Policy framework
On this page:
Drug use in Australia
Alcohol and tobacco are 2 of the most widely used drugs in Australia. The most recent National Drug Strategy Household Survey 2022–2023 reported that of people aged 14 and over in Australia:
- 31% consumed an alcoholic drink in the previous 12 months
- 8.3% smoked tobacco daily.
About 1 in 3 (31% or 6.6 million) people aged 14 and over consumed alcohol in ways that put their health at risk according to the Australian Alcohol Guidelines (drinking more than 10 standard drinks per week on average or more than 4 standard drinks in a single day at least once a month; NHMRC 2020). This was similar to 2019, when 32% of the population (around 6.7 million people) reported drinking at risky levels (AIHW 2024a).
In 2022–2023, illicit drug use was relatively common among people aged 14 and over in Australia:
- 47% self-reported they had illicitly used a drug at some point in their life (including pharmaceuticals used for non-medical purposes) and 17.9% had done so in the last 12 months
- cannabis continued to be the most commonly used illicit drug with more than 1 in 3 (41%) having used it in their lifetime and 11.5% using it in the previous 12 months
- ecstasy and cocaine were the second and third most common illicit drugs used in a lifetime (13.6% and 13.5%, respectively) and in the last 12 months (2.1% and 4.5%, respectively) (AIHW 2024a).
Health impacts
The health impacts associated with alcohol and other drug (AOD) use include hospitalisation, mental health conditions, physical injury, overdose and mortality. Tobacco, alcohol and illicit drug use together account for 16.1% of the burden of disease in Australia (AIHW 2021).
Social impacts
The social impacts of AOD use in Australia include involvement in criminal activity, engagement in risky behaviours, victimisation and road trauma. In 2019, 1 in 5 (21%) people in Australia aged 14 and over were victims of an alcohol-related incident and 10.5% were victims of an illicit drug-related incident (AIHW 2020). This trend continued in 2022–2023, where 1 in 5 people (21%) aged 14 and over were victims of alcohol-related incidents and 1 in 10 people (10.1%) were victims of illicit drug-related incidents. Alcohol and illicit drug related incidents include verbal abuse, physical abuse, or being put in fear by someone under the influence of a substance in the previous 12 months (AIHW 2024).
Economic impacts
The use and misuse of licit and illicit drugs imposes a heavy financial cost on the Australian community. In recent years, the separate costs of tobacco ($136.9 billion in 2015–16), opioid ($15.76 billion in 2015–16), methamphetamine (over $5 billion in 2013–14) and alcohol use ($66.8 billion in 2017–18) in Australia have been estimated, utilising different methodologies (Whetton et al. 2021; Whetton et al. 2020; Whetton et al. 2019; Whetton et al. 2016).
The National Drug Strategy
Australia has had a coordinated approach to dealing with alcohol and other drugs since 1985. The National Drug Strategy (NDS) 2017–2026 is the 7th and latest iteration of the cooperative strategy between the Australian Government, state and territory governments, and the non-government sector. The NDS provides a framework that identifies national priorities relating to alcohol, tobacco and other drugs, guides action by governments – in partnership with service providers and the community – and outlines a national commitment to harm minimisation through balanced adoption of effective demand, supply, and harm reduction strategies.
The objective of the National Drug Strategy
The NDS has an overarching approach of harm minimisation and encompasses 3 pillars, each with specific objectives (NDSC 2017):
- demand reduction
- to prevent the uptake and/or delay the onset of use of alcohol, tobacco, and other drugs
- reduce the misuse of alcohol, tobacco, and other drugs in the community
- support people to recover from dependence through evidence-informed treatment
- supply reduction
- to prevent, stop, disrupt, or otherwise reduce the production and supply of illegal drugs
- to control, manage, and/or regulate the availability of illegal drugs
- harm reduction
- to reduce the adverse health, social and economic consequences of the use of drugs for consumers, their families, and the wider community.
The collection of treatment services data, for example in the Alcohol and Other Drug Treatment Services National Minimum Data Set (AODTS NMDS), forms part of the evidence base reinforcing harm reduction actions in the strategy, which include (NDSC 2017):
- increasing access to pharmacotherapy treatment to reduce drug dependence and reduce the health, social, and economic harms to individuals and the community that arise from misuse of opioids
- monitoring emerging drug issues to provide advice to the health, law enforcement, education, and social services sectors to inform individuals and the community regarding risky behaviours
- developing and promoting culturally appropriate alcohol, tobacco, and other drug information and support resources for individuals, families, communities, and professionals in contact with people at increased risk of harm from alcohol, tobacco, and other drugs
- providing opportunities for intervention among high-prevalence or high-risk groups and locations, including the implementation of settings-based approaches to modify risk behaviours
- enhancing systems to facilitate greater diversion into health interventions from the criminal justice system, particularly for Aboriginal and Torres Strait Islander people, young people, and other at risk populations who may be experiencing disproportionate harm.
