Module 3: Access to health care services
Overall, Aboriginal and Torres Strait Islander people experience poorer health than non-Indigenous Australians, but they do not always have the same level of access to health services. This module includes some selected measures of access to health care services that cover the different levels of the health system. The measures compare use of various services for Indigenous and non-Indigenous Australians as a way of broadly monitoring disparities in access. Disparities in access and use of health services may indicate problems with the cultural safety of services, but there may be many other factors, such as remoteness, affordability, previous experiences of racism in health care environments for themselves, family or community members and fear of how they will be treated.
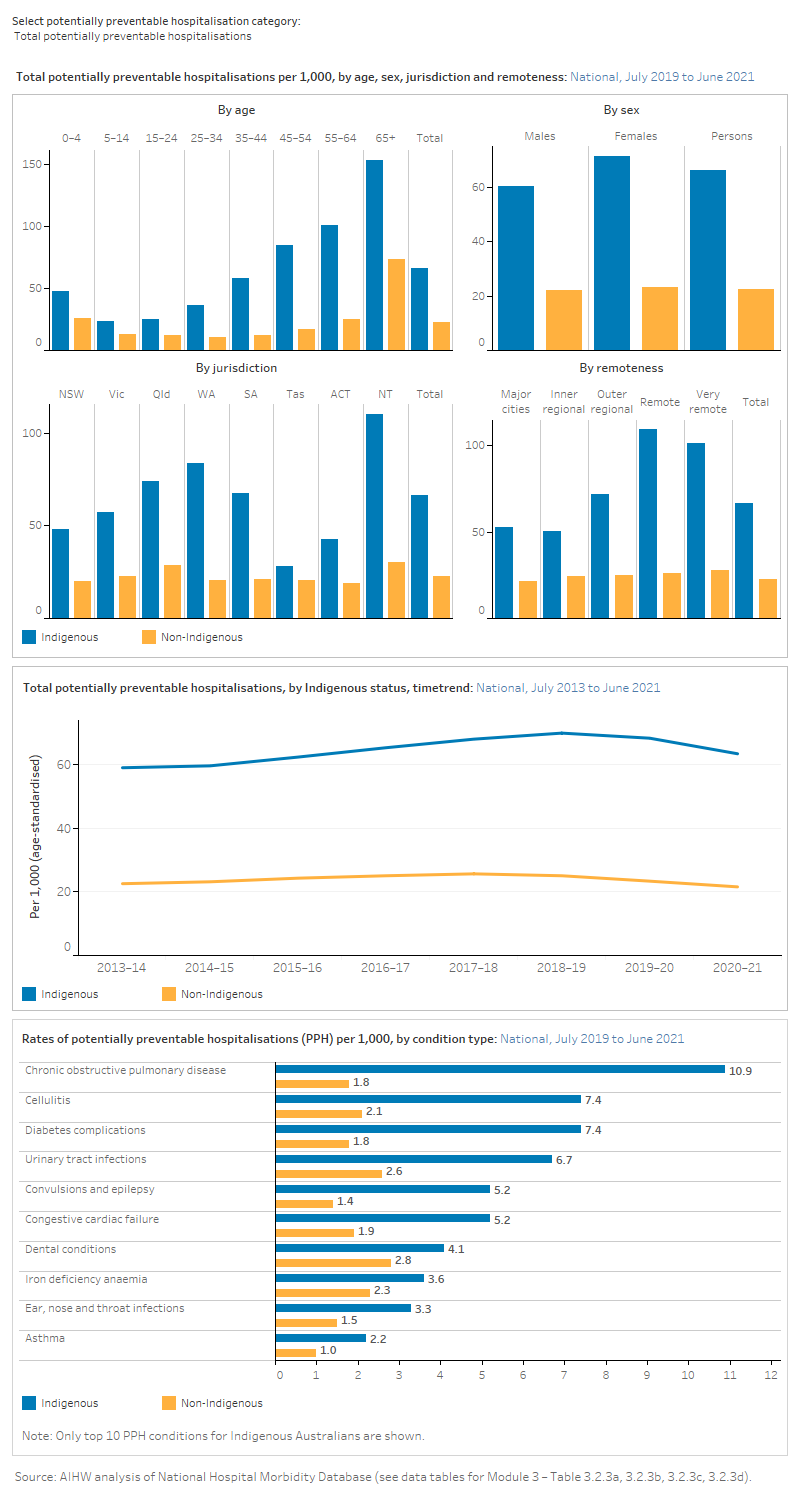
For example, potentially preventable hospitalisations (hospitalisations for conditions that can be effectively treated in a non-hospital setting) can serve as a proxy measure of access to timely, effective and appropriate primary and community-based care. Systematic differences in hospitalisation rates for Indigenous Australians and non-Indigenous Australians can indicate gaps in the provision of population health interventions, primary care services, and continuing care support. The rate of potentially preventable hospitalisations is affected by the interaction of a broad range of factors; however, culturally safe primary health care could help better detect and manage health risk factors and conditions and thereby reduce rates of potentially preventable hospitalisations.
What data are available?
New data were available to update 12 out of 13 measures reported in Module 3 for the 2023 release. One measure could not be updated as the Voluntary Indigenous Identifier (VII) was not updated. For more information, see 3.4 Specialist services and Technical notes.
The measures in this module are based on national administrative data collections covering immunisation, the Medicare Benefits Schedule (MBS), hospitals, mortality, perinatal and elective surgery waiting times.
