Initial findings
This report describes initial insights from the implementation of data collection on mental health and family violence screening in Australia.
Mental health and family violence Perinatal NBEDS items
Queensland, Western Australia, Tasmania and the Australian Capital Territory (ACT) supplied antenatal mental health and family violence screening data for both the 2020 and 2021 birth cohorts.
This report focuses on antenatal EPDS screening status and score for the state and territory health authorities that contributed data for these items (Queensland, Tasmania and the ACT):
- Antenatal mental health risk screening status (Yes, Not offered, Declined)
- Indication of possible symptoms of depression at an antenatal care visit (total EPDS score).
Analysis has not been presented for the following data items:
- Presence or history of mental health condition indicator (Yes, No) - due to high levels of variation between state and territory health authorities and health services in the criteria used to record the data item. Standardising how data are collected for this item would improve its reliability as an indicator and enable further analysis.
- Family violence screening status (Yes, Not offered, Declined) - due to the small number of state and territory health authorities currently providing data for this data item.
Table 1: Overview of state and territory health authorities that supplied the mental health and family violence data items, 2020 and 2021
| Data item | Qld | WA | Tas | ACT | Per cent of mothers from supplying state and territory health authorities(a) with a stated result(c) (%) 2020 | Per cent of mothers from supplying state and territory health authorities(a) with a stated result(c) (%) 2021 | Per cent of all mothers(b) with a stated result(c) (%) 2020 | Per cent of all mothers(b) with a stated result(c) (%) 2021 |
|---|---|---|---|---|---|---|---|---|
Antenatal mental health risk screening status | ✓ | ✓ | ✓ | ✓ | 96.5% | 96.8% | 33.8% | 33.9% |
Indication of possible symptoms of depression at an antenatal care visit, total EPDS score | ✓ |
| ✓ | ✓ | 75.7% (99% of women with an Antenatal mental health risk screening status of ‘Yes’) | 75.3% (99% of women with an Antenatal mental health risk screening status of ‘Yes’) | 18.3% | 18.1% |
Presence or history of mental health condition indicator | ✓ |
| ✓ | ✓ | 100% | 100% | 24.1% | 24.0% |
Family violence screening status | ✓ |
| ✓ |
| 99.6% | 99.6% | 21.9% | 21.9% |
Notes:
- Supplying state and territory are indicated by the check mark for each item.
- All mothers includes all mothers from all states and territories in the NPDC.
- Stated results exclude mothers with ‘Unknown’, ‘Not stated/inadequately described’ or missing results. For instance, for the total EPDS item, stated results include a score of 0 to 30.
Source: AIHW analysis of the NPDC, 2020 and 2021.
Detailed information on completeness, accuracy and other aspects of data quality for the NPDC is in the data quality statement. Additional detail about the NPDC is in the Availability of perinatal data.
The AIHW continues to engage and consult with technical and subject matter experts from state and territory health authorities to determine next steps to improve the consistent collection of these data items. See Data opportunities for more information.
Initial findings – details
As part of the Perinatal NBEDS (NPDC), the AIHW received data for the data items Antenatal mental health screening status and Total EPDS score from Queensland, Tasmania and the ACT for 2020 and 2021, and found:
Of the 145,137 mothers who gave birth in these states and territories, 109,547 (75%) received antenatal mental health screening with a recorded EPDS score during their pregnancy.
- The remaining mothers were either not offered screening (20%), declined screening (0.7%), received antenatal mental health screening but did not have an EPDS score recorded (0.8%) or their screening status was not stated (2.7%).
Who was more likely to be screened?
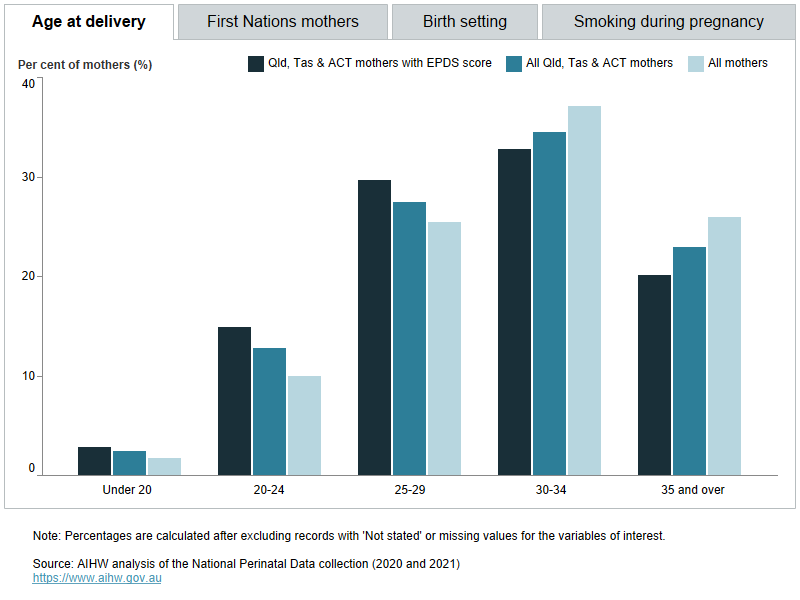
There were differences in some characteristics between women who had an EPDS score recorded and all women who gave birth.
- For example, compared with all mothers who gave birth in Queensland, Tasmania and the ACT, women with a recorded EPDS score were more likely to be aged under 25, give birth in a public hospital, report smoking at any point in their pregnancy, or were First Nations mothers.