Alcohol and other drug treatment services
AOD treatment services provide support to people regarding their use of alcohol or drugs through a range of treatments. Treatment objectives can include reduction or cessation of substance use, as well as improving social and personal functioning. Treatment and assistance may also be provided to support the family and friends of people who use alcohol or other drugs. Treatment services include detoxification and rehabilitation, counselling, and pharmacotherapy, and are delivered in residential and non-residential settings.
In Australia, publicly funded treatment services for AOD use are available in all states and territories. Most of these services are funded by state and territory governments, while some are funded by the Australian Government. Information on publicly funded AOD treatment services in Australia, clients, and drug treatment are collected through the AODTS NMDS. The AODTS NMDS is one of several national minimum data sets that collect data under the 2012 National Healthcare Agreement to inform policy and help improve service delivery (COAG 2012).
Other available data sources that support a more complete picture of AOD treatment in Australia include:
- the National Opioid Pharmacotherapy Statistics Annual Data collection
- the National Hospital Morbidity Database
- the Specialist Homelessness Services collection
- the National Prisoner Health Data collection.
The Alcohol and Other Drug Treatment Services National Minimum Data Set
The Alcohol and Other Drug Treatment Services National Minimum Data Set (AODTS NMDS) contains information on treatment provided to clients by publicly funded AOD treatment services, including government and non-government organisations. Information on clients and treatment services are included in the AODTS NMDS when a treatment episode provided to a client is closed (see Key terminology and glossary).
Information on the following types of treatment are reported:
- assessment only
- counselling
- information and education
- pharmacotherapy
- rehabilitation
- support and case management
- withdrawal management
- other (see Key terminology and glossary).
The AODTS NMDS collects data about services provided to people who are seeking assistance for their own alcohol or drug use and those seeking assistance for someone else’s alcohol or drug use.
Client information is collected at the episode level in the AODTS NMDS. Further details on the estimation of client numbers and the imputation methodology can be found in data and methods.
Data collected by treatment agencies are forwarded to the relevant state and territory health departments, who then extract required data according to the specifications in the AODTS NMDS. Data are submitted to the Australian Institute of Health and Welfare (AIHW) annually for national collation and reporting.
Coverage and data quality
Although the AODTS NMDS collection covers the majority of publicly funded AOD treatment services, including government and non-government organisations, it is difficult to fully quantify the scope of AOD services in Australia.
People receive treatment for alcohol and other drug-related issues in a variety of settings not in scope for the AODTS NMDS. These include:
- services provided by other not-for-profit organisations and private treatment agencies that do not receive public funding
- alcohol and other drug treatment units in acute care or psychiatric hospitals that provide treatment only to admitted patients
- prisons, correctional facilities and detention centres
- primary health-care services, including general practitioner settings, community-based care, Indigenous Australian-specific primary health-care services and dedicated substance use services
- health promotion services (for example, needle and syringe programs)
- accommodation services (for example, halfway houses and sobering-up shelters) (Figure AODTS1).
In addition, agencies whose sole function is prescribing or providing dosing services for opioid pharmacotherapy are excluded from the AODTS NMDS. These data are captured in the AIHW’s National Opioid Pharmacotherapy Statistics Annual Data collection.
Figure AODTS1: Alcohol and other drug treatment and support services in Australia
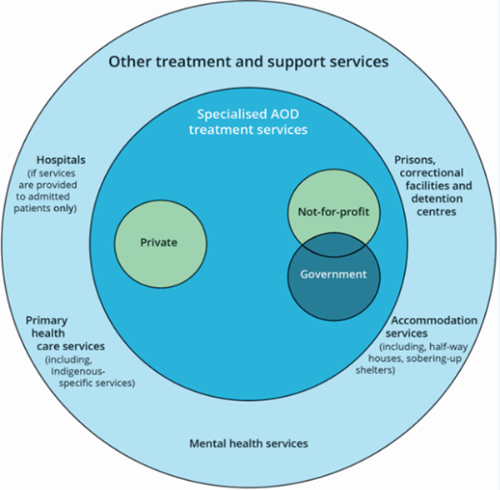
Note: Those in scope for the AODTS NMDS are shaded darker blue.
The Australian Government funds primary healthcare services and substance use services specifically for First Nations people. These services may be in scope for the AODTS NMDS but not all of the services currently report to the NMDS. These services previously reported via the Australian Government-funded First Nations substance use services, via the Online Services Report (OSR) data collection up to 2017–18 (AIHW 2024b). However, the substance use services program was transferred to the Indigenous Affairs Group within the Department of Prime Minister and Cabinet in September 2013 and then to the National Indigenous Australians Agency in July 2019 (Australian National Audit Office 2017, National Indigenous Australians Agency 2024). Since the cessation of substance use services data being collected by the OSR, the number of substance use services for First Nations people in-scope and reporting to the AODTS NMDS has gradually increased.