For further information on the data sources used in this module, see Module 3 – Data sources and data gaps.
Key findings
Selected measures of access to health care services for Indigenous and non-Indigenous Australians are used to monitor disparities in access as they may indicate problems with the cultural safety of services, though many other factors can also impact on access to and use of services (for example, remoteness, affordability, previous experiences of racism, presence of co-morbidities).
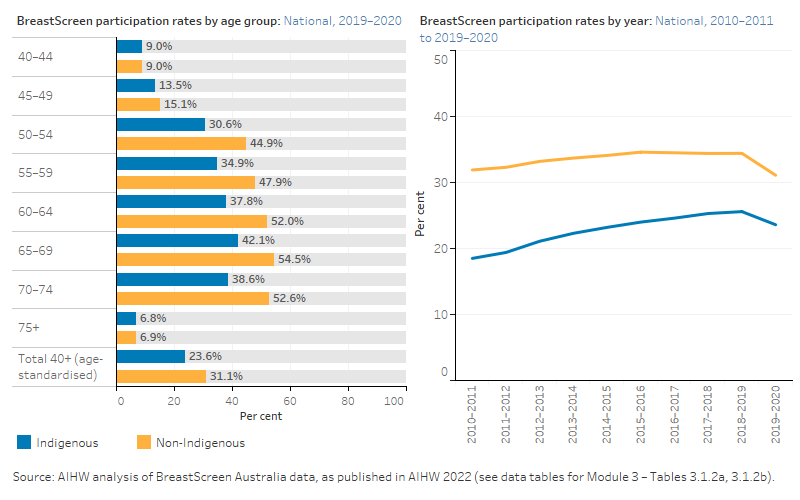
- Mammogram participation rates for Indigenous Australian women increased between 2010–2011 and 2018–2019. Rates decreased in 2019–2020, during the COVID-19 pandemic.
- In 2020–21, the rate of potentially preventable hospitalisations for Indigenous Australians was almost 3 times the rate for non-Indigenous Australians (66 compared with 23 per 1,000, based on age-standardised rates).
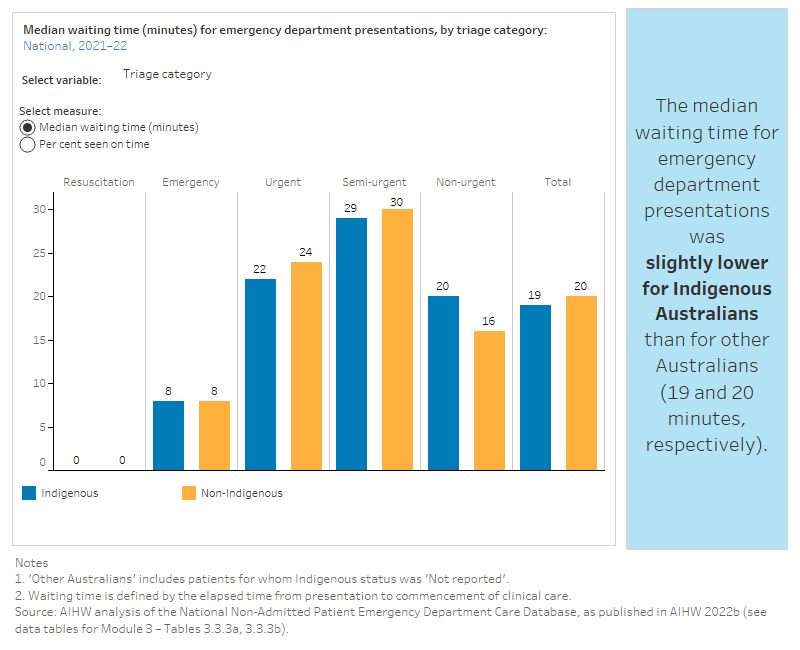
- In 2021–22, the median waiting time for emergency department presentations was similar for Indigenous Australians than for other Australians (19 and 20 minutes, respectively).
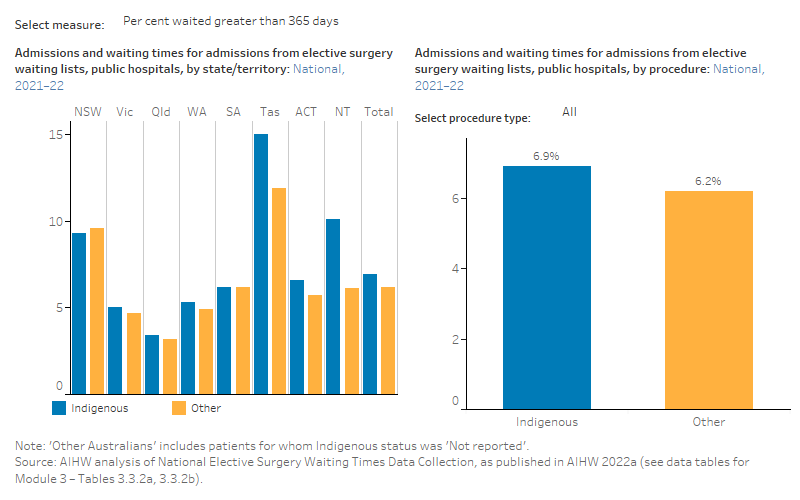
- Indigenous Australians waited longer to be admitted for elective surgery in 2021–22 than non-Indigenous Australians – 50% of Indigenous patients were admitted for elective surgery within 50 days, compared with 39 days for non-Indigenous patients.
