Technical notes
Overarching methods
General methods for estimation of burden of disease can be found in Australian Burden of Disease Study: methods and supplementary material 2018 (AIHW 2021a). This includes descriptions for years of life lost (YLL), years lived with disability (YLD), disability-adjusted life years (DALY) and health-adjusted life expectancy (HALE).
How the Australian Burden of Disease Study 2022 differs from previous studies
The ABDS 2022 is different to the 2003, 2011, 2015 and 2018 studies in that estimates have been produced for the current year (2022). ABDS 2022 includes disease burden estimates for the year of release (2022) for 220 diseases and injuries, including estimates of burden from COVID-19 for the first time. This Study provides burden of disease estimates best matched to the public health context for the Australian population for 2022.
Calculation of estimates
Estimates for most diseases for 2022 were based on sex- and age-specific ABDS time series data between 2003 and 2019. To improve the robustness of trend analysis, 2019 estimates for YLD and YLL were calculated using 2018 methods and updated data where applicable (further described below). YLD and YLL were analysed separately.
2019 and earlier reference years
Estimates for YLD were calculated for 2019 to improve the robustness of trend analysis by using updated data where applicable. This included diseases which use key sources such as the National Hospital Morbidity Database and Australian Cancer Database. If it was determined that there would be no significant changes in 1 year (from 2018 to 2019), or where data were unavailable, rates from 2018 were applied to the 2019 population data. Estimates between 2003 and 2018 followed the methodologies developed for ABDS 2018 (AIHW 2021a).
ABDS 2022 used revised mortality data to calculate single-year estimates for YLL from 2011 to 2019 in the trend analysis to reflect changes in mortality coding under the ABS revisions process. ABS revises mortality information for coroner-certified deaths to improve the accuracy of the coding. These revisions do not increase the overall number of deaths in any particular processing year, but may change the distribution of the causes of death. Further information on the ABS mortality revisions process is available on the ABS website.
2022 estimates
The estimates for 2022 are largely based on trend analyses. Estimates of YLD for 2022 were based on ABDS time series data in 2003, 2011, 2015, 2018 and 2019. Updated source data were used where available, such as revised mortality data since the last ABDS.
For each disease, one of the following methods was used:
- log-linear regression (also called Poisson regression or Poisson linear regression)
- ordinary least-squares regression (also called simple linear regression)
- sex- and age-specific rates assumed to be the same between 2019 and 2022.
For some diseases, the reference period was restricted (i.e. 2011–2019). For example, years were excluded where data were considered inappropriate for use in trend analysis, such as due to coding changes, or data in early years were not robust. See Box 1 for examples of coding changes for selected diseases and how this affected trend analyses.
Substance use disorders and accidental poisoning
In 2014, the ABS implemented the use of new software for coding causes of death, applied International Classification of Diseases 10th revision (ICD-10) updates and reviewed coding practices. These processes impacted the cause of death output from 2013 onwards. Previously, for substance use disorders, where a death was due to an accidental drug overdose for a person with a known addiction to the drug, the addiction was reported as the underlying cause of death (that is, codes F10–F19 Mental and behavioural disorders due to psychoactive substance use). Since the coding changes, the drug overdose is captured as the underlying cause of death (X40–X49 Accidental poisoning) and the addiction is retained as an associated cause of death. The result was an increase in deaths due to Accidental poisoning, and a decrease in the number of deaths due to Mental and behavioural disorders due to psychoactive substance use. These changes will have an impact on comparisons made between 2003 or 2011 and 2015, 2018 or 2022, but not on those made between 2003 and 2011, or between 2015 and 2018 or 2022.
To account for the change in 2013, the 2022 projected estimates of fatal burden (YLL) of substance use disorders were based on trend analysis starting from 2013.
Dementia and stroke
The number of deaths due to dementia has increased when comparing data before 2006 with data from 2006 onwards. This increase can be attributed to (1) changes in ICD-10 instructions for coding deaths data, which have resulted in assigning some deaths to vascular dementia (F01) that may previously have been coded to cerebrovascular diseases (stroke) (I60–I69), and (2) legal changes allowing veterans and members of the defence forces to relate death from vascular dementia to relevant service. This, along with an accompanying promotional campaign targeted at health professionals, is thought to have increased the reported number of dementia deaths among this group (ABS 2014). These changes will have an impact on comparisons made between 2003 and 2011, 2015, 2018 or 2022, but not on those made between 2011 and 2015, 2018 or 2022.
