Treatment
On this page:
What treatments do people receive?
Treatment in Australia
Many types of treatment are available in Australia, aiming to reduce the risk of harm associated with drug use through services such as counselling or information and education. For a subset of people who use alcohol and drugs, treatment and support will be required over the course of their life (consistent with dependence being a chronic condition, like asthma or diabetes). In many cases, people may require ongoing support to achieve long-term change. For other people, early support and treatment will be sufficient to reduce harms and prevent the need for further treatment or they may access treatment intermittently as required (Australian Government Department of Health and Aged Care 2019).
In 2022–23:
- A total of 235,461 treatment episodes were provided to people for their own or someone else’s alcohol or drug use.
- Treatment episode numbers increased by 30% since 2013–14 (from 180,783) and increased by 3.1% from the previous year (228,451 in 2021–22).
- Clients received an average of 1.8 treatment episodes nationally.
What are the treatment types?
Counselling continues to be the most common treatment provided.
In 2022–23:
- Counselling continued to be the most common main treatment type, comprising of just over 1 in 3 (34%) of all treatment episodes, followed by assessment only (22%) and support and case management (15%).
- Among people who received support for their own alcohol or drug use, around 1 in 3 (34%) episodes were for counselling and around 1 in 4 were for an assessment only (23%).
- Among people who received support for someone else’s drug use, over 2 in 5 (46%) episodes were for support and case management and around 1 in 3 (34%) were for counselling (Figure TREATMENT CLIENTS.1).
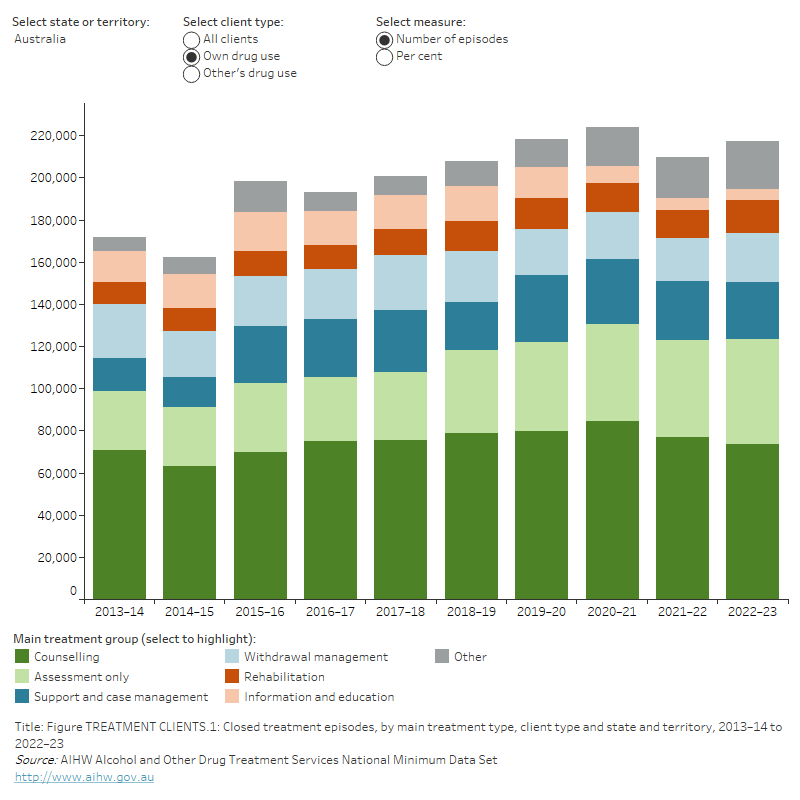
Figure TREATMENT CLIENTS.1: Closed treatment episodes, by main treatment type, client type and state and territory, 2013–14 to 2022–23
The stacked bar graph shows the closed treatment episodes for clients’ own drug use by main treatment type, client type and state and territory, from 2013–14 to 2022–23. Counselling has remained the most common treatment type in Australia in this time, with counselling being provided in 73,561 episodes (33.9%) for clients’ own drug use and 6,128 episodes (33.7%) for others’ drug use in 2022–23.