- In 2021, of 6,749 registered cases of rheumatic heart disease, 78% were Indigenous Australians compared with 22% non-Indigenous Australians.
- In 2021, the avoidable mortality rate for Indigenous Australians was 208 per 100,000. The Indigenous age-standardised rate was over 3 times that for non-Indigenous Australians (296 and 91 per 100,000 respectively).
See Module 3 data tables for all data presented in this module.
Data gaps and limitations
Disparities in access may be due to a range of factors other than a lack of cultural safety. The data provide overall measures of access, but do not include information on all the factors that can impact on access, such as affordability, previous experiences of racism, the presence of co-morbidities or patient choice.
Module 3 domains:
Preventive health services, such as immunisation, can protect children and adults from harmful infectious diseases and prevent the spread of diseases amongst the community. Health screening services, such as breast screening, can help detect serious conditions and reduce mortality.
The data reported for these two measures come from the Australian Immunisation Register and BreastScreen Australia.
Rates of immunisation
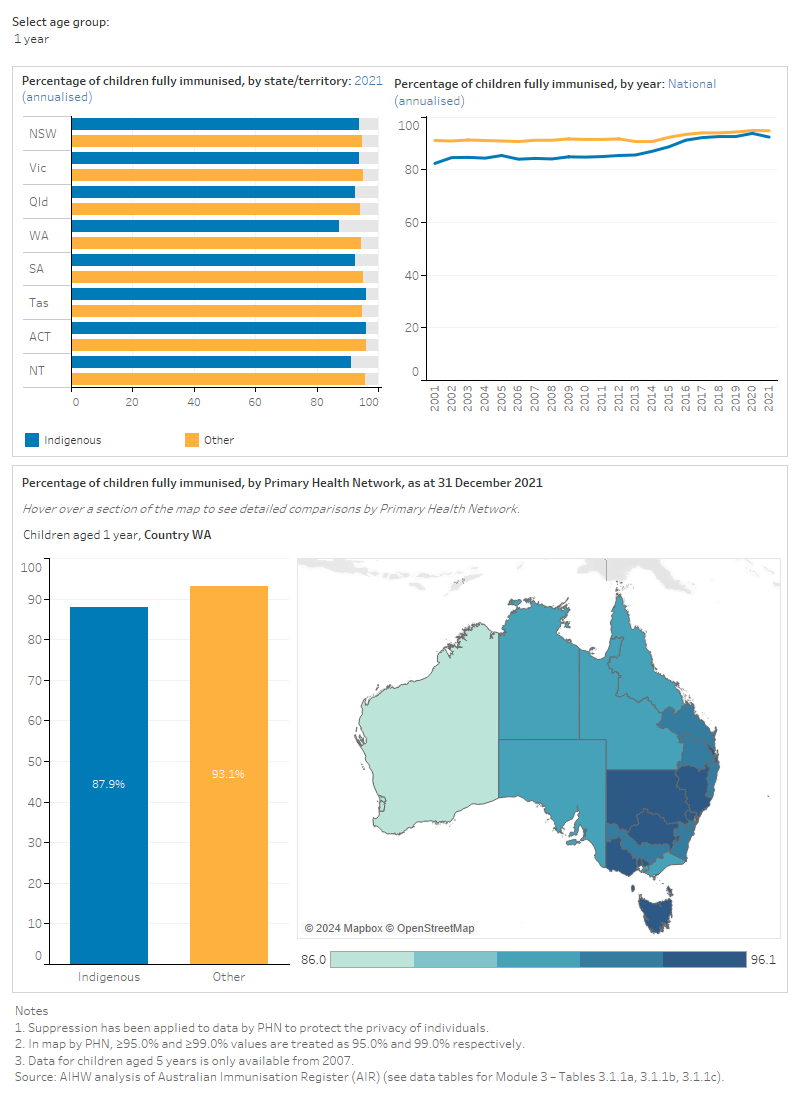
The figure is a set of interactive graphs showing the proportion of children that were fully immunised at age 1 year, 2 years and 5 years, by Indigenous status, state and territory, Primary Health Network and over time. See data tables for Module 3 – Tables 3.1.1a, 3.1.1b and 3.1.1c.
Participation rates for breast screening
The figure is a set of interactive graphs showing BreastScreen participation by Indigenous status, age group and over time. See data tables for Module 3 – Tables 3.1.2a and 3.1.2b.
References
AIHW (Australian Institute of Health and Welfare) 2022. BreastScreen Australia monitoring report 2022. Cat. no. CAN 150. Canberra: AIHW. Viewed 18 May 2023.
Primary health care services can help to keep people well and out of hospital by supporting them to manage their health issues in the community and at home, potentially avoiding health issues from becoming more serious. These services can reduce the need for specialist services and visits to emergency departments.
This domain has data on:
- Indigenous health checks: MBS items 715 and 228 (face-to-face), 92004 and 92011 (video-conference, available from March 2020), and 92016 and 92023 (teleconference, available from March 2020 to July 2021)
- antenatal care
- potentially preventable hospitalisations.
