Module 1: Culturally respectful health care services
Structures, policies and processes across the health system all play a role in delivering culturally respectful health care. The provision of culturally safe health care for Aboriginal and Torres Strait Islander people reflects the extent to which health care systems and providers are aware of and responsive to Indigenous Australians’ cultural needs and experiences. Cultural safety cannot be improved in isolation from the provision of health care.
What data are available?
New data were available to update 5 out of 12 measures reported in Module 1 for the 2023 release. The other 7 measures could not be updated due to discontinued data items in the Online Services Report (OSR). For more information see Data gaps and limitations, Data sources and data gaps and Technical notes.
The main information source of data for this module is the Online Services Report (OSR). OSR data is collected from organisations funded by the Australian Government to deliver primary health care services to Aboriginal and Torres Strait Islander people under the Indigenous Australians Health Program. The OSR includes organisations providing comprehensive primary care services and organisations providing maternal and child health programs and services. Mainstream services are not included in the OSR data.
The numbers and proportions of Indigenous Australians in the health workforce can also be obtained from the National Health Workforce Data Set and the ABS Census of Population and Housing (the census). Data from the National Health Workforce Data Set are presented in domain 1.3 below. Health labour force data from the census are presented in Measure 3.12 of the Aboriginal and Torres Strait Islander Health Performance Framework. The data from the census differ from the National Health Workforce Data Set due to differences in methodology.
In addition, national data are also reported on Indigenous Australians enrolled in health-related training courses and those registered across the health system, including GPs, nurses and some specialist doctors. The Indigenous workforce is integral to ensuring that the health system addresses the health needs of Indigenous Australians in a culturally safe and sensitive way.
For further information on the data sources used in this module, see Module 1 – Data sources and data gaps.
Key findings
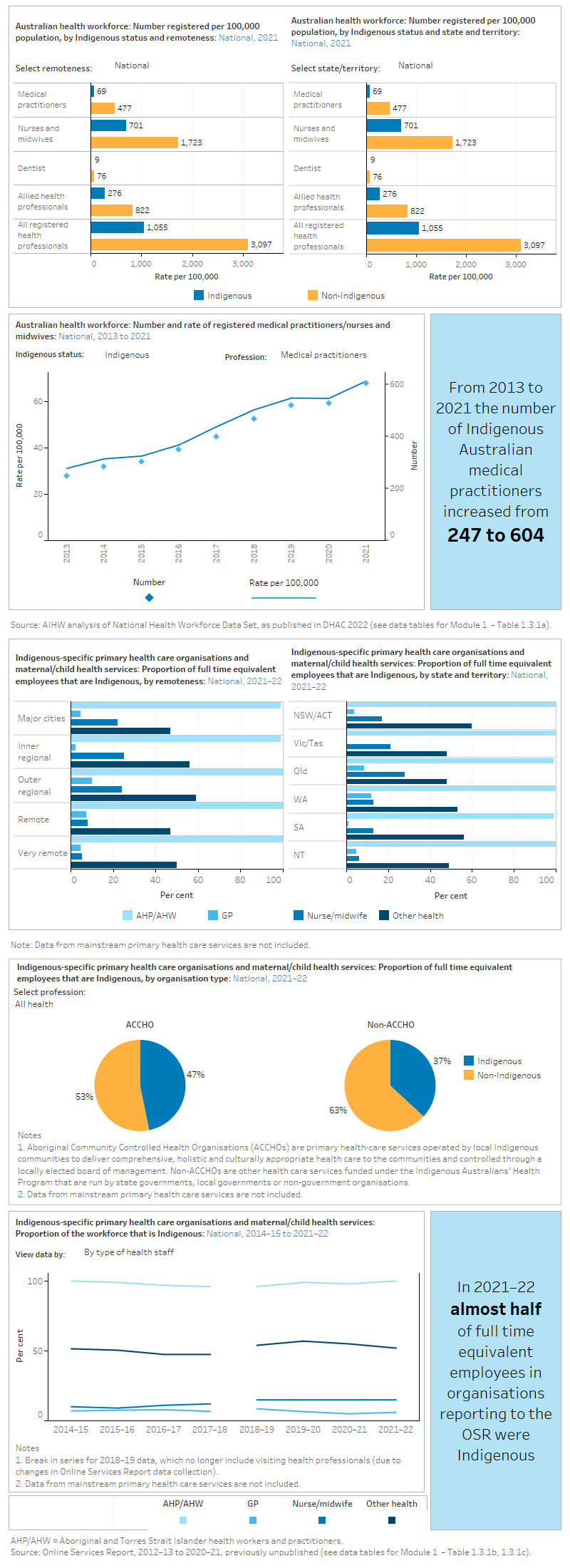
Among the Indigenous-specific primary health care organisations and maternal/child health services reporting to the OSR:
- Of the total 2,305 FTE employed in the services in 2021–22, 46% were Indigenous. This proportion varied by type of health staff:
- Aboriginal Health Practitioners/ Aboriginal Health Workers (960 FTE, 99.5%)
- other health workers including sexual health workers , traditional healers and trainees (1,114 FTE, 52%)
- GPs (42 FTE, 6.1%)
- nurses and midwives (189 FTE, 15%).
