Data opportunities
In 2022, under the National Mental Health and Suicide Prevention Agreement, Bilateral Schedules (Bilateral Schedules) between state and territory health authorities and the Australian Government were developed to support the enhanced collection and reporting of perinatal mental health data from public antenatal and postnatal care settings, and the provision of perinatal mental health data to the AIHW (Commonwealth of Australia 2022). This work builds on efforts that commenced in 2010 with extensive consultation with subject matter and data experts, and supports the National Perinatal Depression Initiative which recommended nationally consistent perinatal mental health data to inform analysis, service provision and decision making (Highet and Purtell 2012). The collection of woman-reported data also supports the delivery of woman-centred continuity of care and improved outcomes and experiences for women and their families (COAG Health Council 2019).
Despite challenges, there are a number of developments and opportunities underway to harness these data:
Mental health and family violence Perinatal NBEDS items
State and territory health authorities are at different stages of implementing the four mental health and family violence Perinatal NBEDS items, for a variety of reasons. Data quality, comparability, and universal coverage are required before the data items can progress to become mandatory as part of the Perinatal NMDS.
The AIHW is undertaking extensive stakeholder engagement with state and territory health authorities through the Perinatal Mental Health Jurisdictional Data Working Party (Working Party) to understand the challenges experienced in implementing and collecting these data items, and to ensure that these data items are fit-for-purpose and a priority for jurisdictional and national data development. For example, for the Perinatal NBEDS Presence or history of mental health condition indicator data item, Working Party members are considering how analysis of PMHp data, which includes the self-reported mental health history from the ANRQ and SAFE START Psychosocial questions, could provide evidence to improve the consistency and comparability of the data collected.
Each state and territory health authority’s perinatal data collection, which feeds into the NPDC, is typically sourced from data collected by midwives or other birth attendants shortly after the mother has given birth. Data may also be sourced from information that has been previously electronically captured through the woman’s antenatal care. At present there is limited capacity to collect additional mental health-related items in the NPDC. Data about the postnatal period after discharge are out of scope for the NPDC.
Perinatal Mental Health pilot
The Perinatal Mental Health pilot (PMHp) is a novel collection of de-identified screening data sourced from public antenatal and postnatal maternity health services. In mid-2023, the AIHW received the first tranche of PMHp data from South Australia’s Northern Adelaide Local Health Network (NALHN). Analysis is underway including sharing service-level data back to NALHN through the AIHW’s Perinatal Portal, a secure platform to share perinatal data and insights with perinatal service providers.
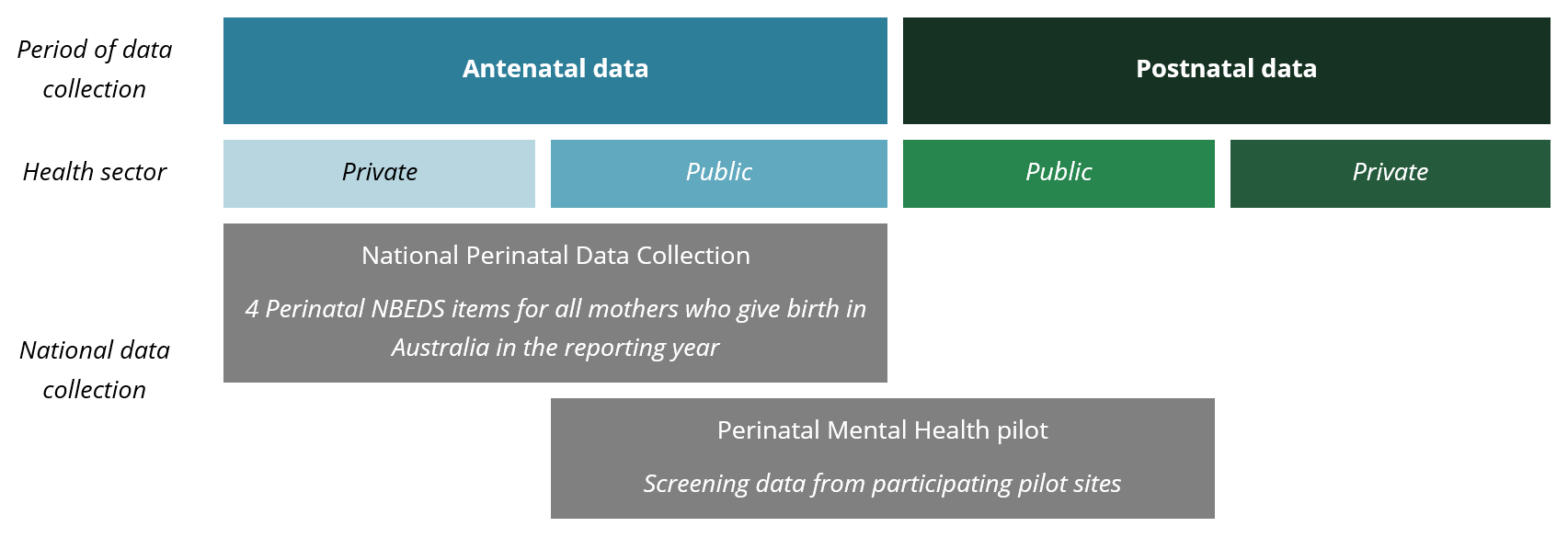
The PMHp will grow iteratively in scope and coverage over time, as state and territory health authorities and health services commit to contributing their public antenatal and postnatal maternity service data. The AIHW has received interest from Queensland and New South Wales (NSW) to participate in the PMHp. As such the PMHp is a small but growing sample of the antenatal and postnatal mental health screening occurring across Australia. The PMHp aims to complement the NPDC (Figure 4), by collecting data that is currently out of scope for the NPDC, such as postnatal data and psychosocial risk factor screening data from participating pilot sites.