Indigenous health checks
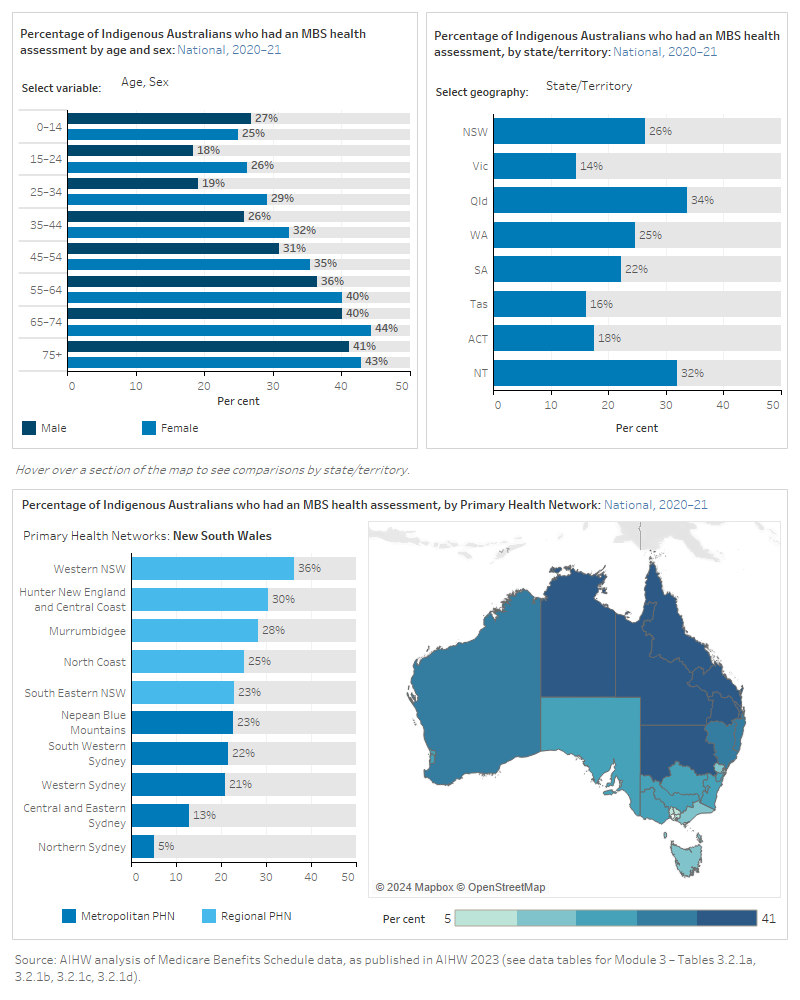
The figure is a set of interactive graphs showing the proportion of Indigenous Australians who had an Indigenous-specific health assessment face-to-face (MBS items 715 and 228), video-conference (92004 and 92011, available from March 2020) and teleconference (92016 and 92023, available from March 2020 to July 2021), by age group, sex, remoteness, state and territory, Primary Health Network and over time. See data tables for Module 3 – Tables 3.2.1a, 3.2.1b, 3.2.1c and 3.2.1d.
Access to antenatal care
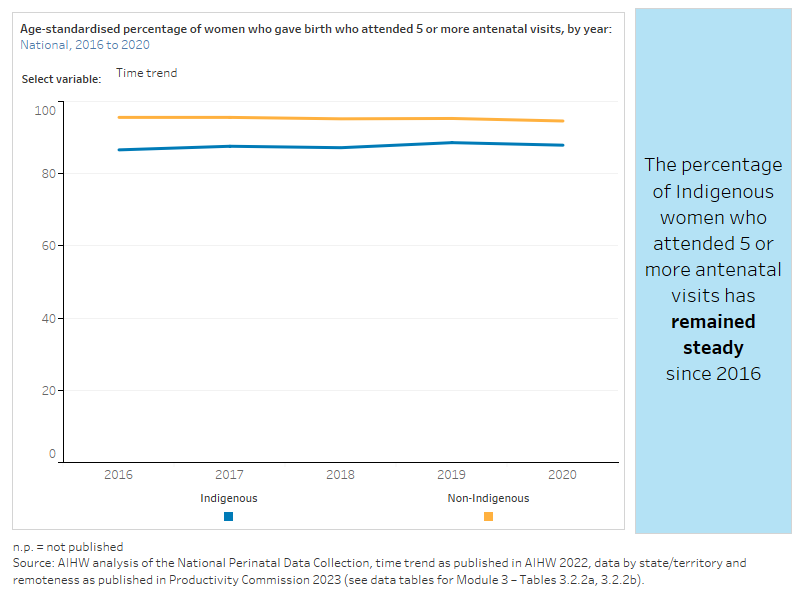
The figure is a set of interactive graphs showing the proportion of women who gave birth who attended 5 or more antenatal visits by Indigenous status, remoteness, state and territory and over time. See data tables for Module 3 – Tables 3.2.2a and 3.2.2b.
Potentially preventable hospitalisations
Potentially preventable hospitalisations are hospitalisations for conditions that can be effectively treated in a non-hospital system. These hospitalisations serve as a proxy measure for access to timely, effective and appropriate primary and community-based care. For more information, see Measure 3.07: Selected potentially preventable hospital admissions on the Aboriginal and Torres Strait Islander Health Performance Framework.
The figure is a set of interactive graphs showing the rate of potentially preventable hospitalisations (disaggregated by hospitalisations for acute conditions, chronic conditions, vaccine preventable conditions and total potentially preventable hospitalisations), by Indigenous status, age group, sex, state and territory, remoteness and over time. It also shows the rate of potentially preventable hospitalisations by condition type. See data tables for Module 3 – Tables 3.2.3a, 3.2.3b, 3.2.3c and 3.2.3d.