To account for the change in 2006, the 2022 burden estimates (both YLL and YLD) for dementia and stroke were based on trend analysis starting from 2011.
Gestational diabetes
The International Association of the Diabetes and Pregnancy Study Groups (IADPSG) developed a new consensus guideline for the testing and diagnosis of gestational diabetes in 2010. In 2014, the endorsement of the IADPSG guidelines by the Australasian Diabetes in Pregnancy Society (ADIPS) resulted in a significant change to the practice of testing and diagnosing gestational diabetes in Australia (AIHW 2019). Reflecting international trends, Australian studies found increases in the number of women diagnosed with gestational diabetes following the introduction of the IADPSG guidelines between about 2010 and 2014, of 20% (Laafira et al. 2015), 35% (Moses et al. 2011) and 74% (Cade et al. 2019). A steep increase of the incidence of gestational diabetes was recorded from 2012–13 (AIHW 2019). These changes will have an impact on comparisons made between 2003 or 2011 and 2015, 2018 or 2022, but not on those made between 2003 and 2011, or between 2015 and 2018 or 2022.
To address this change, the 2022 non-fatal burden (YLD) estimates of gestational diabetes were based on trend analysis starting from 2015, which was the closest starting point amongst available ABDS estimates.
Two regression models were used to accommodate different annual patterns of diseases. The Poisson regression assumed that rates changed at a constant per cent annually, whereas the simple linear regression assumed a constant fixed amount of change (e.g. 10 YLD) every year (NCI 2022).
COVID-19 was added to the ABDS 2022 as a new disease. Lower respiratory infections (including influenza and pneumonia) were impacted by COVID-19, and estimates were derived using the most recent available data for 2022. Further details on these diseases, including caveats and assumptions, are presented below.
HALE
To calculate HALE, Sullivan’s method was used (see Jagger et al. 2014). Further information can be found in Australian Burden of Disease Study: methods and supplementary material 2018 (AIHW 2021a).
The life expectancy used to calculate HALE in 2022 was sourced from the 2018–2020 life table (ABS 2021). Life expectancy in Australia has generally increased over time, however, from exploratory analyses, a small decline in life expectancy for 2020–2022 is anticipated due to the impact of COVID-19, compared to the 2018–2020 life table. Lower than expected deaths occurred in 2020 and 2021 (ABS 2022b) and the expected gains in life expectancy for these years may offset the decline of life expectancy due to deaths from COVID-19 in 2022.
For other reference years, the 2016–2018 life table (ABS 2019) was used for 2018 HALE estimates, the 2013–2015 life table (ABS 2016b) was used for 2015 HALE estimates, the 2010–2012 life table (ABS 2013) was used for 2011 HALE estimates and the 2002–2004 life table (ABS 2005) was used for 2003 HALE estimates.
Estimation of COVID-19 for 2022
Fatal burden
Methods for calculating fatal burden (expressed as YLL) of COVID-19 used the number of deaths directly due to COVID-19, the ages at which these deaths occurred, and the Global Burden of Disease Study (GBD) standard reference life table.
Definition and coding of COVID-19 deaths
In the International Classification of Diseases 10th revision (ICD-10), COVID-19 deaths are coded in 2 ways:
- ICD-10 code U07.1 – COVID-19 virus identified is used when COVID-19 is confirmed by laboratory testing.
- ICD-10 code U07.2 – COVID-19 virus not identified is used for suspected or clinical diagnoses of COVID-19 where testing is not completed or inconclusive.
In ABDS 2022, deaths coded to U07.1 and U07.2 as the underlying cause of death (death directly due to COVID-19) were used to estimate fatal burden. At the time of analysis, the latest available data on COVID-19-related deaths were also used to inform the estimate.
Box 2: Defining COVID-19 deaths and COVID-19-related deaths
COVID-19 death (also called deaths due to COVID-19) is a death directly due to the SARS-CoV-2 virus.
COVID-19 related death (also called deaths with COVID-19) is a death where there is a disease or injury pathway to death that is not directly caused by the SARS-CoV-2 virus. For example, a person may have late stage cancer that has metastasised causing organ damage leading to death. This person may also have contracted COVID-19. While the virus may have negatively impacted health in an immuno-compromised person, the virus itself did not cause the terminal event leading to death (e.g. organ failure). In this example, the underlying cause of death would be cancer and COVID-19 would be considered an associated cause of death (ABS 2022a).
