49 |
50 | 50 |
|
Median number of nights accommodated |
39 |
37 |
40 |
40 | 35 |
|
Proportion of a client group with a case management plan |
74 |
74 |
75 |
75 | 73 |
|
Achievement of all case management goals (per cent) |
16 |
13 |
13 |
14 | 15 |
Notes:
- Rates are crude rates based on the Australian estimated resident population (ERP) at 30 June of the reference year. Minor adjustments in rates may occur between publications reflecting revision of the estimated resident population by the Australian Bureau of Statistics.
- The denominator for the proportion receiving accommodation is all SHS clients who have problematic drug and/or alcohol use. Denominator values for proportions are provided in the relevant supplementary table.
- The denominator for the proportion achieving all case management goals is the number of client groups with a case management plan. Denominator values for proportions are provided in the relevant supplementary table.
- Data for 2014–15 to 2016–17 have been adjusted for non-response. Due to improvements in the rates of agency participation and SLK validity, data from 2017–18 are not weighted. The removal of weighting does not constitute a break in time series and weighted data from 2014–15 to 2016–17 are comparable with unweighted data for 2017–18 onwards. For further information, please refer to the Technical Notes.
Source: Specialist Homelessness Services Collection 2014–15 to 2018–19.
Age and sex
In 2018–19, of clients with problematic drug and/or alcohol use (Supplementary table SUB.1):
- More than half (54% or more than 15,000 clients) were male which differed to the overall SHS client profile which was mostly female (60%).
- Clients with problematic drug and/or alcohol use had a younger age profile than other SHS client groups with around 8 in 10 (79%) clients aged under 44 years; 27% were aged 10–24 years, 25% aged 25–34 and 26% aged 35–44. This is even notwithstanding clients under the age of 10 not included.
- Male clients had an older age profile than females, with 53% of males aged 35 and over compared with 42% of females.
Indigenous status
- In 2018–19, around 8,000 clients with problematic drug and/or alcohol use identified as Indigenous (Supplementary table SUB.8). This equates to 3 in 10 clients (29%) with problematic drug and/or alcohol use whose Indigenous status was known.
- Indigenous clients with problematic drug and/or alcohol use represent 12% of all Indigenous SHS clients (Supplementary table INDIGENOUS.1).
Indigenous clients with problematic drug and/or alcohol use had a younger age profile than non-Indigenous clients with problematic drug and/or alcohol use. That is:
- 30% of Indigenous clients with problematic drug and/or alcohol use were aged 10–24 compared with 26% of non-Indigenous clients, and
- 19% of Indigenous clients with problematic drug and/or alcohol use were aged 45 and over compared with 22% of non-Indigenous SHS clients.
States and territory and remoteness
In 2018–19:
- The highest number of SHS clients with problematic drug and/or alcohol use were reported accessing services in Victoria (more than 9,600 clients or 34% of national total) and New South Wales (8,300 or 30%) (Supplementary table SUB.2).
- There were higher rates of clients with problematic drug and/or alcohol use in the Northern Territory (39 per 10,000 population) and Tasmania (17 per 10,000 population). Queensland had the lowest rate, at 8 clients per 10,000 population.
- Services in the Australian Capital Territory and Tasmania had the highest proportion of SHS clients with problematic drug and/or alcohol use (13% each). Victoria (9%) had the lowest proportion of all their SHS clients reporting problematic drug and/or alcohol use (Supplementary table SUB.2 and CLIENTS.1).
- SHS agencies in the Northern Territory (61% females, 39% males) and Western Australia (59% females, 41% males) had higher proportions of female clients with problematic drug and/or alcohol use, while Tasmania had mostly males (61% males, 39% females).
- SHS clients with problematic drug and/or alcohol use primarily accessed services in Major cities (64%) and Inner regional areas (22%) (Supplementary table SUB.10).