References
AIHW (Australian Institution of Health and Welfare) 2022. Australia’s mothers and babies. Cat. No. PER 101. Canberra: AIHW. Accessed 18 May 2023.
AIHW 2023. Eye health measures for Aboriginal and Torres Strait Islander people 2022. Cat. No. IHW 271. Canberra: AIHW. Accessed 18 May 2023.
Productivity Commission 2023. Socioeconomic outcome area 2: Aboriginal and Torres Strait Islander children are born healthy and strong. Closing the Gap Information Repository website. Canberra: Productivity Commission. Accessed 25 May 2023.
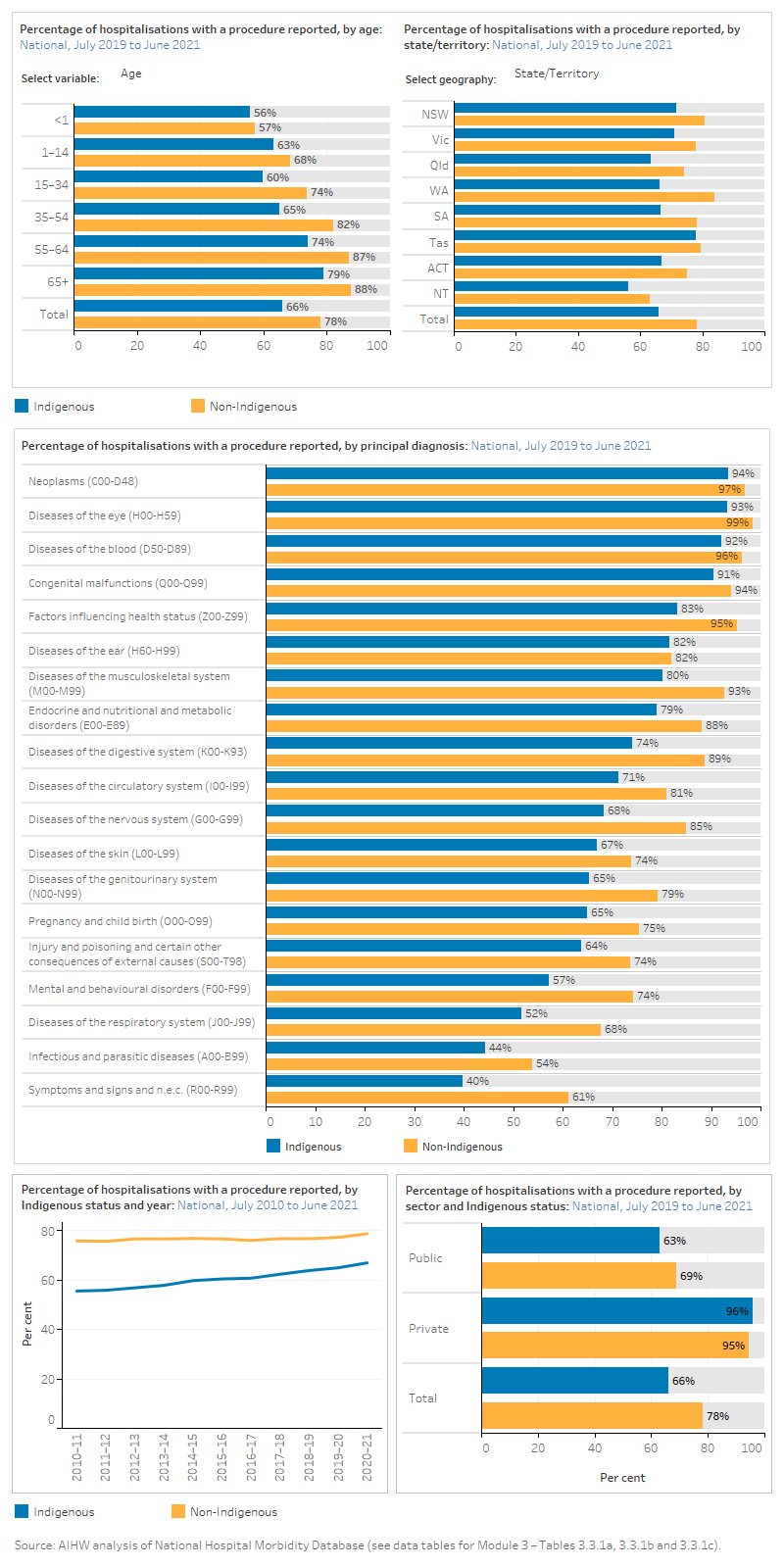
There are various measures that can be used to assess access to hospital services. Emergency department waiting times are one indicator of the accessibility of hospital services as they reflect how long patients have to wait for urgent medical attention, or to receive care as an admitted hospital patient. Access to medical procedures while in hospital are another indicator as studies have shown that while Aboriginal and Torres Strait Islander people are more likely to be hospitalised than other Australians, they are less likely to receive certain medical or surgical procedures. The data on waiting times for elective surgery also show that Indigenous Australians often wait longer to receive surgery.
Waiting times for almost all elective procedures became shorter between 2020–21 and 2021–22. However, as part of the early response to COVID-19, restrictions were placed on elective surgery in 2019–20, which led to longer waiting times for most intended procedures in 2020–21 (AIHW 2023).