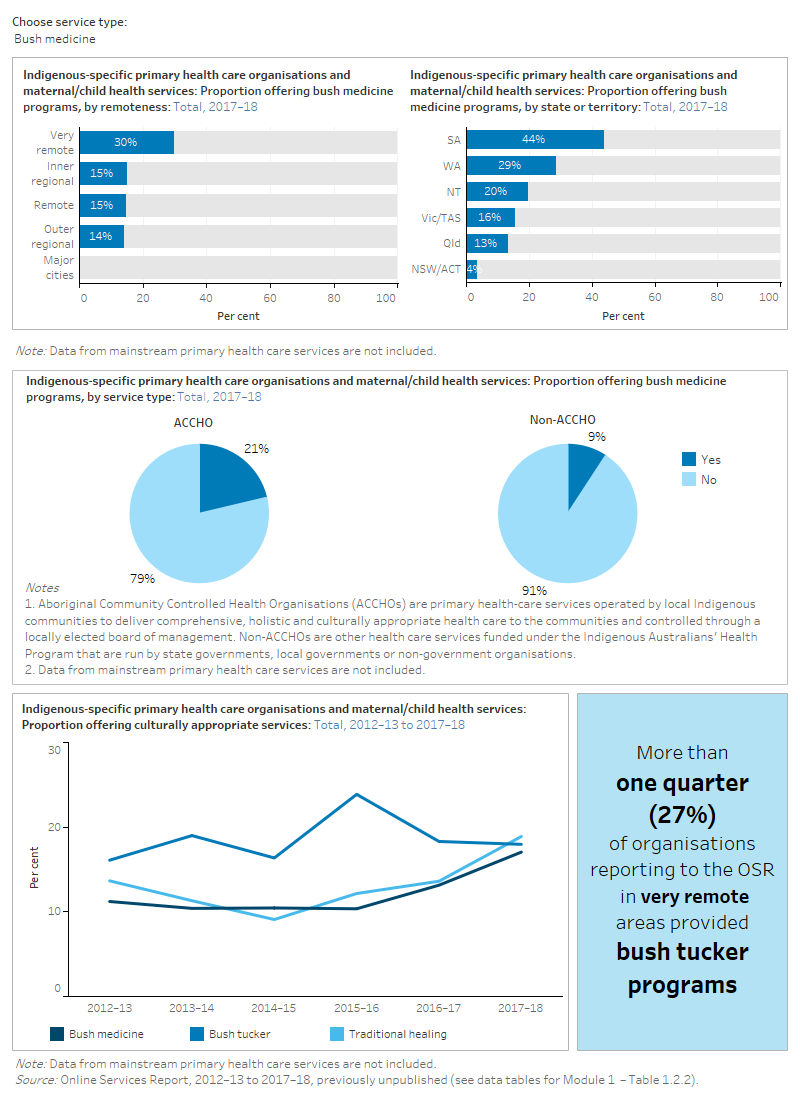
- Of the total 217 services, 40% provided interpreter services, while around one third offered culturally appropriate services such as bush tucker, bush medicine and traditional healing in 2017–18.
National health workforce data show that in Australia from 2013 to 2021, the number of Indigenous:
- medical practitioners registered increased from 247 to 604
-
nurses and midwives registered increased from 2,833 to 6,160.
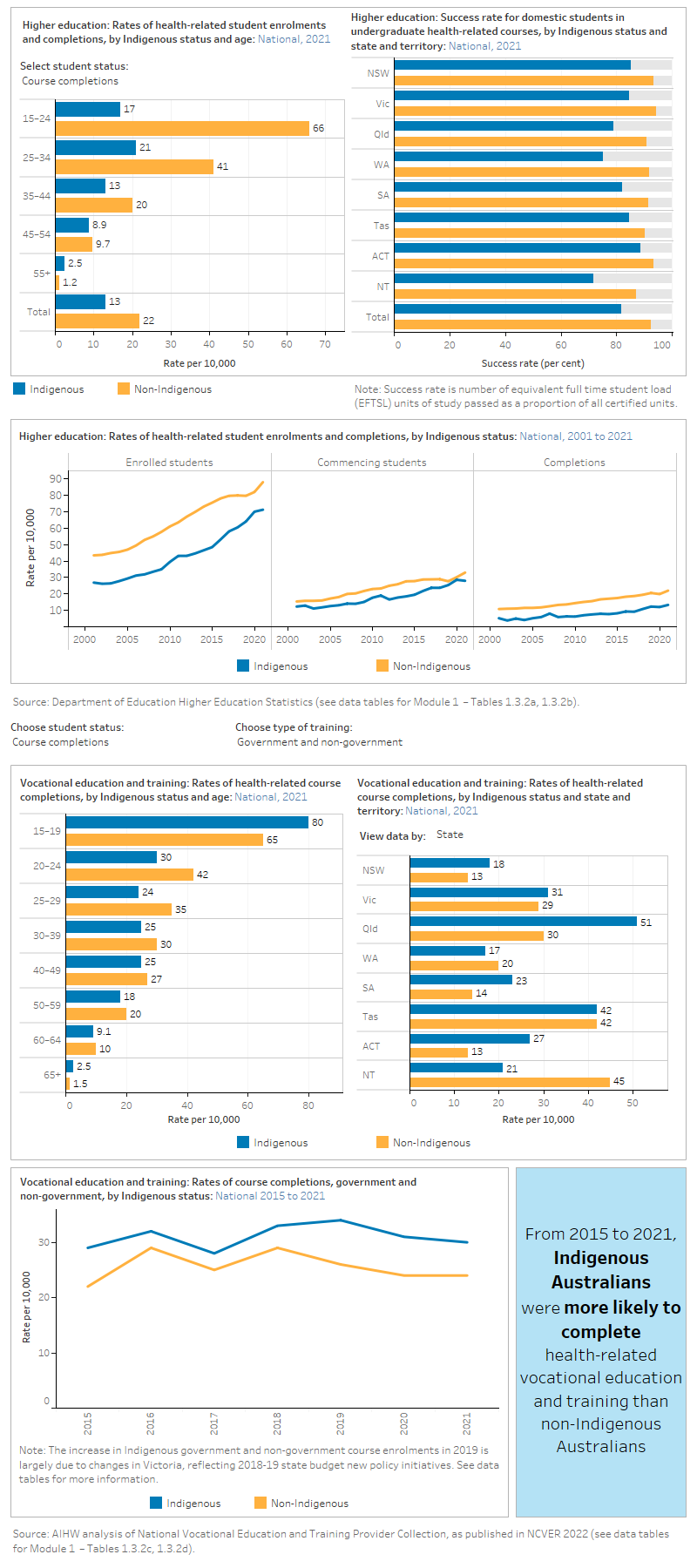
Higher education statistics from the Department of Education show that from 2001 to 2021, the rate of enrolment in health-related courses for Indigenous Australian students increased from 27 per 10,000 (931 students) to 71 per 10,000 (4,227 students).