Living arrangements
The types of living arrangements reported by SHS clients with problematic drug and/or alcohol use at the beginning of support were quite different from the overall SHS population and other client groups. In 2018–19 (Supplementary tables SUB.9 and CLIENTS.7):
- Almost 6 in 10 (59% or more than 15,900) clients with problematic drug and/or alcohol use were living alone at the beginning of SHS support. This is a higher proportion than for all SHS clients (30%) and other client groups, such as clients with a current mental health issue (46%) and clients with disability (37%).
- Comparatively fewer clients with problematic drug and/or alcohol use were living as one parent with child(ren) (13% or 3,500 compared with 36% of total SHS clients), or in a group (10% or 2,700 clients compared with 6% of total SHS clients).
Selected vulnerabilities
Most clients with problematic drug and/or alcohol use face additional challenges which may make them more vulnerable to homelessness. The selected additional vulnerabilities presented here include family and domestic violence and/or a current mental health issue.
In 2018–19 (Table SUB.2):
- More than 2 in 5 (43% or almost 12,000) clients with problematic drug and/or alcohol use also reported a current mental health issue.
- Almost 8,400 (30%) clients with problematic drug and/or alcohol use also reported a current mental health issue and family and domestic violence.
- Less than 1 in 10 (9% or 2,500) clients with problematic drug and/or alcohol use also reported family and domestic violence.
- Less than 1 in 5 (19% or 5,200) clients only reported problematic drug and/or alcohol use.
|
Family and domestic violence |
Mental health issue |
Problematic drug |
Clients |
Per cent |
|---|---|---|---|---|
|
Yes |
Yes |
Yes |
8,351 |
29.9 |
|
Yes |
No |
Yes |
2,455 |
8.8 |
|
No |
Yes |
Yes |
11,951 |
42.7 |
|
No |
No |
Yes |
5,217 |
18.6 |
|
|
|
|
27,974 |
100.0 |
Notes:
- Clients are assigned to one category only based on their vulnerability profile.
- Clients are aged 10 and over.
- Totals may not sum due to rounding.
Source: Specialist Homelessness Services Collection 2018–19.
Service use patterns
Clients with problematic drug and/or alcohol use (see Tables SUB.1, DIS.1 and MH.1) received:
- a higher median number of days of support (87 days), compared with clients with disability (80 days) and clients with a current mental health issue (75 days)
- a higher average number of support periods per client (2.9), compared with clients with disability and clients with a current mental health issue (2.4 support periods each)
- a lower median number of nights of accommodation (35) compared with clients with disability and current mental health issues (39 nights each).
New or returning clients
In 2018–19 (Supplementary table SUB 7):
- Clients with problematic drug and/or alcohol use were more likely to have received SHS services in the past (74% or more than 20,800 clients) than be new clients (26% or more than 7,100). That is, more clients had previously been assisted by an SHS agency at some point since the collection began in 2011–12.
- Compared with 2017–18, there was an increase in the number of returning clients (an increase of 1,100 clients, or 2 percentage points).
- Clients with problematic drug and/or alcohol use were also more likely to be returning (74%), compared with other client groups, for example 66% of clients with a mental health issue and 62% of those with profound or severe disability. This may reflect the cyclic nature of homelessness for people with problematic drug and/or alcohol use.
Main reasons for seeking assistance
In 2018–19, the main reasons clients with problematic drug and/or alcohol use presented to SHS agencies were:
- housing crisis (21%, compared with 20% of the overall SHS population)
- family and domestic violence (13%, compared with 28%)
- inadequate/inappropriate dwelling conditions (13%, compared with 10%) (Supplementary tables SUB.5 and CLIENTS.16).
Few clients (6%) with problematic drug and/or alcohol use reported their substance use as the main reason for seeking SHS assistance.
Services needed and provided
In 2018–19, the top 6 needs reported by SHS clients with problematic drug and/or alcohol use mainly related to housing and tenure (Figure SUB.1). Key features include:
- Short-term or emergency accommodation was the most needed service or assistance type (61% or more than 16,900 clients) and it was provided to 67% of these clients. A higher proportion of clients in this group needed this type of short-term housing compared with other groups, such as those with mental health issues (48%) and those with disability (45%).