Figure 4. Scope of the National Perinatal Data Collection and Perinatal Mental Health pilot
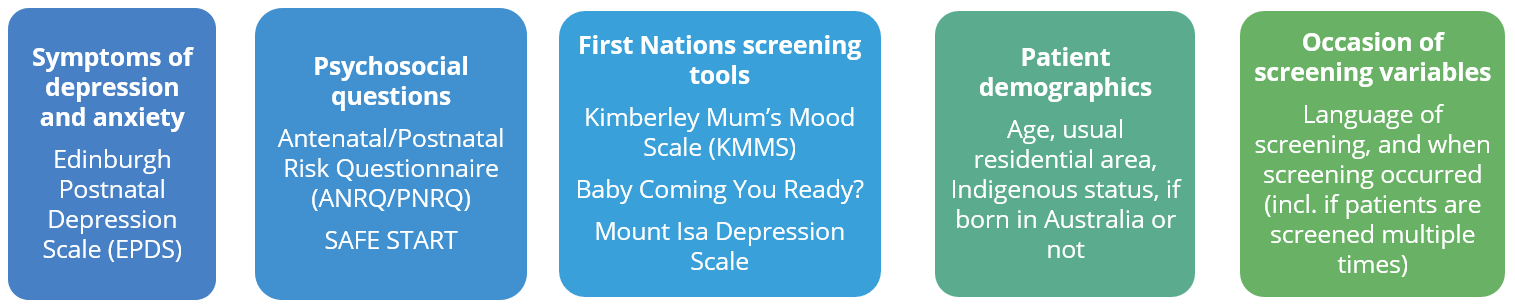
The PMHp will trial a new way to collect and report perinatal mental health screening data. Noting that screening practices differ across the country, the PMHp has a flexible scope, with ongoing AIHW ethics approval to collect a broad range of data including:
Key areas for investigation
The PMHp will provide valuable insights about variation in perinatal mental health screening uptake and the prevalence of psychosocial risk factors by maternal age, socioeconomic level, Indigenous status, geographic region, and language, and changes over time; these insights will inform clinical decision making and benchmarking progress. For example, the PMHp will enable analysis of:
- All EPDS scores (not just the total score): This will provide insights in relation to whether patients report thoughts of self-harm (Question 10), and their anxiety risk (EPDS questions 3, 4 and 5, and ANRQ questions relating to trait anxiety and perfectionism), noting further investigation is needed to assess the validity of the anxiety items (Austin et al. 2022; Smith-Nielsen et al. 2021).
- When and how screening is conducted: To inform interpretation of these data, the PMHp is seeking to collect data from all occasions of screening, including how many weeks pregnant or postpartum the woman was at the time of screening. This will allow exploration of the patient journey through contact points with maternity services by considering factors including repeat screening, whether women were screened in both the antenatal and postnatal periods, differences between initial and subsequent screens, and whether at-risk patients (EPDS score 13 or higher) received follow-up screening within the recommended period.
- Presence or history of mental health condition indicator data item: Analysis of PMHp data will also support efforts to improve this data item in the Perinatal NBEDS.
- Psychosocial risk factors refer to prior mental health history, availability of support systems and feeling safe with their partner, experiences of abuse, alcohol or other drug concerns, and experience of giving birth and parenting. Collecting these data will provide a fuller picture of women’s perinatal mental health and build understanding of the different tools used to conduct psychosocial risk factor screening across the country.
- Protective factors interact with risk factors and are relative to the individual and their psychological, social, environmental, and cultural needs. Improved understanding about risk factors of mental health conditions through screening in the perinatal period, will help improve understanding about protective factors, such as social support, physical activity, and coping strategies before and after childbirth, as well as positive mother-infant interaction.
- Priority populations such as First Nations people and CALD communities, particularly as mainstream approaches may not be the most suitable for these populations. The iCOPE screening platform includes First Nations-specific screening tools and is available in 24 languages other than English. By collecting the language of screening, it will allow recommended lower cut off scores to be accounted for when analysing the data. The AIHW is also exploring opportunities to include perinatal mental health screening of fathers and other non-birthing parents which the iCOPE screening platform facilitates.
