How do Australia's males access health care?
Page highlights
Australian males claimed more than 218 million services through Medicare, which equates to an average of 17 Medicare services per person, in 2020–21.
Males had a lower participation rate for bowel cancer screening than females (39% compared with 43%) across the 50–74 target age range, in 2020–21.
- Almost 8 in 10 (79%) Australian males aged 15 and over visited a GP in the previous 12 months.
- 21% of males aged 15 and over who needed to and saw a GP, waited longer than they felt acceptable to get an appointment with a GP, in 2020–21.
58% of Australian males had some form of private health insurance, in 2020–21.
There were 4.3 million emergency department presentations among males, with rates of presentations highest in those aged 85 and over, in 2020–21.
The Australian health system provides a wide range of preventive, treatment and palliative health care services. Monitoring people’s health needs, their help-seeking behaviours, and their patterns of health service use helps governments and health service providers to identify inequalities in access and predict future health care needs.
The Medicare Benefits Schedule (MBS) is a listing of the Medicare services subsidised by the Australian Government. Claims data comprise information on services that qualify for a Medicare Benefit, for which a claim has been processed (including bulk billed services). In 2021–22, Australian males (of all ages) claimed more than 218 million services through Medicare, an increase from 178 million services in 2018–19. This equates to an average of 17 Medicare services per person in that year (SA 2022).
Australian males (of all ages) claimed more than 41 million GP services in 2021–22 (SA 2022). This equates to an average of 3.3 GP services per person in that year. In comparison, females (of all ages) claimed an average of 4.1 GP services per person.
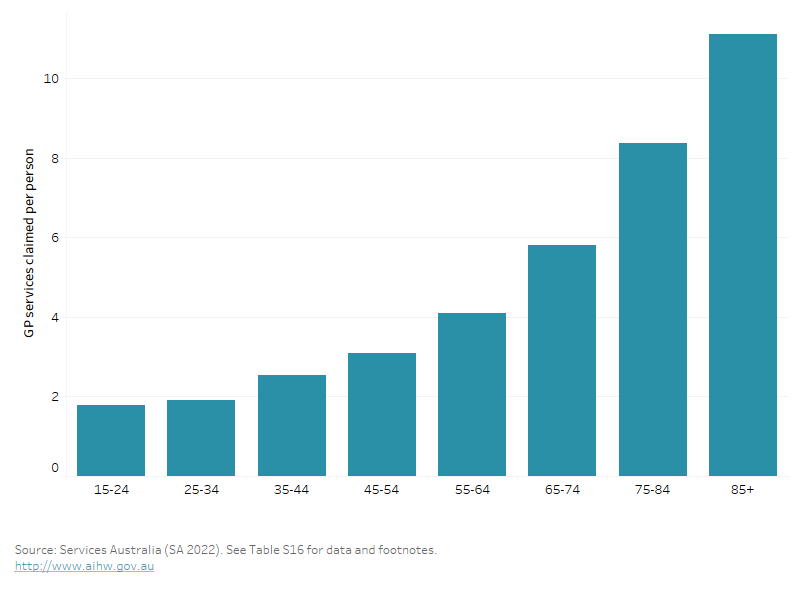
The average number of GP services claimed by males varies by age group (Figure 23). In 2021–22 (SA 2022):
- males aged under 45 claimed 2.2 services per person on average
- males aged 75 and over claimed 9.0 services per person on average.
Figure 23: Average number of GP services per person, claimed through Medicare, by age group, males, 2021–22
Figure 23: Average number of GP services per person claimed through Medicare, by age group, males, 2021
This bar chart shows the number of GP services claimed across age groups, with the number of services claimed increasing with age, peaking in the oldest age group of 85+.
Cancer screening
Population-based cancer screening involves testing for signs of cancer or conditions that cause cancer before a person has symptoms. Early detection of cancer allows for early intervention, which can improve outcomes.