Among clients seeking treatment for their own drug use in Australia in 2022–23, assessment only (49,612 episodes, 22.8%), support and case management (27,357 episodes, 12.6%) and withdrawal management (23,250 episodes, 10.7%) were the next most common treatment types.
Among clients seeking treatment for their other’s drug use in Australia in 2022–23, support and case management (8,355 episodes, 46.0%), assessment only (1,255 episodes, 6.9%) and information and education (522 episodes, 2.9%) were the next most common treatment types.
Notes:
- 'Other' includes pharmacotherapy.
- Rehabilitation, withdrawal management (detoxification), and pharmacotherapy are not available for clients receiving treatment for someone else’s alcohol or other drug use.
- In 2019–20, changes were made to categories under Main Treatment – the word ‘only’ was removed from support and case management and information and education. The removal of the word ‘only’ from support and case management and information and education, changed reporting rules for agencies – allowing agencies to be able to report and more accurately capture these items as an additional treatment in conjunction with a main treatment type.
- The AODTS NMDS also collects data on a client's other treatment types, as well as main treatment type, however, this variable is not included in these data visualisations.
- South Australia reports a high proportion of Assessment only treatment episodes due to legislated client assessments under the state’s Police Drug Diversion Initiative and child protection programs.
- Data are subject to minor revisions over time.
- Components of tables may not sum to totals due to rounding.
Treatment delivery setting
2 in 3 treatment episodes were provided in a non-residential treatment setting.
Nationally, in 2022–23:
- Around 2 in 3 treatment episodes were provided in a non-residential treatment setting (66% of episodes), such as community-based Non-Government Organisations (NGOs) and hospital outpatient services.
- The next most common settings were residential treatment settings (16%), which allow clients to stay in a facility that is not their home or usual place of residence, other (7.3%) and outreach settings (6.5%) (such as mobile/outreach alcohol and other drug treatment service providers) (Figure TREATMENT DELIVERY.1).
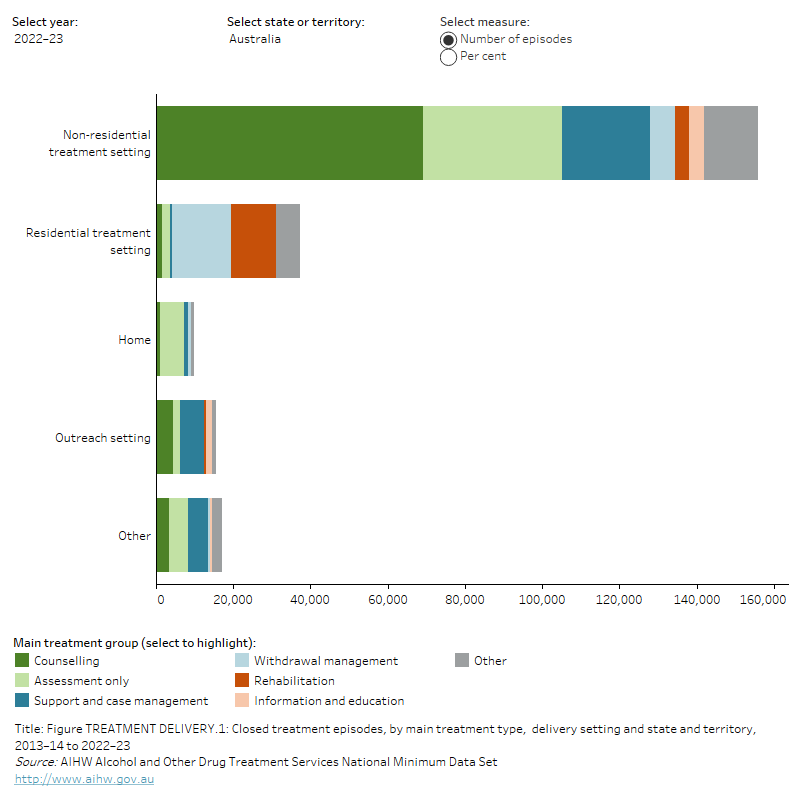
Figure TREATMENT DELIVERY.1: Closed treatment episodes, by main treatment type, delivery setting and state and territory, 2013–14 to 2022–23
The horizontal stacked bar graph shows the number of closed treatment episodes by main treatment type, delivery setting and state and territory. Most treatment episodes were delivered in non-residential treatment settings.