Data linkage
Data linkage is a process that combines information from multiple data collections to tell a richer story than would be possible from a single data source. This maximises the utility of existing data sources and minimises the burden and cost of collecting additional data.
There is potential, with relevant approvals, to link the NPDC to other health and welfare related data collections. This will build an understanding about patterns of mental health care use by women before, during and after pregnancy, and health outcomes for mothers and babies. For example, linking the NPDC to:
- MBS will provide insight into use of mental health-related Medicare subsidised services, including from GPs, psychiatrists, psychologists and other allied health workers
- PBS will provide insight into use of mental health-related prescription medications
- Hospital admitted patient data will provide insight into hospital admissions for mental health and intentional self-harm
- Hospital ED will provide insight into mental health-related ED presentations
- Community mental health data will provide data about women treated in specialist community and hospital-based outpatient care services provided by state and territory governments. These are collectively referred to as community mental health care (CMHC) services and contribute data to the Community Mental Health Care National Minimum Data Set (CMHC NMDS). The CMHC NMDS does not include data from non-government funded community services such as not-for-profit organisations.
- Mortality data will provide data about women who die by suicide in the postnatal period, beyond 42 days after birth. Linkage with the above data sources, will also provide insight into mental health service use and medication use by these women, compared with women who have not died by suicide.
These insights will inform service planning and policy, to help ensure women and families get the care they need, when they need it.
Development of primary health care data
GPs and other primary health care providers play a key role in the delivery of antenatal and postnatal mental health screening, referral and care. As noted earlier, MBS data offers limited insight into the delivery of these services and patient outcomes, without linkage to other data collections.
There are information gaps in primary health care data that make it difficult to understand a patient’s journey through the health care system. A variety of clinical information systems are used in primary health care settings, and there are also different tools for extracting data from these systems, which can make it difficult to collate data into a national collection.
There are a number of large-scale projects underway to improve the availability of primary health care data, and it may be possible to leverage these projects to give insight into the screening and management of perinatal mental health conditions in general practice, particularly for women in the postnatal period:
- The AIHW is developing a National Primary Health Care Data Collection (NPHCDC), with an initial focus on general practice activity data. The AIHW has consulted across the primary health care sector and is now working collaboratively with PHNs to conduct small-scale data demonstration projects. The goal of these projects is to generate a comprehensive overview of the current state of general practice data in Australia. The first data demonstration project commenced in 2023 and is focused on general practice data on dementia. A long-term aim is for the NPHCDC to be linked with other datasets in the national data linkage system.
- NSW’s Lumos is a state-wide program linking GP data with public and private hospital admitted patient, non-admitted patient, ambulance, cancer and cause of death data. Data linkages are performed twice per year, and after each linkage participating GPs and PHNs receive a customised report about their patients. As of October 2022, all NSW PHNs and more than 600 general practices were participating in Lumos. The program has been funded through the Commonwealth Health Innovation Fund (NSW Health 2022).
- The University of Melbourne, in partnership with general practices, has developed Data for Decisions, a collection of de-identified general practice data. In 2020, there were approximately 3.5 million de-identified patients in the dataset and around 80 million patient visits.
Next steps for perinatal mental health screening data
Evidence about perinatal mental health is essential to inform the development and evaluation of policies and to help plan, deliver and coordinate targeted services and initiatives. Perinatal mental health data are currently disparate and fragmented, and this report highlights there is currently no single solution. To produce a meaningful national picture, a multipronged, iterative approach is needed that builds on existing systems and works in tandem with the delivery of quality health care.
The various data development initiatives described in this report will improve evidence about perinatal mental health in Australia. Amplified by Australian stories of perinatal mental health experiences, future reporting of state and territory efforts, including data gained from the PMHp and data linkage, will improve our picture of the needs of mothers and families, so they receive the mental health support they need.
Austin M, Mule V, Hadzi-Pavlovic D and Reilly N (2022) ‘Screening for anxiety disorders in third trimester pregnancy: a comparison of four brief measures’, Archives of Women's Mental Health, 25(2):389–397, doi:10.1007/s00737-021-01166-9.
Commonwealth of Australia (2022) The National Mental Health and Suicide Prevention Agreement, Australian Government, accessed 26 September 2023.
Council of Australian Governments (COAG) Health Council (2019) Woman-centred care: strategic directions for Australian maternity services, Department of Health, Australian Government, accessed 26 September 2023.
Highet NJ and Purtell CA (2012) The National Perinatal Depression Initiative: a synopsis of progress to date and recommendations for beyond 2013, Beyond Blue, accessed 26 September 2023.
New South Wales Ministry of Health (NSW Health) (2022) Lumos evaluation report 2: October 2022, Ministry of Health, New South Wales Government, accessed 26 September 2023.
Smith-Nielsen J, Egmose I, Wendelboe KI, Steinmejer P, Lange T and Vaever MS (2021) ‘Can the Edinburgh Postnatal Depression Scale-3A be used to screen for anxiety?’, BMC Psychology, 9(1):118, doi:10.1186/s40359-021-00623-5.