Preliminary data show that in 2020–21 males had a lower participation rate for bowel cancer screening than females (39% compared with 43%) across the 50–74 target age range. Participation increased across male age groups from 30% in the 50–54 years group to 52% in the 70–74 group (AIHW 2023b).
Australia does not have a population-based program for prostate cancer. This is because, unlike for cancers of the bowel, breast or cervix, there is insufficient evidence to support the benefits of population-based screening for prostate cancer with the prostate specific antigen (PSA) test, and that potential harm may outweigh the benefit (DoHAC 2014). However, men have the option to be tested if they are at higher risk due to family history of prostate cancer, symptoms, or being aged 50–69.
For more information see Cancer screening and Prostate cancer screening.
In Australia, primary health care is usually a person’s first encounter with the health system when they have a health concern. Primary health care broadly encompasses health care that is not related to a hospital visit.
Around 79% of males aged 15 and over visited their general practitioner (GP) in the last 12 months in 2021–22. The proportion increased as age increased with 62% of males aged 15–24 compared to 95% of males aged 65 and over having seen a GP in the last 12 months (ABS 2021c).
Barriers to accessing health services may impede the best possible health outcomes for males. In 2020–21, among males aged 15 and over (ABS 2021d):
- 21% waited longer than they felt acceptable to get an appointment with a GP
- 2.7% delayed seeing or did not see a GP when needed because of cost
- 4.9% delayed getting, or did not get, prescribed medication because of cost.
Among males aged 15 and over:
- 12% needed to and saw a mental health professional, in 2021–22 (ABS 2022o)
- 1.5% reported that they saw another mental health professional other than their GP, psychologist or psychiatrist (such as mental health nurse, social worker, counsellor or occupational therapist), in 2021–22 (ABS 2022o)
- 12% of males discussed the issue of reaching a healthy weight with their GP, and this was most discussed in the 45–54 age group (19%) (ABS 2022c)
- 43% reported visiting a dentist at least once in the past 12 months, while 27% reported their last visit was more than 2 years ago (ABS 2022c).
For more information see: Primary health care.
In Australia, private health insurance is available for those wanting to fully or partly cover the costs of being admitted to hospital as a private patient and/or the costs of other ancillary health services.
Based on the 2021–22 ABS Patient Experience Survey, 58% Australian males had some form of private health insurance (ABS 2022m):
- 48% had both hospital and extras cover
- 6% had hospital cover only
- 4% had extras cover only
- 42% had no private health insurance.
Hospital care
Emergency department care
Hospital emergency departments provide care for patients who present for urgent medical attention.
In 2021–22, there were 4.3 million emergency department presentations among all Australian males, accounting for 49% of all presentations with rates of emergency department presentations highest in those aged 85 and over (AIHW 2021e).
For males aged 15 and over, one of the most common reasons for emergency care is ‘Injury and poisoning’. For those aged 45–64 and 65+, ‘Musculoskeletal system diseases’ and ‘Circulatory system diseases’ were among the top reasons, respectively (AIHW 2022b).
For more information see Emergency department care
Admitted patient care
Admitted patient care refers to care provided by public and private hospitals to admitted patients. A hospitalisation is an episode of hospital care that starts with the formal admission process and ends with the formal separation process.