Figure 2. Maternal and pregnancy characteristics of all mothers, mothers who gave birth in Queensland, Tasmania and the Australian Capital Territory, and mothers with an EPDS score, 2021 and 2022.
Who was more likely to be identified as at risk?
Overall, 7.6% of mothers with a recorded EPDS score were assessed as scoring 13 or above, indicating a high risk of depression and/or anxiety.
Of the women with a recorded EPDS score during their pregnancy:
- a higher proportion of mothers aged under 20 years scored 13 or above (20%), compared with 9.0% of mothers in their 20s, and 5.9% of mothers aged 30 and over
- a higher proportion of mothers who smoked at any point during pregnancy had a score of 13 or above (17%), compared with mothers who did not report smoking at any point (6.3%)
- a higher proportion of mothers who gave birth in public hospitals scored 13 or above (8.2%), compared with mothers who gave birth in a private hospital (3.9%)
- a higher proportion of mothers who had 3 or more previous live births scored 13 or above (9.9%), compared with 7.6% of first-time mothers and 7.2% of mothers who had 1-2 previous live births. A similar pattern was observed by parity with a higher proportion of mothers who had experienced 3 or more previous pregnancies scoring 13 or above (9.9%) compared with 7.6% of mothers experiencing pregnancy for the first time, and 7.2% of mothers who had experienced 1–2 previous pregnancies.
Birth outcomes for at-risk mothers
The causes of adverse pregnancy outcomes, such as stillbirth or pre-term birth, are complex. Adverse birth outcomes are associated with a range of factors that may also be associated with higher EPDS scores, including previous experience of trauma, complications during pregnancy, smoking, and social disadvantage. Associations between adverse birth outcomes and scores of 13 or above on the EPDS do not imply a causal relationship. Despite this, there may be an opportunity to further explore the relationship between birth outcomes, perinatal mental health screening results, and common contributing factors as more data become available.
In the data currently available, for women with a recorded EPDS score during their pregnancy:
- a higher proportion of mothers who subsequently had a pre-term birth (less than 37 weeks gestation) scored 13 or above during pregnancy (11.2%), compared with 7.4% of mothers who subsequently gave birth to their babies at term (37 to 41 weeks).
- a higher proportion of mothers who subsequently had a stillbirth scored 13 or above during pregnancy (11.8%), compared with 7.6% of mothers who had all live births for the pregnancy.
Interpreting the data
Scoring high on the EPDS is not a diagnosis of mental illness, it is an indication that the woman may have experienced depressive and/or anxiety symptoms in the past 7 days. Interpreting a high EPDS score as a diagnosis would likely overestimate antenatal depression prevalence (Lyubenova et al. 2021). The total EPDS score is one measure that clinicians can use to understand when women may be at heightened risk of poor mental health and may need further assessment, support and follow up. Similarly, factors associated with a higher EPDS score provide some insight into what cohorts of women may require more support through targeted services, policies or programs.
This report explores data from three states and territories who have implemented the perinatal mental health screening data items in the Perinatal NBEDS/NPDC. This report includes NPDC data for women giving birth in Queensland, Tasmania and the ACT only. This is the first perinatal mental health screening data to be assessed as being suitable for reporting, providing a case study to demonstrate the insights to be gained from reporting perinatal mental health screening data. Data from other state and territory health authorities will be available progressively as national implementation of the Perinatal NBEDS continues.
A higher proportion of women who had an EPDS score recorded had demographic and health factors which have been associated with a higher risk of perinatal depression, compared with all mothers in the three supplying state and territory health authorities and nationally. As such, results are not generalisable nationally.
Variation in EPDS response rates and scores may be due to a range of factors, such as the willingness of women to disclose their concerns and symptoms, and the cultural appropriateness of the EPDS for the woman. The NPDC also only collects data for one occasion of screening per woman, even if they were screened multiple times during pregnancy. Screening uptake and results may also have been affected by the COVID-19 pandemic shutdowns and service disruptions. However, the impact of the pandemic cannot be examined because the collection of these NPDC data items only began in 2020 and the date of screening is not collected.
See Key information gaps and Data opportunities for further information.
Lyubenova A, Neupane D, Levis B, Wu Y, Sun Y, He C, Krishnan A, Bhandari PM, Negeri Z, Imran M, Rice DB, Azar M, Chiovitti MJ, Saadat N, Riehm KE, Boruff JT, Ioannidis JPA, Cuijpers P, Gilbody S, Kloda LA, Patten SB, Shrier I, Ziegelstein RC, Comeau L, Mitchell ND, Tonelli M, Vigod SN, Aceti F, Barnes J, Bavle AD, Beck CT, Bindt C, Boyce PM, Bunevicius A, Chaudron LH, Favez N, Figueiredo B, Garcia-Esteve L, Giardinelli L, Helle N, Howard LM, Kohlhoff J, Kusminskas L, Kozinszky Z, Lelli L, Leonardou AA, Meuti V, Radoš SN, García PN, Pawlby SJ, Quispel C, Robertson-Blackmore E, Rochat TJ, Sharp DJ, Siu BWM, Stein A, Stewart RC, Tadinac M, Tandon SD, Tendais I, Töreki A, Torres-Giménez A, Tran TD, Trevillion K, Turner K, Vega-Dienstmaier JM, Benedetti A and Thombs BD (2021) ‘Depression prevalence based on the Edinburgh Postnatal Depression Scale compared to Structured Clinical Interview for DSM disorders classification: systematic review and individual participant data meta-analysis’, International Journal of Methods in Psychiatric Research, 30(1):e1860, doi:10.1002/mpr.1860