Access to hospital procedures
The figure is a set of interactive graphs showing the proportion of hospitalisations with a procedure report, by Indigenous status, age, sex, remoteness, state and territory, principal diagnosis and over time. See data tables for Module 3 – Tables 3.3.1a, 3.3.1b and 3.3.1c.
Waiting times for elective surgery
The figure is a set of interactive graphs showing admissions for elective surgery, days waited at the 50th percentile, days waited at the 90th percentile and per cent who waited greater than 365 days, by Indigenous status and state and territory. See data tables for Module 3 – Tables 3.3.2a and 3.3.2b.
Emergency department waiting times
The figure is a set of interactive graphs showing the median waiting time (minutes) and per cent seen on time for emergency department presentations by Indigenous status, triage category and state and territory. See data tables for Module 3 – Tables 3.3.3a and 3.3.3b.
References
AIHW (Australian Institute of Health and Welfare) 2022a. Elective surgery. MyHospitals. Canberra: AIHW. Viewed 7 February 2023.
AIHW 2022b. Emergency department care. MyHospitals. Canberra: AIHW. Viewed 7 February 2023.
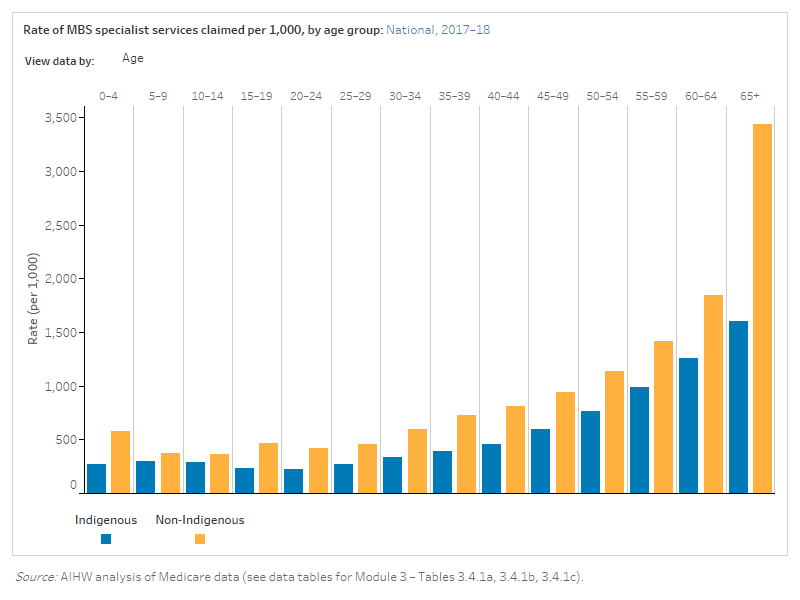
The Australian health system provides specialist treatment services to help people with a range of health concerns. Data are reported on specialist services claimed through the Medical Benefits Schedule (MBS), and on treatment of kidney failure, rheumatic heart disease and cataract surgery.
The MBS data presented here was derived using the Voluntary Indigenous Identifier (VII). Current VII data were not available in time for this report and therefore these measures have not been updated. For more information about the VII, see Voluntary Indigenous Identifier (VII) Framework on the Department of Health and Aged Care website.
MBS specialist services
This measure is calculated using VII data, which has not been updated. For a complete list of what data were available for the 2023 update, see Technical notes.
The figure is a set of interactive graphs showing the rate of MBS specialist services claimed, by Indigenous status, age group, service type and over time. See data tables for Module 3 – Tables 3.4.1a, 3.4.1b and 3.4.1c.
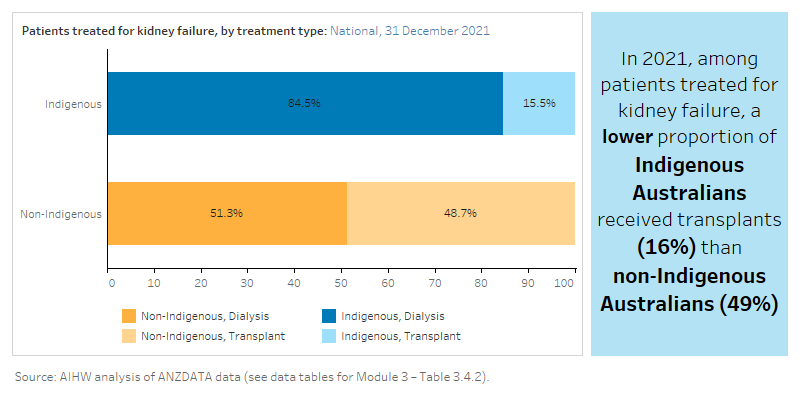
Treatment of kidney failure
The figure is a set of interactive graphs showing the treatment of kidney failure (either dialysis or transplant) by Indigenous status. See data tables for Module 3 – Table 3.4.2.
Rheumatic heart disease
The figure is a set of interactive graphs showing various indicators relating to Rheumatic heart disease, including registered cases, and proportion receiving prescribed penicillin doses, by Indigenous status. All data is only for Queensland, Western Australia, South Australia and Northern Territory. See data tables for Module 3 – Tables 3.4.3a, 3.4.3b.