See Module 1 data tables for all data presented in this module.
Data gaps and limitations
Following a review of the OSR and nKPI collections in 2018, the collection of specific OSR data items on cultural safety were paused (AIHW 2020). Data collected in 2017–18 reporting period are the latest data available on cultural safety from Indigenous specific primary health care services.
Data on cultural safety in mainstream health services, such as general practitioners, and public hospitals continue to be critical data gaps. Data on these services are required to provide a more comprehensive assessment of cultural safety across the Australian health system.
References
AIHW (Australian Institute of Health and Welfare) 2020. Review of the two national Indigenous specific primary health care datasets: The Online Services Report and the national Key Performance Indicators. Cat. no. IHW 222. Canberra: AIHW. Accessed 20 June 2023.
Module 1 domains
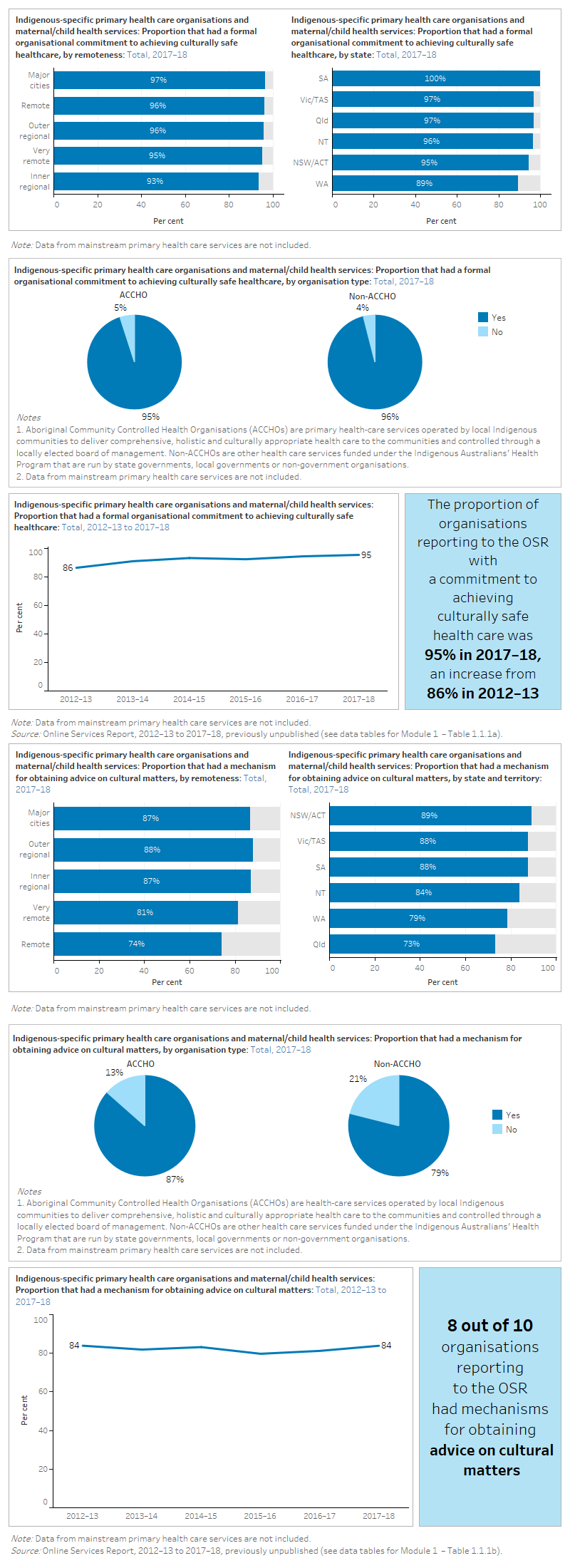
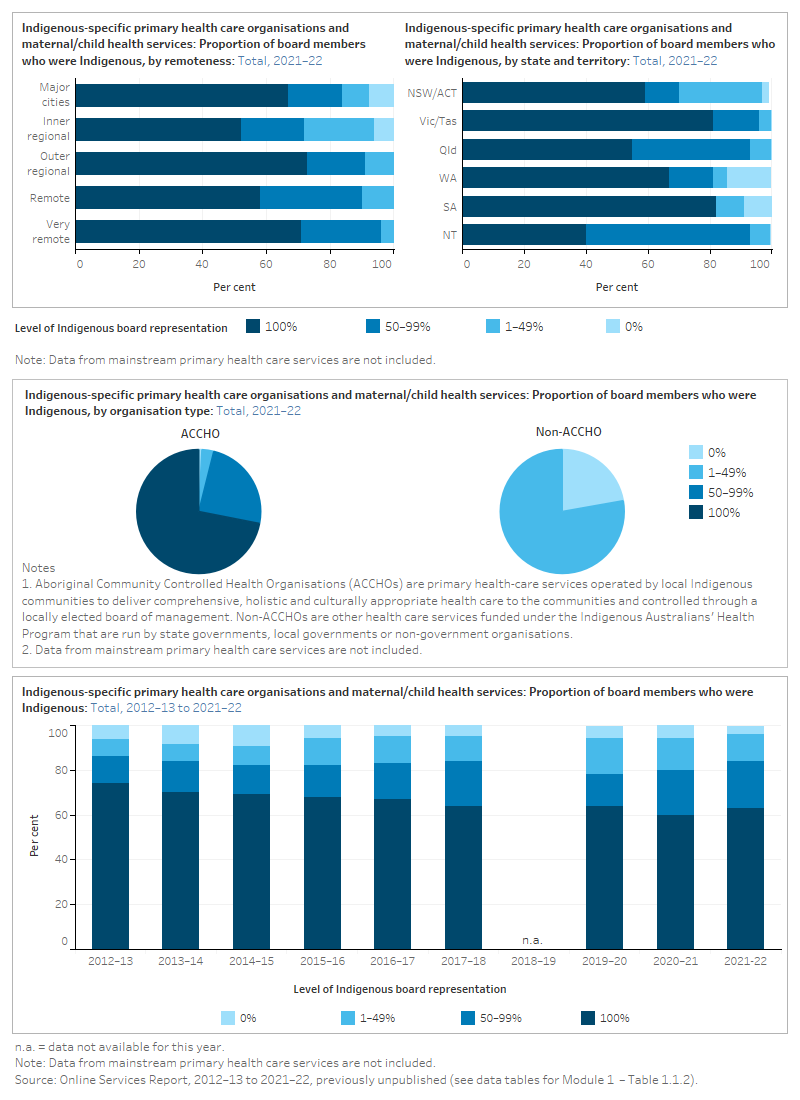
An organisational approach and commitment to providing culturally respectful and safe health care at the highest level is necessary but not sufficient to ensure care is culturally safe. Aboriginal and Torres Strait Islander leadership at the board or executive level can be an indicator that services are culturally aware and respectful. Data on these measures are provided from organisations funded to deliver comprehensive primary health care and/or maternal and child health services to Indigenous Australians. Data on Indigenous leadership at the board/executive level are available for 2021–22, while the latest available data on organisational approach and commitment are for the 2017–18 collection period.
Organisational commitment to culturally respectful and safe healthcare
The data items below are no longer collected. The most recent collection period for these data was 2017–18. For a complete list of what data were available for the 2023 update, see Technical notes.
This figure is a set of interactive graphs showing the proportion of Indigenous primary health care organisations and maternal/child health services that had a formal organisational commitment to achieving culturally safe healthcare, and the proportion of Indigenous primary health care services that had a mechanism for obtaining advice on cultural matters in 2017–18. Both measures are disaggregated by remoteness, state and territory, ACCHOs or non-ACCHOs, and over time. See data tables for Module 1 – tables 1.1.1a and 1.1.1b.
Aboriginal and Torres Strait Islander leadership at Board/Executive level
The figure is a set of interactive graphs showing the proportion of Indigenous primary health care organisations and maternal/child health services that had an Indigenous board in 2021–22, disaggregated by remoteness, state and territory, ACCHOs or non-ACCHOs, and over time. See data tables for Module 1 – Table 1.1.2.