The National Agreement on Closing the Gap noted that funding for First Nations Alcohol and Other Drugs (AOD) services and support will increase by up to $66 million to 2024–25, in addition to current funding. First Nations’ AOD Treatment Services funded under the Indigenous Advancement Strategy (IAS) currently assists more than 65 providers to deliver AOD activities (Department of Prime Minister and Cabinet 2024). The Commonwealth also provides AOD treatment services and prevention, research and communication activities through the Drug and Alcohol Program (DAP) and funding to Primary Health Networks (PHNs), with nearly 30% of PHN funding allocated for First Nations specific treatment services (National Indigenous Australians Agency 2022).
In 2022–23, 95.6% (1,280) of in-scope agencies submitted data to the AODTS NMDS. Overall, from 2021–22 to 2022–23, there was a decrease of less than 1 percentage point (0.3%) in the proportion of in-scope agencies that reported to the collection. For the 2014–15 and 2015–16 reporting periods, sector reforms and system issues in some jurisdictions affected the number of in scope agencies that reported. This led to an under-count of the number of closed treatment episodes reported for these years, so results, especially across reporting years, should be interpreted with caution.
Further details on scope, coverage and data quality are available from the AODTS NMDS 2022–23 Data Quality Statement.
ANAO (Australian National Audit Office) (2017). Indigenous Advancement Strategy: Department of the Prime Minister and Cabinet, ANAO, Australian Government, accessed 6 March 2023.
AIHW 2020. National Drug Strategy Household Survey 2019: detailed findings. Drug Statistics series no. 32. Cat. no. PHE 270. Canberra: AIHW.
AIHW 2021. Australian Burden of Disease Study: Impact and causes of illness and death in Australia 2018. Cat. no. BOD 29. Canberra: AIHW. Viewed 9 March 2022.
AIHW 2024a. National Drug Strategy Household Survey 2022–2023 Cat. no: PHE 340 AIHW, Australian Government, accessed 29 February 2024.
AIHW 2024b. Online Services Report (OSR) for Aboriginal and Torres Strait Islander specific primary health care organisations, 2022–23; Quality Statement, AIHW METEOR Metadata Online Registry website, accessed 6 March 2024.
COAG (Council of Australian Governments) 2012. The National Health Reform Agreement. Canberra: COAG. Viewed 18 March 2022.
Department of Prime Minister and Cabinet (2024), Funding boost for First Nations Alcohol and Other Drug treatment services, Department of Prime Minister and Cabinet website, accessed 8 April 2024.
NDSC (National Drug Strategy Committee) 2017. National Drug Strategy 2017–2026. Canberra: Commonwealth of Australia.
NHMRC (National Health and Medical Research Council) 2020. Australian guidelines to reduce health risks from drinking alcohol. Canberra: Commonwealth of Australia.
NIAA (National Indigenous Australians Agency) (2022). Commonwealth Closing the Gap Annual Report 2022, NIAA, Australian Government, accessed 6 March 2023.
NIAA (2024). Our Business, NIAA, Australian Government, accessed 6 March 2024.
Whetton S, Shanahan M, Cartwright K, Duraisingam V, Ferrante A, Gray D, Kaye S, Kostadinov V, McKetin R, Pidd K, Roche A, Tait R, Allsop S 2016. The social costs of methamphetamine in Australia 2013/14. National Drug Research Institute, Curtin University, Perth, Western Australia.
Whetton S, Tait R, Scollo M, Banks E, Chapman J, Dey T, Abdul Halim S, Makate M, McEntee A, Muhktar A, Norman R, Pidd K 2019. Identifying the Social Costs of Tobacco Use to Australia in 2015/16. National Drug Research Institute, Curtin University, Perth, Western Australia. Viewed 22 October 2019.
Whetton S, Tait R, Chrzanowka A, Donnelly N, McEntee, Muhktar A, et al. 2020. Quantifying the social costs of pharmaceutical opioid misuse & illicit opioid use to Australia in 2015/16. National Drug Research Institute, Curtin University, Perth, Western Australia.
Whetton S, Tait R J, Gilmore W, Dey T, Agramunt S, Abdul Halim S, McEntee A, Mukhtar A, Roche A, Allsop S and Chikritzhs T (2021) Examining the social and economic costs of alcohol use in Australia: 2017/18, National Drug Research Institute, Curtin University, Perth, accessed 31 March 2022.