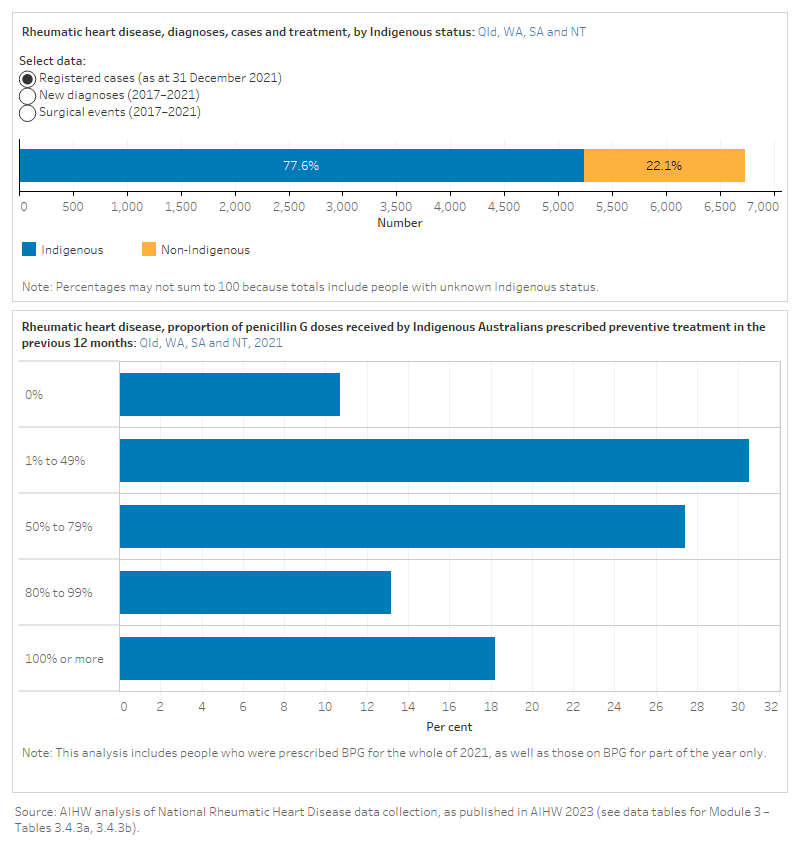
For more information on rheumatic heart disease, see AIHW reports Acute rheumatic fever and rheumatic heart disease in Australia 2017–2021 and Better Cardiac Care measures for Aboriginal and Torres Strait Islander people: seventh national report 2022 (data update).
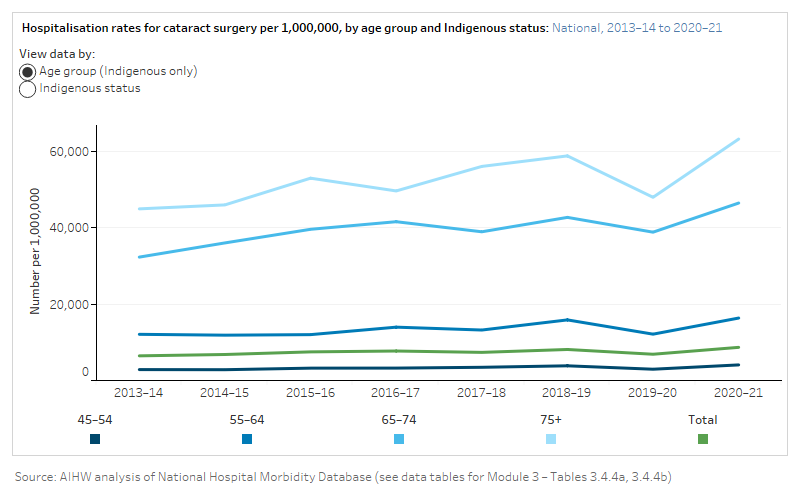
Cataract surgery
The figure is a set of interactive graphs showing hospitalisation rates for cataract surgery over time, by age (for Indigenous Australians only) or Indigenous status. Rates are presented per 1,000,000. See data tables for Module 3 – Tables 3.4.4a, 3.4.4b.
References
AIHW (Australian Institute of Health and Welfare) 2023. Acute rheumatic fever and rheumatic heart disease in Australia 2017-2021. Cat. no. CVD 99. Canberra: AIHW. Viewed 16 March 2023.
Avoidable mortality refers to deaths from conditions that are considered avoidable, given timely and effective health care, including disease prevention and population health initiatives. Avoidable mortality is one measure of the quality, effectiveness and accessibility of the health system. It should be noted, however, that deaths from most conditions are also influenced by factors other than access to health system services, including the underlying prevalence of conditions in the community, environmental and social factors, and health risk factors.
Avoidable deaths
The figure is a set of interactive graphs showing potentially avoidable deaths by Indigenous status and age, sex, state and territory, cause of death and over time. All data is only for New South Wales, Queensland, Western Australia, South Australia and the Northern Territory. See data tables for Module 3 – Tables 3.5.1a, 3.5.1b, 3.5.1c and 3.5.1d.