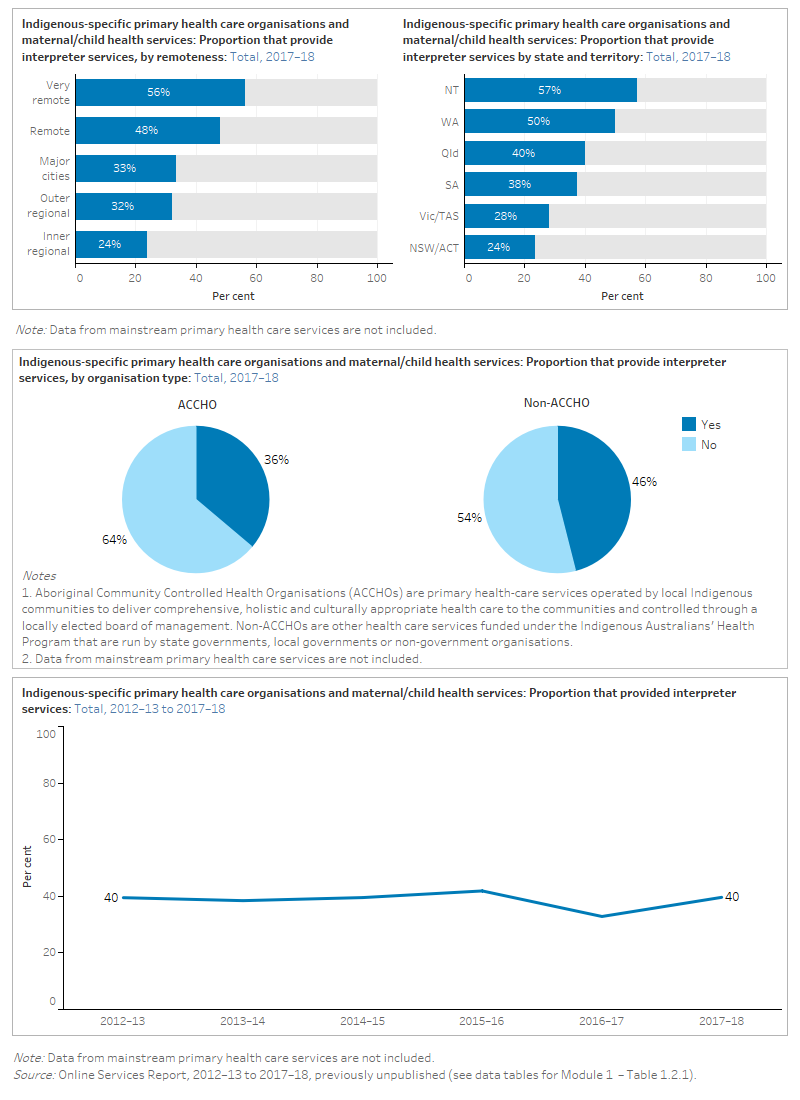
Health service environments that value Aboriginal and Torres Strait Islander culture by displaying Indigenous artwork and providing culturally appropriate resources, communications and other services can help to make Indigenous people feel culturally safe.
There are some data on communication and cultural services from organisations funded to provide comprehensive primary health care and maternal and/or child health services to Indigenous Australians. The latest data available from the OSR collection on communication and cultural services are for the 2017–18 collection period.
Culturally appropriate communication resources
The data items below are no longer collected. The most recent collection period for these data was 2017–18. For a complete list of what data were available for the 2023 update, see Technical notes.
The figure is a set of interactive graphs showing the proportion of Indigenous primary health care organisations and maternal/child health services that provided interpreter services in 2017–18, disaggregated by remoteness, state and territory, ACCHOs or non-ACCHOs, and over time. See data tables for Module 1 – Table 1.2.1
Offers culturally appropriate services
The data items below are no longer collected. The most recent collection period for these data was 2017–18. For a complete list of what data were available for the 2023 update, see Technical notes.
The figure is a set of interactive graphs showing the proportion of Indigenous primary health care organisations and maternal/child health services that provided culturally appropriate services (bush medicine, bush tucker or traditional healing) in 2017–18, disaggregated by remoteness, state and territory, ACCHOs or non-ACCHOs, and over time. See data tables for Module 1 – Table 1.2.2.
Aboriginal and Torres Strait Islander employees in the health workforce can increase the cultural safety of Indigenous patients because they understand the needs and priorities of Indigenous patients. National data are available on Indigenous enrolments in health-related courses and Indigenous participation in the health workforce for 2021 . Data on the health workforce and on cultural safety training among non-Indigenous staff are also available from organisations funded to provide comprehensive primary health care and/or maternal and child health services to Indigenous Australians with the latest data available from the OSR collection are for the 2017–18 collection period.
Aboriginal and Torres Strait Islander participation in the workforce
The figure is a set of interactive graphs showing the Australian health workforce by Indigenous status, remoteness, state and territory in 2021 and over time. It then shows the proportion of full time equivalent staff at Indigenous primary health care organisations and maternal/child health services that are Indigenous, by profession, remoteness, state and territory, ACCHOs or non-ACCHOs in 2021–22, and over time. See data tables for Module 1 – Tables 1.3.1a and 1.3.1b.
The Mayi Kuwayu team published a paper further describing trends in the Indigenous health workforce using ABS Census data from 2006, 2011 and 2016. The team found that while the number of Indigenous Health Workers had increased over this time (1,009 in 2006 to 1,347 in 2016), the rates showed a slight decrease (221 per 100,000 population in 2006 to 207 per 100,000 in 2016) (Wright et al. 2019). AIHW analysis of Census data also showed a slight decrease in the rate of Aboriginal and Torres Strait Islander Health Workers from 35 per 10,000 in 2006 to 30 per 10,000 in 2016. This increased to 32 per 10,000 in 2021 (AIHW forthcoming). See Measure 3.12 of the Aboriginal and Torres Strait Islander Health Performance Framework for more information. The rates published by the AIHW differ from those published by Mayi Kuwayu due to differences in methodology.
Aboriginal and Torres Strait Islander workforce development
The figure is a set of interactive graphs showing the rates of health-related student enrolments, commencing students and completions in higher education in 2021, by Indigenous status, age group and over time, as well as the success rate of students by Indigenous status and state and territory. It then shows the rates of health-related vocational education and training course enrolments and completions in 2021, by Indigenous status, state and territory, remoteness and over time. See data tables for Module 1 – Tables 1.3.2a, 1.3.2b, 1.3.2c and 1.3.2d.