Data sources
COVID-19 deaths for 2022 were sourced from 2 key sources:
- Australian Bureau of Statistics (ABS) death registration data
This is the official Australian deaths data collected via the state/territory Registrars of Births, Deaths and Marriages. It includes death registration data and medical cause of death information completed by a certifying medical practitioner and is considered a high-quality data source. In early-mid 2020, the ABS started releasing provisional deaths data to monitor the impact of the COVID-19 pandemic. Further information about the completeness and timeliness of ABS provisional deaths data is available on the ABS website.
- National Notifiable Diseases Surveillance System (NNDSS) data
Data are collected by state and territory infectious disease surveillance systems and compiled into a national data source by the Australian Government Department of Health and Aged Care. Surveillance requires more timely data to enable a quicker public health response to outbreaks. Because it can be difficult to attribute a death to a single cause, particularly for people who have multiple and co-morbid conditions, the NNDSS reports deaths which include death in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID-19 (e.g. trauma).
Estimating fatal burden in 2022
Doctor-certified COVID-19 and COVID-19 related deaths between January and August 2022 were provided by the ABS. The COVID-19 associated deaths between January and August 2022 were extracted from published data on the NNDSS website.
As the ABS data were incomplete for August 2022, data from the NNDSS were used to inform the number of COVID-19 deaths for this month. The monthly changes of COVID-19 deaths were calculated from the NNDSS and applied to ABS data to derive the number of COVID-19 deaths for August. The COVID-19 deaths for the remainder of 2022 were modelled with an assumption of a gradual decline to December. The total number of deaths was inflated by 2.5% to account for coroner-certified COVID-19 deaths.
The estimated COVID-19 deaths for 2022 were disaggregated by age and sex, using the age and sex distributions from the provisional deaths provided by the ABS. The standard reference life table was then applied to the estimates to derive the YLL at each age.
Non-fatal burden
Conceptual model
The conceptual model for COVID-19 is shown in Figure 1, which was the consensus model being used by the European Burden of Disease Network (EBDN) to calculate non-fatal burden due to COVID-19 at the time of analysis. Important components of the YLD model which acquire health loss (Figure 1) include:
- Mild/moderate cases: correspond to those not requiring hospitalisation to treat their disease. It is noted that some cases in Australia were hospitalised to maintain strict isolation rather than because of the severity of their disease (particularly at the start of the pandemic).
- Severe cases: correspond to those hospitalised to treat their disease, but not requiring admission to intensive care units (ICU).
- Critical cases: correspond to people who were treated in ICU.
- Post-acute consequences: correspond to cases with post COVID-19 condition (also known as ‘long COVID’). Evidence is still emerging on this so a simple model was adopted for this Study. A more detailed model may be developed in the future as more data become available.
Permanent functional impairment from COVID-19 was not included in this Study due to a lack of evidence. More elapsed time is needed to understand these potential consequences.
Figure 1: Conceptual model for COVID-19 burden of disease analysis
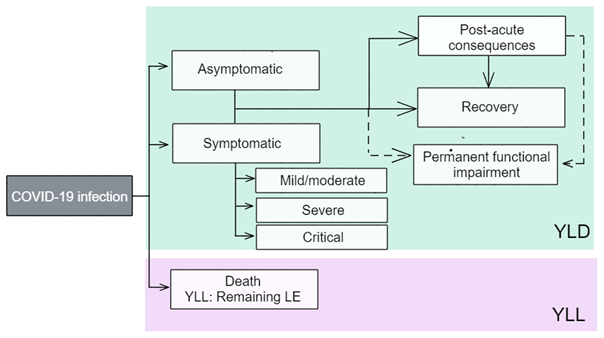
LE = life expectancy; YLD = years lived with disability; YLL = years of life lost.
Source: EBDN 2020.
Model parameters: disability weights and disease durations
The ‘disability weights’ reflect the severity of the disease and correspond to a ‘health state’ which describes the average experience for people at that severity level. As is the usual approach in the ABDS, the use of GBD disability weights was prioritised. However, an additional disability weight (for critical cases) sourced from the European Disability Weight survey (Haagsma et al. 2015) was used as no corresponding disability weight was available from the GBD at the time of analysis.
Table 1 outlines the disability weights for each health state. The disability weights were drawn from EBDN 2020.
It is important to note that in this Study:
- Asymptomatic cases have no disability weight as these cases are considered to have no health loss. The possible burden of isolation and worry of potential transmission to family members is not counted.
- The model may change in future studies as more evidence and data on COVID-19 and long COVID emerge. The AIHW continues to liaise with the COVID-19 Epidemiology and Surveillance Team at the Department of Health and Aged Care and the EBDN, as well as review other sources (for example, GBD) and assess international developments in the model for long COVID.