- Long-term housing (54% or around 15,100 clients) was also commonly needed, but was one of the services that was least able to be provided (5% of these clients).
- Material aid/brokerage was needed by around half of clients (51% or almost 14,300 clients), with assistance provided to the majority (89%) of these clients.
- Unlike other client groups, transport (41%) was one of the top 6 needs, and it was provided to 93% of these clients.
In 2018–19, more than one-third (35% or almost 9,800 clients) of clients with problematic drug and/or alcohol use identified a need for drug or alcohol based services (Figure SUB.1):
- almost half (45% or 4,400 clients) had their request met
- 2,000 clients (20%) were referred to another agency
- 3,400 clients (35%) had unmet needs for drug or alcohol based services (neither provided nor referred).
Figure SUB.1: Clients with problematic drug or alcohol issues, by most needed services and service provision status (top 6), 2018–19
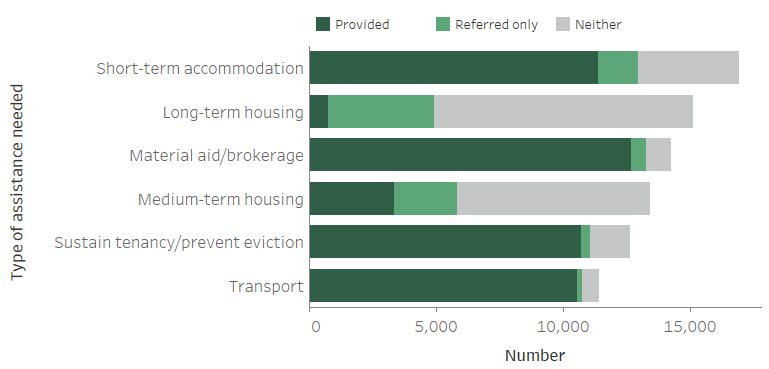
Notes:
- Excludes ‘Other basic assistance’, ‘Advice/information’ and ‘Advocacy/liaison on behalf of client’.
- 'Short-term accommodation' includes temporary and emergency accommodation and sustain tenancy/prevent eviction includes assistance to sustain tenancy or prevent tenancy failure or eviction.
- 'Neither' indicates a service was neither provided nor referred.
Source: Specialist Homelessness Services Collection 2018–19, Supplementary table SUB.3.
The proportion of SHS clients with problematic drug and/or alcohol use with a case management plan has remained comparatively high over time (73% in 2018–19); however, those achieving all case management goals has remained low (15% in 2018–19). This group remains one of the least likely of all SHS client groups to meet all goals.
Outcomes at the end of support
Outcomes presented here highlight the changes in clients’ housing situation between the start and end of support. Data is limited to clients who ceased receiving support during the financial year—meaning that their support periods had closed and they did not have ongoing support at the end of the 2018–19 reporting period.
Many clients had long periods of support or even multiple support periods during 2018–19. They may have had a number of changes in their housing situation over the course of their support. These changes within the year are not reflected in the data presented here, rather the client situation at the start of their first period of support during 2018–19 is compared with the end of their last period of support in 2018–19. A proportion of these clients may have sought assistance prior to 2018–19, and may again in the future.
In 2018–19 (Table SUB.3):
- Over half of clients with problematic drug and/or alcohol use began support known to be experiencing homelessness (56% or 9,800 clients); decreasing by 2,300 to 7,600 clients (46%) by the end of support. Compared with all other client groups, these clients were most likely to start and end support known to be experiencing homelessness.
- Much of the decrease in numbers of clients known to be experiencing homelessness can be attributed to the drop in clients sleeping rough (no shelter or improvised/inadequate dwellings); from 3,300 clients at the start to 1,800 at the end of support.