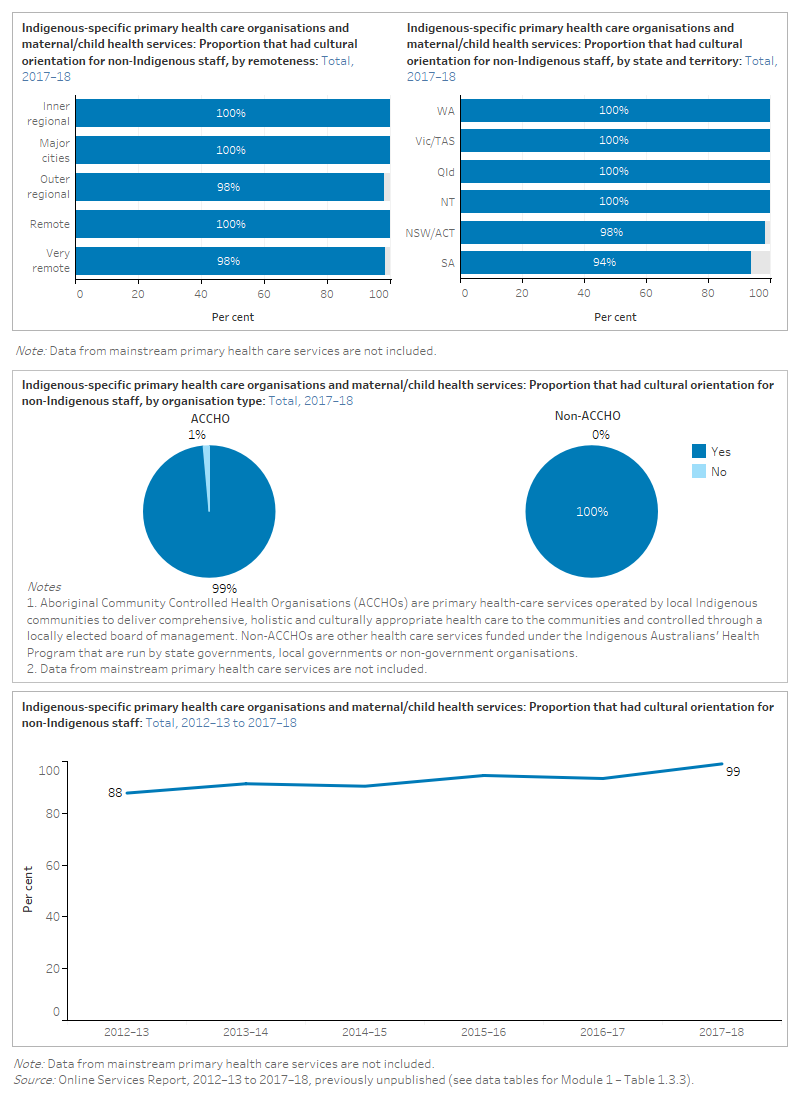
Cultural safety and responsiveness training for staff
The data items below are no longer collected. The most recent collection period for these data was 2017–18. For a complete list of what data were available for the 2023 update, see Technical notes.
The figure is a set of interactive graphs showing the proportion of Indigenous primary health care organisations and maternal/child health services that offered cultural orientation for non-Indigenous staff in 2017–18, disaggregated by remoteness, state and territory, ACCHOs or non-ACCHOs, and over time (from 2012–13). See data tables for Module 1 – Table 1.3.3.
References
AIHW (Australian Institute of Health and Welfare) forthcoming. Measure 3.12: Aboriginal and Torres Strait Islander people in the health workforce. Aboriginal and Torres Strait Islander Health Performance Framework website.
DHAC (Department of Health and Aged Care) 2022. Health Workforce Data [TableBuilder]. DHAC website. Accessed 10 February 2023.
NCVER (National Centre for Vocational Education Research) 2022. VOCSTATS [TableBuilder]. NCVER website. Accessed 10 February 2023.
Wright A, Briscoe K and Lovett R 2019. A national profile of Aboriginal and Torres Strait Islander Health Workers, 2006-2016. Australian and New Zealand Journal of Public Health. 43(1):24–26. doi:10.1111/1753-6405.12864.