Table 1: Health states and corresponding disability weights for COVID-19 analysis
| Health state type | Severity level | Health state | Disability weight |
| Acute infectious disesase | Asymptomatic | Has infection but experiences no symptoms | Nil |
| Mild/moderate | Has a fever and aches, and feels weak, which causes some difficulty with daily activities | 0.051 | |
| Severe | Has a high fever and pain, and feels very weak, which causes great difficulty with daily activities | 0.133 | |
| Critical | Intensive care unit admission | 0.655 | |
| Chronic infectious disease | Post-acute consequences | Is always tired and easily upset, the person feels pain all over the body and is depressed. | 0.219 |
The duration used for mild/moderate cases was 7 days due to the shorter duration of Omicron infection, which was the dominant variant in Australia in 2022 (Menni et al. 2022). The duration parameters for severe and critical cases are based on empirical data on average length of stay from the National Hospital Morbidity Database (NHMD), using the period from 1 July 2020 to 30 June 2021, which were the latest available data from the NHMD at the time of analysis. It was assumed that the same durations would apply for those hospitalised due to COVID-19 in 2022. Hospitalisations without an ICU admission are used for severe cases, and those with ICU admission for critical cases. Median length of stay for critical cases only includes time spent in ICU—their time spent outside of the ICU is counted under the median length of stay for severe cases.
The average duration parameter used for post-acute consequences is 4 months, corresponding to a third of a year (GBD Long COVID Collaborators 2022). This is a broad assumption as data on the full trajectory for people with long COVID are still emerging.
Data sources
Broadly, the number of people in each severity category were required. Ideally, this would be from national data sets, but where there were data gaps, state/territory level data were used and adjustments made for national analysis.
The input data needed to reflect the full coverage of cases, with any under-ascertainment adjusted for with appropriate data, if available. Under-ascertainment for COVID-19 is becoming a bigger issue as time goes on due to the move from close contact tracing and strict requirements for PCR-based testing, to rapid antigen testing and reliance on self-reporting. Under-ascertainment is discussed further in each severity category.
Asymptomatic cases
An AIHW COVID-19 report (AIHW 2021b) used figures from a meta-analysis (Byambasuren et al. 2020) to estimate the proportion of asymptomatic COVID-19 cases. This showed that 17% of cases were truly asymptomatic (for example, excludes pre-symptomatic cases). However, this review was conducted in 2020 and due to the emergence of newer variants and sub-variants, higher vaccination rates and changes in requirements for COVID-19 testing in 2022, it is likely this proportion is no longer suitable.
As no data on asymptomatic cases were available, it was assumed that the NNDSS only includes symptomatic cases and the inclusion of asymptomatic cases is minimal in estimates of mild/moderate cases.
Mild/moderate cases
This was calculated as the total number of confirmed cases recorded in the NNDSS.
Under-ascertainment would be highest in the mild/moderate category. Given the lower severity (and hence lower contribution per case to the disease burden) in this category and challenges with adjusting for under-ascertainment with currently available data, there was not enough information to inform adjustments for under-ascertainment in this Study. There are serosurvey studies that measure the prevalence of antibodies to SARS-CoV-2 in the blood donor population (e.g. the National Centre for Immunisation Research and Surveillance, the Kirby Institute’s Australian COVID-19 Serosurveillance Network serosurveys). However, the blood donor population may not be representative of the general Australian population.
Severe and critical cases
The number of severe cases are the number of cases admitted to hospital minus those admitted to ICU. This was calculated by applying the proportion of cases that were admitted to hospital but not in ICU (sourced from the NNDSS) to the total number of COVID-19 cases. Age distributions were from published COVID-19 reports by NSW Health.
Critical cases are the number of cases admitted to ICU. This was calculated by applying the proportion of ICU admissions obtained from the NNDSS to the total number of COVID-19 cases. Similar to the estimates for severe cases, age distributions were from multiple published NSW COVID-19 reports (NSW Health 2022).
It is assumed that there would be virtually no under-ascertainment among the severe and critical categories as it is unlikely that people who require hospital care would not receive that care in Australia. People admitted would almost certainly have been tested for SARS-CoV-2 if there was any chance they had contracted it.
As there may be people who contracted COVID-19 in hospital (but did not suffer from severe or critical disease), identification of these cases in the data would be useful for burden estimation when more detailed hospitals data become available. However, it is acknowledged that because these cases cannot be identified, it may result in an overestimate of the burden due to severe COVID-19 (though an underestimate of mild/moderate cases).