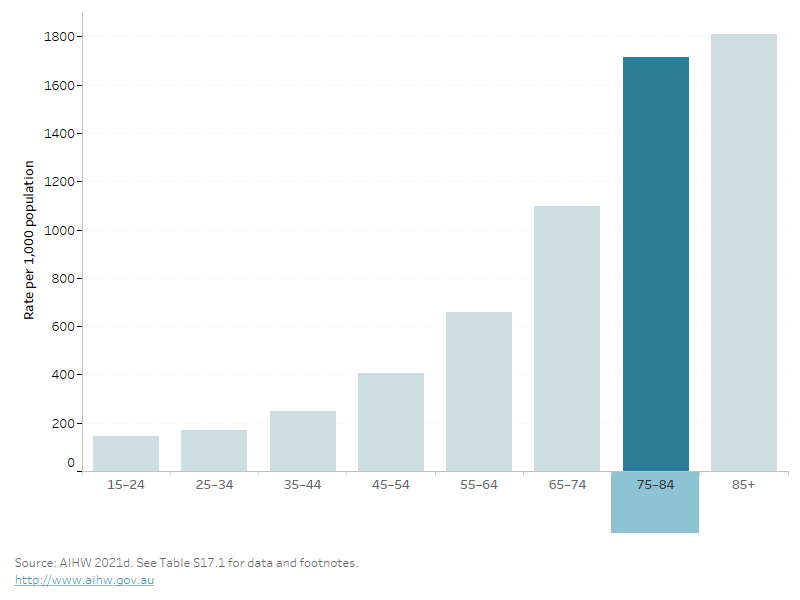
In 2020–21, there were 5.6 million hospitalisations among Australian males, accounting for 48% of all hospitalisations. Hospitalisation rates generally increase with age, and are highest in males aged 85 and over (Figure 24) (AIHW 2021d).
The reasons for hospitalisation vary by age as males experience different health issues over life stages. For males aged under 5, the top reasons were ‘Perinatal period conditions’ and ‘Respiratory system diseases’. For those aged 5–14 and 15–24, the top two reasons were ‘Injury and poisoning’ and ‘Digestive system diseases’, while the third most common reason differed between these two age groups – ‘Respiratory system diseases’ for those aged 5–14 and ‘Mental and behavioural disorders’ for those aged 15–24. For males aged 25–64, ‘Digestive system diseases’ and ‘Injury and poisoning’ continued to be one of the top 3 reasons, while in those aged over 65 ‘Neoplasms’ and ‘Circulatory system diseases’ become the most common reasons for hospitalisation (AIHW 2022b).
Figure 24: Hospitalisations per 1,000 population by age group, males, 2020–21
This bar chart shows the rate of hospital admissions across age groups, with the rate of hospitalisations increasing with age.
For more information see Admitted patient care.
ABS (2021c) Patient Experiences in Australia: Summary of Findings, [Table 2.3: Experience of GP services], abs.gov.au, accessed 17 May 2023.
ABS (2021d) Patient Experiences in Australia: Summary of Findings, [Table 5.3: experience of GP services], abs.gov.au, accessed 17 May 2022.
ABS (2022c) Health Conditions Prevalence: Health service usage and type of health professional consulted by age, [Table 15.3: experience of GP services], abs.gov.au, accessed 10 March 2023.
ABS (2022m) Patient Experiences, [Table 2.3: Private health insurance], abs.gov.au, accessed 17 May 2022.
ABS (2022o) Patient Experiences, 2021-22, [Table 27.3: Experience of mental health services], abs.gov.au, accessed 17 May 2022.
AIHW (2021c) Hospitals: Admitted patients, AIHW website, accessed 27 October 2022.
AIHW (2021d) Hospitals: Admitted patients, [Table 3.8: Admitted Patient care 2020-21, Who used admitted patient services?], AIHW website, accessed 27 October 2022.
AIHW (2021e) Hospitals: Emergency department care 2021–22 [Table 3.1: Emergency department presentations by age and sex], AIHW website, accessed 17 December 2022.
AIHW (2022b) Australia's hospitals at a glance, Hospital activity, AIHW website, accessed 10 March 2023.
AIHW (2023b) Cancer screening programs: quarterly data, AIHW website, accessed 7 October 2022.
DoHAC (2014) Prostate cancer screening – position statement, health.gov.au, accessed 30 January 2023.
SA (Services Australia) (2022) Microdata: Medicare, 2021–22, detailed microdata. Findings based on AIHW analysis of Services Australia microdata.