- One of the greatest changes in housing situation from the start to the end of SHS support was for those living in public or community housing; a 9 percentage point increase from around 12% to 20%.
While overall housing outcome figures generally reflect trends towards more favourable housing, experiences of homelessness, particularly rough sleeping, appear to be more common for clients with problematic drug and/or alcohol use both at the start and end of SHS support.
|
Housing situation |
Beginning of support |
End of |
Beginning of support |
End of |
|---|---|---|---|---|
|
No shelter or improvised/inadequate dwelling
|
3,315 | 1,848 | 18.8 | 11.2 |
| Short term temporary accommodation | 3,323 | 3,484 | 18.9 | 21.1 |
|
House, townhouse or flat - couch surfer or with no tenure |
3,189 |
2,228 |
18.1 |
13.5 |
| Total homeless | 9,827 | 7,560 | 55.8 | 45.9 |
|
Public or community housing - renter or rent free |
2,025 |
3,307 |
11.5 |
20.1 |
|
Private or other housing - renter, rent free or owner |
3,054 |
3,720 |
17.4 |
22.6 |
|
Institutional settings |
2,693 |
1,886 |
15.3 |
11.4 |
|
Total at risk |
7,772 |
8,913 |
44.2 |
54.1 |
| Total clients with known housing situation | 17,599 | 16,473 | 100.0 | 100.0 |
| Not stated/other | 1,518 | 2,644 | ||
|
Total clients |
19,117 |
19,117 |
|
|
Notes:
- Percentages have been calculated using total number of clients as the denominator (less not stated/other).
- It is important to note that individual clients beginning support in one housing type need not necessarily be the same individuals ending support in that housing type.
- Not stated/other includes those clients whose housing situation at either the beginning or end of support was unknown.
Source: Specialist Homelessness Services Collection. Supplementary table SUB.4.
Housing outcomes for homeless versus at risk clients
For clients with a known housing status who were at risk of homelessness at the start of support (almost 7,100 clients), by the end of support (Interactive Tableau visualisation):
- Almost 1 in 3 (2,200 clients or 31%) were in private housing.
- Around 1,900 clients (27%) were in public or community housing.
A smaller number were experiencing homelessness at the end of support (around 1,600 clients or 23% of those who started support at risk).
For clients who were known to be homeless at the start of support (just over 8,500 clients), agencies were able to assist:
- 2,400 clients (28%) into short term accommodation
- 1,400 (16%) into private housing.
A further 1,600 clients (19%) were couch surfing at the end of support and 1,500 clients (17%) were rough sleeping at the end of support.
The characteristics of people with problematic drug and/or alcohol use as well as their service use patterns and housing outcomes were different from the other client groups presented in this report. Clients with problematic drug and/or alcohol use were more likely to be male, present to agencies alone and be homeless at first presentation compared with overall SHS clients. They were also more likely to be returning clients and use support services to a greater extent.
AIHW (Australian Institute of Health and Welfare) 2019. Alcohol, tobacco & other drugs in Australia. AIHW Cat. no: PHE 221. Canberra: AIHW. Viewed 26 September 2019.
Kaleveld L, Seivwright A, Box E, Callis Z & Flatau P 2018. Homelessness in Western Australia: A review of the research and statistical evidence. Perth: Government of Western Australia, Department of Communities. Viewed 27/06/2019
Johnson C & Chamberlain G 2008. Homelessness and substance abuse: which comes first? Australian Social Work, 61(4) Viewed 1 February 2018.
Robinson C 2014. Trauma: A cause and consequence of homelessness. In: Chamberlain C, Johnson G, Robinson C (eds.) Homelessness in Australia. Sydney, NSW: NewSouth Publishing.
Scutella R, Chigavazira A, Killackey E, Herault N, Johnson G, Moshcion J & Wooden M 2014. Journeys Home Research Report No. 4 Findings from Waves 1 to 4: Special Topics. University of Melbourne.