It was assumed that in 2022, the number of cases who were admitted to hospital for isolation purposes rather than treatment was minimal.
Post-acute consequences
Australian data on this cohort are becoming more available (Darley et al. 2021; Liu et al. 2021). However, there was still no standard definition and set of symptoms for long COVID at the time of analysis and reporting. For the ABDS 2022, a proportion of 4.5% (for those aged 25 years and older) and a proportion of 1.44% (for those aged under 25 years) were used to estimate the number of cases who developed post-acute consequences from their COVID-19 infection. The proportion for those aged 25 years and over was sourced from the study by Antonelli et al. (2022) and was the proportion of Omicron cases who experienced long COVID. This proportion was not used for those aged under 25 years as there is evidence showing the likelihood of getting long COVID in younger age groups is lower (GBD Long COVID Collaborators 2022). The proportion for those aged under 25 years was based on the estimated percentage of people under 25 years living in private households with self-reported long COVID of any duration in the UK. This proportion was based on the UK Coronavirus (COVID-19 Infection Survey) data for the 4-week period ending 3 September 2022 (ONS 2022).
Estimating non-fatal burden in late 2022
NNDSS data were available for 1 January to 31 August 2022. Hospital proportions were derived from data for the same period. Similar to estimating fatal burden from COVID-19, non-fatal burden was estimated using monthly trends in case numbers. It was assumed that there was an exponential decline in the number of cases from September to December 2022. As described above, proportions from the NNDSS and from Antonelli et al. (2022) were applied to the total number of COVID-19 cases for 2022 to estimate the point prevalence of acute infection of COVID-19 by severity and post-acute consequences of COVID-19. However, this assumes that any trend in the number of cases at the time of analysis will continue for the remainder of the year. If there are any marked changes in COVID-19 cases and deaths in Australia later in the year, estimates for 2022 will be revised in the next study.
Estimation of lower respiratory infections (including influenza and pneumonia) for 2022
Fatal burden
Deaths due to lower respiratory infections (LRIs), including influenza and pneumonia, were sourced from the ABS death registration data and the Australian Influenza Surveillance Reports. The Australian Influenza Surveillance Reports are compiled from a number of data sources, including laboratory-confirmed notifications to the NNDSS; influenza-associated hospitalisations; sentinel influenza-like illness (ILI) reporting from general practitioners; ILI-related community level surveys; and sentinel laboratory testing results. See Department of Health and Aged Care for more information.
Deaths for 2022 were first estimated for fatal burden calculations and were derived separately for LRIs and influenza. Provisional doctor-certified deaths by month and age groups from January to June 2022 were provided by the ABS and used as death estimates for the first 6 months of 2022. Doctor-certified deaths were estimated for July to December 2022 using various methods. For LRIs, monthly deaths from the Australian Influenza Surveillance Reports were compared with the ABS provisional deaths data supplied. The proportional differences were used to adjust the deaths in July and August reported in the Australian Influenza Surveillance Reports.
For the remainder of 2022, the pattern of monthly doctor-certified deaths in 2019 were used to inform the proportional increase (or decrease) of deaths from one month to the next month.
Using deaths between 2011 and 2019 from the National Mortality Database, we derived the average inflation factor from all deaths to doctor-certified deaths for LRIs and influenza. This factor was applied to the number of doctor-certified deaths estimated for 2022.
The age distribution from the provisional deaths provided by the ABS were applied to the total number of deaths estimated for 2022. The standard reference life table was then applied to the estimates to derive the YLL at each age.
Non-fatal burden
Conceptual models
Lower respiratory infections (LRIs, including pneumonia)
The following disease model forms the conceptual basis for modelling YLD calculations for LRIs, including the sequelae, health states and disability weights.
Figure 2: Conceptual model for lower respiratory infections
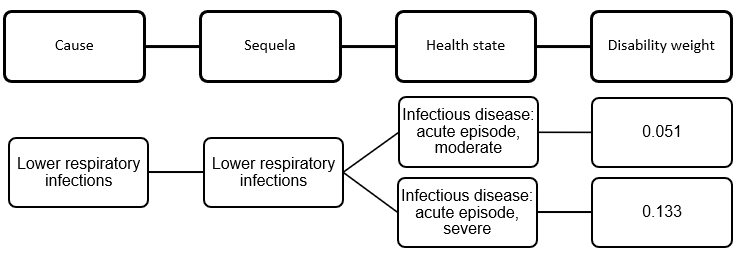
A duration of 2 weeks was used for both health states to estimate point prevalence.