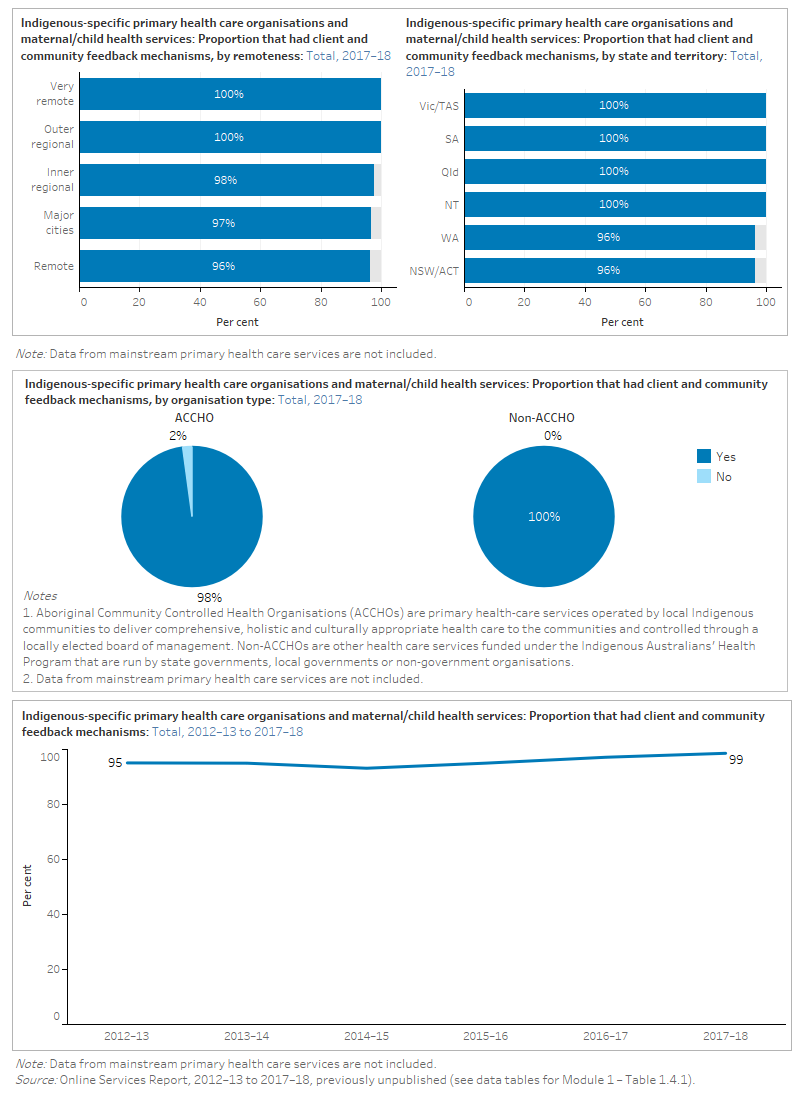
Client and community feedback is important for health services to ensure that their policies and programs are meeting the needs of Aboriginal and Torres Strait Islander communities. Collaboration with Indigenous organisations is also important for ensuring services are culturally respectful. Data on these measures are provided from organisations funded to provide comprehensive primary health care and/or maternal and child health services to Indigenous Australians. The latest data available from the OSR collection on consumer engagement and stakeholder collaboration are from 2017–18.
Client and community feedback mechanisms
The data items below are no longer collected. The most recent collection period for these data was 2017–18. For a complete list of what data were available for the 2023 update, see Technical notes.
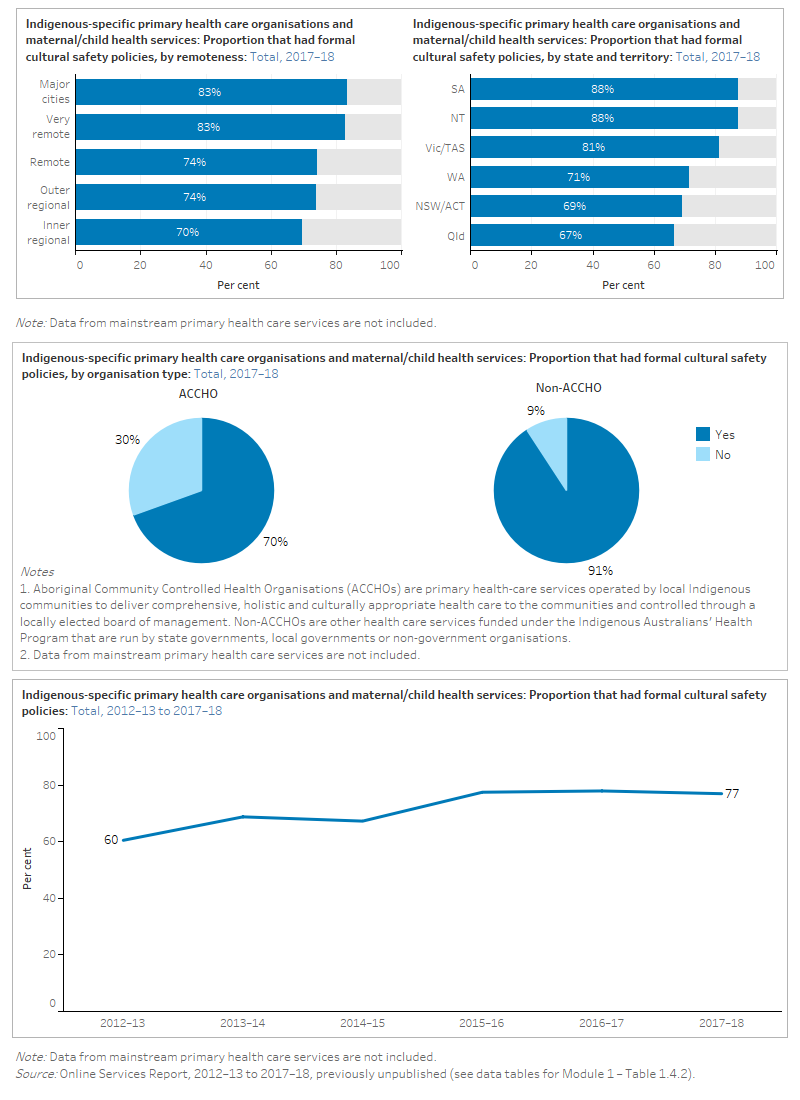
The figure is a set of interactive graphs showing the proportion of Indigenous primary health care organisations and maternal/child health services that had formal cultural safety policies in 2017–18, disaggregated by remoteness, state and territory, ACCHOs or non-ACCHOs, and over time (from 2012–13). See data tables for Module 1 – Table 1.4.2.