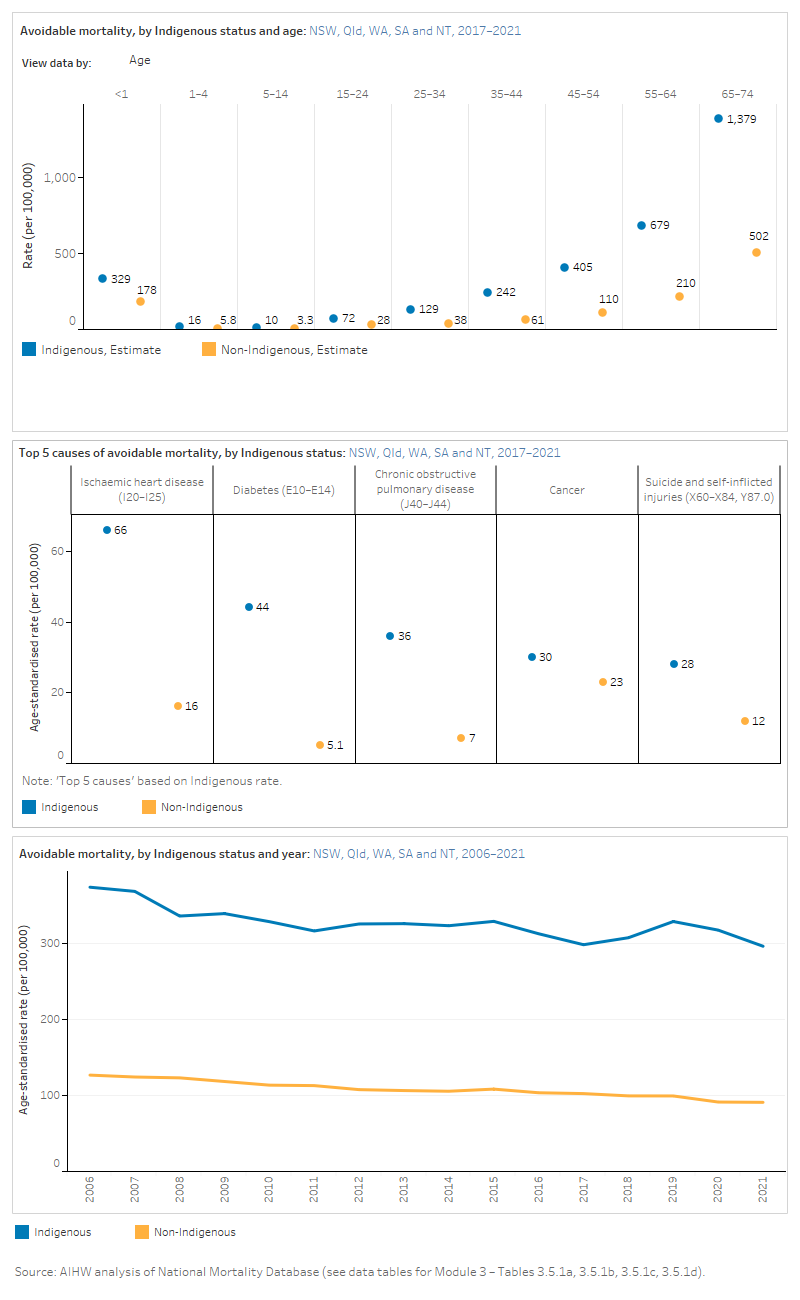
For more information, see Measure 1.24: Avoidable and preventable deaths on the Aboriginal and Torres Strait Islander Health Performance Framework.
The main data sources for the access to services measures were national data collections, mainly administrative data:
- Australian and New Zealand Dialysis and Transplant Registry
- Australian Immunisation Register
- BreastScreen Australia data
- Medicare Benefits Schedule data
- National Hospitals Data Collection
- National Elective Surgery Waiting Times Data Collection
- National Hospital Morbidity Database
- National Non‑admitted Patient Emergency Department Care Database
- National Mortality Database
- National Perinatal Data Collection
- National Rheumatic Heart Disease data collection.
There were data available for reporting on all measures in this module as they were based on existing national indicators or data collections.
| Domains and measures | Data sources |
|---|---|
| 3.1 Preventive health services | |
| Rates of immunisation | Australian Immunisation Register |
| Participation rates for breast screening | BreastScreen Australia data |
| 3.2 Primary health care | |
| Indigenous health checks | Medicare Benefits Schedule data |
| Access to antenatal care | National Perinatal Data Collection |
| Potentially preventable hospitalisations | National Hospital Morbidity Database |
| 3.3 Hospital services | |
| Access to hospital procedures | National Hospital Morbidity Database |
| Waiting times for elective surgery | National Elective Surgery Waiting Times Database |
| Emergency department waiting times | National Non-Admitted Patient Emergency Department Care Database |
| 3.4 Specialist services | |
| Specialist services claimed | Medicare Benefits Schedule data |
| Treatment of kidney failure | Australian and New Zealand Dialysis and Transplant Registry |
| Rheumatic heart disease | Rheumatic Heart Disease data collection |
| Cataract surgery | National Hospital Morbidity Database |
| 3.5 Overall health system | |
| Avoidable mortality | National Mortality Database |
Notes
The National Hospitals Data Collection includes the major national hospitals databases held by the AIHW. This report includes data from the following hospital data collections:
- The National Hospital Morbidity Database (NHMD), a compilation of episode-level records from admitted patient morbidity data collection systems in Australian public and private hospitals.
- The National Non-admitted Patient Emergency Department Care Database (NNAPEDCD), a compilation of episode-level records (including waiting times for care) for non-admitted patients registered for care in emergency departments in selected public hospitals.
- The National Elective Surgery Waiting Times Data Collection (NESWTDC), which holds episode-level information on patients added to or removed from elective surgery waiting lists managed by public hospitals.
For more information about these hospitals collections and the data quality statements see National Hospitals Data Collection and MyHospitals ‘About the Data'.
See the Aboriginal and Torres Strait Islander Health Performance Framework ‘Data sources and quality’ page for more information on AIHW data collections and other data collections presented in this module.