Influenza
The following disease model forms the conceptual basis for modelling YLD calculations for influenza, including the sequelae, health states and disability weights.
Figure 3: Conceptual model for influenza
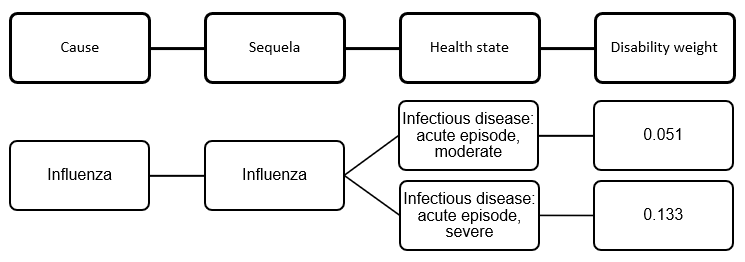
A duration of 2 weeks was used for both health states to estimate point prevalence.
Data sources from ABDS 2018
For the ABDS 2018, the following data sets were used for estimating burden from LRIs (including pneumonia) and influenza:
- The Bettering the Evaluation and Care of Health (BEACH) program data were used to estimate the total incidence of LRIs (including pneumonia) and influenza, accounting for the moderate severity in each of the above conceptual models. As the BEACH program last published data for 2016, disease rates for that year were applied to the 2018 population. Influenza is notifiable in all states and territories. However, notifications are ‘strongly influenced by the healthcare seeking behaviour of patients, testing, notification practices and follow-up by jurisdictional health departments’ (Li-Kim-Moy et al. 2016). Notifications are likely to be a significant underestimate of influenza incidence.
- The incidence of severe cases of LRIs and influenza were sourced from the National Hospital Morbidity Database (NHMD). The latest data available for the NHMD are for 1 July 2020 to 30 June 2021.
Influenza
For the ABDS 2022, national notifications information published by the Australian Department of Health and Aged Care (DHAC 2022) were used to explore trends in influenza between 2017 and 2022. Based on this, it was assumed that the overall number of influenza cases in 2022 will be similar to 2017 and 2019. There are some limitations with this assumption. Firstly, the degree of under-ascertainment in influenza notifications data in 2017 and 2019 is unknown. The degree of under-ascertainment may also change from year to year depending on factors such as testing rates and severity of disease for that year.
With this assumption, severe influenza point prevalence estimates for 2022 were modelled using patterns from 2017 and 2019 hospitalisations—2018 hospitalisations were excluded since hospitalisations in that year were considerably lower than 2017 and 2019. Moderate influenza point prevalence for 2022 was then modelled using the ratio of moderate point prevalence to severe point prevalence in 2019.
Lower respiratory infections (including pneumonia)
There were no national data on incidence of LRIs for 2022 at the time of analysis. However, it was observed that hospitalisations for LRIs were stable between 2017 and 2019. It was assumed that hospitalisations for 2022 would be similar to the hospitalisation trends between 2017 and 2019 following the reduction in public health measures from COVID-19, which had resulted in lower hospitalisations due to LRI in 2020 and 2021.
With this assumption, severe LRI point prevalence estimates for 2022 were modelled using patterns in hospitalisations from 2017, 2018 and 2019. Moderate LRI point prevalence for 2022 was then modelled using the ratio of moderate point prevalence to severe point prevalence in 2019.
Estimating non-fatal burden in late 2022
As the ABDS 2022 is estimating disease burden in the same year as publication, there are a number of months of the year where burden estimates needed to be modelled. As outlined above, it was assumed that the overall estimate for the calendar year 2022 would be similar to 2017–2019 for LRIs and to 2017 and 2019 for influenza.
Population data
Population data were used to derive rates in this report. The Australian population data between 2015 and 2019 were sourced from rebased ABS Estimated Resident Population (ERP) (released on 27 June 2017) (ABS 2017). Population data between 2003 and 2011 were sourced from final population estimates from the 2011 Census (released 15 December 2016) (ABS 2016a).
Population data for 2022 were sourced from population projections by the Centre for Population (2021). At the time of analysis, these data were the only available source which factored in the early impacts of the COVID–19 pandemic on Australia’s population. The components of the population projection included population growth, net overseas migration and natural increase, with assumptions made regarding migration, mortality, and fertility rates (Centre for Population 2021). The population ‘Central scenario’ was used for this Study. This scenario assumed that the COVID-19 pandemic has significantly impacted the net migration in Australia in 2020–2021.