Consultation with Aboriginal and Torres Strait Islander communities
The data items below are no longer collected. The most recent collection period for these data was 2017–18. For a complete list of what data were available for the 2023 update, see Technical notes.
The figure is a set of interactive graphs showing the proportion of Indigenous primary health care services that had formal cultural safety policies in 2017–18, disaggregated by remoteness, state and territory, ACCHOs or non-ACCHOs, and over time (from 2012–13). See data tables for Module 1 – Table 1.4.2.
The following sources were included for this module:
- Online Services Report (OSR) – for data on Indigenous-specific primary health care organisations and maternal/child health services funded through the Indigenous Australians’ Health Program
- Higher Education Statistics and National Vocational Education and Training data – for data on enrolments in health-related courses
- National Health Workforce Dataset – for information on the characteristics of the health workforce.
| Domains and measures | NHWD | HES/VET | OSR |
|---|---|---|---|
| 1.1. Organisational approach and commitment | |||
|
Organisational commitment to culturally respectful and safe healthcare |
✓ |
||
|
Aboriginal and Torres Strait Islander leadership at Board/Executive level |
✓ |
||
| 1.2. Communication and cultural services | |||
|
Culturally appropriate communication resources (brochures, interpreters) |
✓ |
||
| Offers culturally appropriate services |
✓ |
||
| 1.3. Workforce development and training | |||
| Aboriginal and Torres Strait Islander participation in the workforce |
✓ |
✓ |
|
| Aboriginal and Torres Strait Islander workforce development |
✓ |
||
| Cultural safety and responsiveness training for staff |
✓ |
||
| 1.4 Consumer engagement and stakeholder collaboration | |||
| Client and community feedback mechanism |
✓ |
||
| Consultation with Aboriginal and Torres Strait Islander communities |
✓ |
Note: OSR – Online Services Report; HES – Higher Education Statistics; VET – Vocational Education and Training statistics; NHWD National Health Workforce Dataset; NHMD – National Hospital Morbidity Database.
Notes
Most of the available data for this module comes from the AIHW Online Services Report (OSR) data collection and relates to Indigenous-specific primary health care and maternal and child health services. These services include Aboriginal Community Controlled Health Organisations (ACCHOs), government and non-government organisations funded under the Indigenous Australians’ Health Program (IAHP).
For 2019–20, 2020–21 and 2021–22, reporting to the OSR collection was made voluntary in acknowledgement of the additional pressures on organisations because of COVID-19, therefore data should be interpreted with caution. For more information see Impact of COVID-19.
| Collection year | Number of primary care organisations | Number of organisations funded for maternal and child health services only |
|---|---|---|
| 2017–18 | 198 | 19 |
| 2018–19 | 210 | 22 |
| 2019–20 | 196 | 19 |
| 2020–21 | 191 | 20 |
| 2021–22 | 211 | 19 |
For further information see OSR – summary over time.
The OSR has a module-based structure, with individual items that are a mix of counts of activities/services provided (such as number of clients seen), workforce information, questions with tick box answers, and some text responses. The OSR collection includes data on staffing levels, client numbers, client contacts, episodes of care and services provided.
Contextual information about each organisation is also collected. The OSR data presented in this monitoring framework are drawn from the:
- community engagement, control and cultural safety module, which consists of mostly tick box answers about activities undertaken by organisations to deliver culturally safe services to Indigenous clients
- corporate services/infrastructure module, workforce submodule, which consists mostly of counts of FTE staff by Indigenous status and various role/function categories.
See Supplementary material: Cultural safety-related questions from the OSR data collection for more information.
OSR data presented in the monitoring framework are also disaggregated by type of organisation – that is, by whether it is an ACCHO or other organisation receiving funding under the IAHP.
The OSR collection is being redeveloped and as a result some items have not had updated data since the 2017–18 reporting period. For more information about OSR see:
- Aboriginal and Torres Strait Islander-specific primary health care: results from the OSR and nKPI collections – Interpreting OSR data
- Online Services Report data collection.
The National Health Workforce Dataset provides national data on the Indigenous status of the health workforce for a wide range of professions, including GPs, nurses, and medical specialists. The Higher Education and Vocational Education and Training data provide information on the Indigenous status of student enrolments and completions for health-related courses, such as:
- nursing
- medical studies
- pharmacy
- dentistry
- some allied health; for example, rehabilitation therapies and optical science
- other health, which includes Aboriginal and Torres Strait Islander health workers.
These data are important for monitoring programs that aim to build an Indigenous health workforce to help improve the cultural safety of health services.
Data gaps
There is little relevant data from mainstream services, such as primary health care and hospitals, across all levels of geography, from national to regional. A high proportion of Indigenous Australians use mainstream services, including in regional and remote areas.
There are also gaps in workforce data below state and territory levels of geography, such as at the Primary Health Network (PHN) level.
The Australian Commission on Safety and Quality in Health Care (ACSQHC) has included six Aboriginal and Torres Strait Islander specific actions in the National Safety and Quality Health Service Standards. The aims of the Standards are to protect the public from harm and to improve the quality of health service provision. However, data from the ACSQHC is not available to use for reporting in the monitoring framework.
The current monitoring framework focuses on the experience of the patient in the health care system. However, the experience of health care professionals and the cultural safety for Indigenous Australians in the health workforce are important aspects of a system free from racism.