In 2022–23, the most common treatments by setting in Australia were: counselling (69,054 episodes, 44.3%) in non-residential settings; withdrawal management (15,264 episodes, 41.0%) was most common in residential settings; assessment only (6,083 episodes, 62.3%) in home settings; support and case management (6,048 episodes, 39.2%) in outreach settings; and support and case management (5,299 episodes, 30.8%) in other settings.
Notes:
- 'Other' includes pharmacotherapy.
- Rehabilitation, withdrawal management (detoxification), and pharmacotherapy are not available for clients receiving treatment for someone else’s alcohol or other drug use.
- In 2019–20, changes were made to categories under Main Treatment – the word ‘only’ was removed from support and case management and information and education. The removal of the word ‘only’ from support and case management and information and education, changed reporting rules for agencies – allowing agencies to be able to report and more accurately capture these items as an additional treatment in conjunction with a main treatment type.
- The AODTS NMDS also collects data on a client's other treatment types, as well as main treatment type, however, this variable is not included in these data visualisations.
- South Australia reports a high proportion of Assessment only treatment episodes due to legislated client assessments under the state’s Police Drug Diversion Initiative and child protection programs.
- Data are subject to minor revisions over time.
- Components of tables may not sum to totals due to rounding.
Length of treatment
Clients whose principal drug of concern was amphetamines spent one of the longest periods in treatment, with a median duration of 31 days.
In 2022–23, the median treatment duration across all treatment episodes was almost 4 weeks (27 days). The duration of treatment episodes varied by main treatment type and principal drug of concern:
- Among all treatment episodes, the median duration was 67 days for clients receiving counselling.
- For people who received support for their own alcohol or drug use, the median duration was 43 days for rehabilitation, 38 days for support and case management, 8 days for withdrawal management, and 3 days for an assessment only.
- Among treatment episodes for the four most common principal drugs of concern, median treatment duration was longest for amphetamines (31 days), followed by heroin (34 days), alcohol (27 days) and cannabis (24 days).
What are the common reasons for ceasing treatment?
In 2022–23, almost 3 in 5 (59%) of all treatment episodes ended in a planned or expected completion, and around 1 in 5 (19%) ended due to an unplanned completion (Figure REASON CESSATION.1).
Figure REASON CESSATION.1: Closed treatment episodes, by reason for cessation and main treatment, 2013–14 to 2022–23
The stacked bar graph shows closed treatment episodes, by reason for cessation and main treatment, 2013–14 to 2022–23. Expected/planned completion has consistently remained the most common reason for cessation for all treatments in this time, increasing from 116,147 episodes (64.2%) in 2013–14 to 138,671 episodes (58.9%) in 2022–23.
Ending due to unplanned completion has remained the next most common reason for cessation for all treatments, increasing from 36,360 episodes (20.1%) in 2013–14 to 45,826 episodes (19.5%) in 2022–23.

Notes:
- ‘Other’ includes pharmacotherapy.
- Rehabilitation, withdrawal management (detoxification), and pharmacotherapy are not available for clients receiving treatment for someone else’s alcohol or other drug use.
- In 2019–20, changes were made to categories under Main Treatment – the word ‘only’ was removed from support and case management and information and education. The removal of the word ‘only’ from support and case management and information and education, changed reporting rules for agencies – allowing agencies to be able to report and more accurately capture these items as an additional treatment in conjunction with a main treatment type.
- The AODTS NMDS also collects data on a client’s other treatment types, as well as main treatment type, however, this variable is not included in these data visualisations.
- South Australia reports a high proportion of Assessment only treatment episodes due to legislated client assessments under the state’s Police Drug Diversion Initiative and child protection programs.
- Data are subject to minor revisions over time.
- Components of tables may not sum to totals due to rounding.
Australian Government Department of Health and Aged Care 2019. National Framework for Alcohol, Tobacco and Other Drug Treatment 2019–29, Department of Health and Aged Care, Australian Government, accessed 6 March 2024.