YLD data quality
The burden estimates for ABDS 2022 were largely based on trend analyses. The quality of input estimates in the ABDS 2022 for earlier reference years (2003, 2011, 2015 and 2018) are the same as the quality presented in the ABDS 2018. The ABDS 2018 estimates were produced using the best data available within the scope and time frame of the study. To provide information on the quality of estimates, a quality index was developed to rate estimates according to the relevance and quality of source data, and methods used to transform data into a form required for analysis. Generally, the higher the rating, the more relevant and accurate the estimate.
Fatal burden (YLL) estimates were considered to have the highest rating for both data and methods used, whilst non-fatal burden (YLD) estimates varied depending on the disease or injury, and the data sources used.
Information about the quality of the YLD 2018 estimates and the data and methods used can be found in Appendix B in the Australian Burden of Disease Study: impact and causes of illness and death in Australia 2018 report and in the Australian Burden of Disease Study: methods and supplementary material 2018 report.
For the first time, COVID-19 was added to the ABDS 2022 as a new disease. Lower respiratory infections (including influenza and pneumonia) were adjusted using recent data due to available evidence that these diseases were impacted by COVID-19. To help users understand the potential sources of uncertainty associated with the estimates, the 2-dimensional index developed for the burden estimates was used for these 2 diseases. This index was derived based on:
- the relevance of the underlying epidemiological data
- the methods used to transform that data into a form required by this analysis.
The quality of COVID-19 and lower respiratory infections (including influenza and pneumonia) are discussed below.
COVID-19
Estimates for COVID-19 are considered to be of somewhat reasonable quality. Data sources were considered relevant as they were broadly derived from the NNDSS. However, the estimates for post-acute consequences of COVID-19, which is the biggest contributor to non-fatal burden, were calculated using 2 proportions (one proportion for those aged under 25 years and another for those aged 25 years and over) so substantial modelling was done to estimate burden by sex and 5-year age groups. Estimates also needed to be modelled for the last 4 months of the year, which relied on the assumption that the current decreasing trend in number of cases will continue for the remainder of the year. Therefore, estimates must be used with caution.
Data score = D
Method score = D
Lower respiratory infections (including influenza and pneumonia)
Estimates for LRIs are considered to be of reasonable quality. Modelling was based on assumptions that LRIs and influenza were similar to years before the COVID-19 pandemic. These assumptions may not hold once 2022 data are available. Therefore, estimates must be used with caution.
Data score = C
Method score = C
ABS (Australian Bureau of Statistics) (2005) Life tables, 2002–2004, ABS, accessed 1 July 2022.
ABS (2013) Life tables, 2010–2012, ABS, accessed 1 July 2022.
ABS (2014) Causes of death, Australia, 2012, ABS, accessed 8 September 2022.
ABS (2016a) Australian demographic statistics, Jun 2016, ABS, accessed 8 September 2022.
ABS (2016b) Life tables, 2013–2015, ABS, accessed 1 July 2022.
ABS (2017) Australian demographic statistics, Dec 2016, ABS, accessed 8 September 2022.
ABS (2019) Life tables, 2016–2018, ABS, accessed 1 July 2022.
ABS (2021) Life tables, 2018–2020, ABS, accessed 1 July 2022.
ABS (2022a) COVID-19 mortality in Australia: deaths registered until 30 September 2022, ABS, accessed
21 November 2022.
ABS (2022b) Provisional mortality statistics methodology, ABS, accessed 21 September 2022.
AIHW (Australian Institute of Health and Welfare) (2019) Incidence of gestational diabetes in Australia, AIHW, accessed 8 September 2022.
AIHW (2021a) Australian Burden of Disease Study: methods and supplementary material 2018, AIHW, accessed
29 August 2022.
AIHW (2021b) The first year of COVID-19 in Australia: direct and indirect health effects, AIHW, doi:10.25816/phdn-x648.
Antonelli M, Capdevila Pujol J, Spector TD, Ourselin S and Steves CJ (2022) ‘Risk of long COVID associated with delta versus omicron variants of SARS-CoV-2’, The Lancet 399(10343):2263–64, doi:10.1016/S0140-6736(22)00941-2.
Byambasuren O, Cardona M, Bell K, Clark J, Mclaws ML and Glasziou P (2020) ‘Estimating the extent of asymptomatic COVID-19 and its potential for community transmission: systematic review and meta-analysis’, Official Journal of the Association of Medical Microbiology and Infectious Disease Canada 5:223–34, doi:10.3138/jammi-2020-0030.
Cade TJ, Polyakov A and Brennecke SP (2019) ‘Implications of the introduction of new criteria for the diagnosis of gestational diabetes: a health outcome and cost of care analysis’, BMJ Open 9:e023293, doi:10.1136/bmjopen-2018–023293.
Centre for Population (2021) Population statement, Centre for Population, accessed 16 August 2022.
Darley DR, Dore GJ, Cysique L, Wilhelm KA, Andresen D, Tonga K, Stone E, Byrne A, Plit M, Masters J, Tang H, Brew B, Cunningham P, Kelleher A and Matthews G (2021) ‘Persistent symptoms up to four months after community and hospital-managed SARS-CoV-2 infection’, Medical Journal of Australia 214(6): 279–80, doi:10.5694/mja2.50963.
DHAC (Department of Health and Aged Care) (2022) Australian Influenza Surveillance Report – No 12 – fortnight ending 11 September 2022, DHAC, accessed 27 October 2022, https://www1.health.gov.au/internet/main/publishing.nsf/Content/ozflu-surveil-no12-22.htm.
EBDN (European Burden of Disease Network) (2020) Burden of disease of COVID-19: protocol for country studies, EBDN, accessed 3 February 2021, https://www.burden-eu.net/docs/covid19-bod-protocol.pdf.
GBD (Global Burden of Disease Study) Long COVID Collaborators (2022) ‘Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021’, JAMA, doi:10.1001/jama.2022.18931.
Haagsma JA, de Noordhout CM, Polinder S, Vos T, Havelaar AH, Cassini A, Devleesschauwer B, Kretzschmar ME, Speybroeck N and Salomon JA (2015) ‘Assessing disability weights based on the responses of 30,660 people from four European countries’, Population Health Metrics 13:10, doi:10.1186/s12963-015-0042-4.
Jagger C, Van Oyen H and Robine J (2014) Health expectancy calculation by the Sullivan method: a practical guide (4th edition), Institute for Ageing, Newcastle University, accessed 12 September 2022, http://www.eurohex.eu/pdf/Sullivan_guide_pre%20final_oct%202014.pdf.
Laafira A, White SW, Griffin CJ and Graham D (2016) ‘Impact of the new IADPSG gestational diabetes diagnostic criteria on pregnancy outcomes in Western Australia’, Australian and New Zealand Journal of Obstetrics and Gynaecology 56(1):36–41, doi:10.1111/ajo.12394.
Li-Kim-Moy J, Yin JK, Patel C, Beard FH, Chiu C, Macartney KK and McIntyre PB (2016) ‘Australian vaccine preventable disease epidemiological review series: influenza 2006 to 2015’, Communicable Diseases Intelligence 40(4):E482–E495, https://www1.health.gov.au/internet/main/publishing.nsf/Content/cda-cdi4004-pdf-cnt.htm/$FILE/cdi4004f.pdf.
Liu B, Jayasundara D, Pye V, Dobbins P, Dore GJ, Matthews G, Kaldor J and Spokes P (2021) ‘Whole of population-based cohort study of recovery time from COVID-19 in New South Wales Australia’, The Lancet Regional Health Western Pacific 12(100193), doi:10.1016/j.lanwpc.2021.100193.
Menni C, Valdes AM, Polidori L, Antonelli M, Penamakuri S, Nogal A, Louca P, May A, Figueiredo JC, Hu C, Molteni E, Canas L, Österdahl MF, Modat M, Sudre CH, Fox B, Hammers A, Wolf J, Capdevila J, Chan AT, David SP, Steves CJ, Ourselin S and Spector TD (2022) ‘Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study’, The Lancet 399(10335): 1618–24, doi:10.1016/S0140-6736(22)00327-0.
Moses RG, Morris GJ, Petocz P, San Gil F and Garg D (2011) ‘The impact of potential new diagnostic criteria on the prevalence of gestational diabetes mellitus in Australia’, Medical Journal of Australia 194(7):338–40, doi:10.5694/j.1326-5377.2011.tb03001.x.
NCI (National Cancer Institute) (2022) Linear or log-linear model, NCI, accessed 8 September 2022.
NSW Health (2022) NSW respiratory surveillance reports – COVID-19 and influenza, NSW Health, accessed
21 October 2022.
ONS (Office for National Statistics) (2022) Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 6 October 2022, ONS, accessed 12 October 2022.


