Clients with problematic drug and/or alcohol use
On this page
Key findings: Clients with problematic drug and/or alcohol use, 2021–22

There is a strong association between problematic alcohol or other drug use and experiences of homelessness (AIHW 2022). Problematic drug and/or alcohol use can be a pathway into homelessness or develop while experiencing homelessness (Robinson 2014; Johnson & Chamberlain 2008). It can lock people into homelessness and compound the effects of limited service engagement and increased social isolation.
Problematic alcohol or other drug use is related to several homelessness risk factors, including low socioeconomic status and family and domestic violence (Lalor 2020). Problematic drug and/or alcohol users are also at great risk of serious and preventable health issues and death, particularly those who are homeless (AIHW 2022). The Journeys Home project identified that people were more likely to have risky levels of alcohol and drug use, the longer they were homeless (Scutella et al. 2014).
The characteristics of people with problematic drug and/or alcohol use as well as their service use patterns and housing outcomes were different from the other client groups presented in this report. Clients with problematic drug and/or alcohol use over the age of 10 were more likely to be male, present to agencies alone and be homeless at first presentation compared with all SHS clients. They were also more likely to be returning clients and use support services to a greater extent.
Reporting clients with problematic drug and/or alcohol use in the Specialist Homelessness Services Collection (SHSC)
SHS clients aged 10 and over are considered to have problematic drug and/or alcohol use if, at the beginning of or during support, the client provided any of the following information:
- recorded their dwelling type as rehabilitation facility
- required drug or alcohol counselling
- were formally referred to the SHS agency from an alcohol and drug treatment service
- had been in a rehabilitation facility or institution during the past 12 months
- reported problematic drug, substance or alcohol use as a reason for seeking assistance or the main reason for seeking assistance.
The identification of clients with problematic drug and/or alcohol use may be current or recent; referring to issues at presentation, just prior to receiving support or at least once in the 12 months prior to support.
For more information see Technical notes.
In 2021–22:
- SHS agencies assisted more than 23,400 clients (aged 10 and over) with problematic drug and/or alcohol use, a decrease from around 27,200 in 2020–21 (Historical data table HIST.SUB).
- Clients with problematic drug and/or alcohol use represented 8.6% of all SHS clients. (Supplementary table CLIENTS.39).
Client characteristics
Figure SUB.1: Key demographics, clients with problematic drug and/or alcohol use, 2021–22
This interactive image describes the characteristics of the approximately 23,400 clients with problematic drug and/or alcohol use and received SHS support in 2021–22. The majority of clients were male, aged 25–44. A third were Indigenous. Victoria had the greatest number of clients and the Northern Territory had the highest rate of clients per 10,000 population. The majority of clients had previously been assisted by a SHS agency since July 2011. Most were experiencing homelessness at the beginning of support. Most were in major cities.

Presenting unit and Living arrangements
Most clients (89% or nearly 20,800) with problematic drug and/or alcohol use presented to services for assistance alone, higher than for all SHS clients (64%) (Supplementary tables CLIENTS.9 and CLIENTS.42). A further 7.3% (or around 1,700) of clients who were single with one or more children, which was much lower than the rate for all SHS clients (27%).
The living arrangements reported by SHS clients with problematic drug and/or alcohol use at the beginning of support were quite different from the overall SHS population and other client groups. In 2021–22 (Supplementary table CLIENTS.10):
- About 61% (or around 13,800) clients with problematic drug and/or alcohol use were living alone at the beginning of SHS support (Supplementary table CLIENTS.43), higher than the proportion for all SHS clients (32%) and other client groups, such as clients with disability (40%) and clients with a current mental health issue (47%).
- Comparatively fewer clients with problematic drug and/or alcohol use were living as one parent with child(ren) (11% or 2,600 compared with 34% of all SHS clients) (Supplementary table CLIENTS.10 and CLIENTS.43).
Selected vulnerabilities
Most clients with problematic drug and/or alcohol use face additional challenges which may make them more vulnerable to homelessness. The additional vulnerabilities presented here include family and domestic violence and/or a current mental health issue.
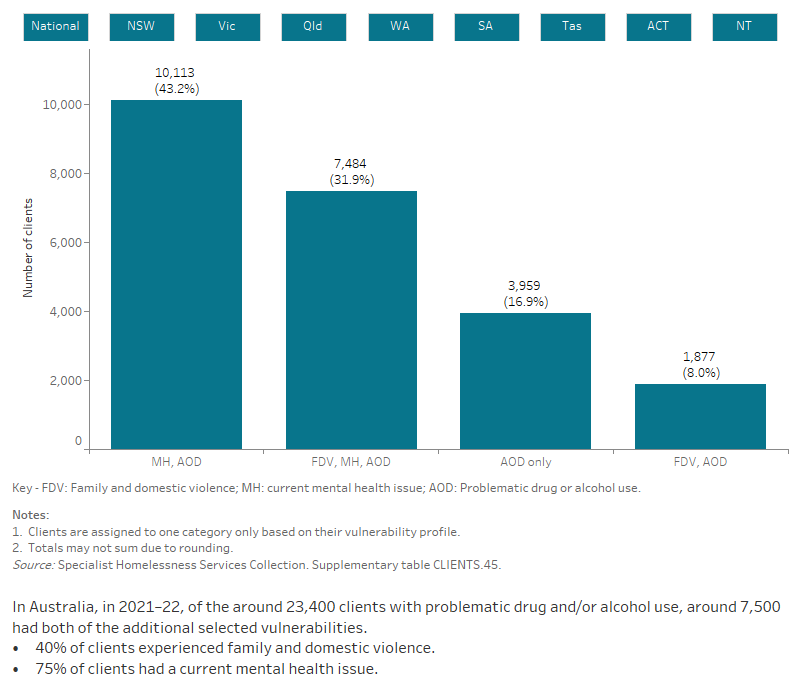
Figure SUB.2: Clients with problematic drug and/or alcohol use, by selected vulnerabilities, 2021–22
The interactive bar graph shows proportions of clients with problematic drug and/or alcohol use also experiencing additional vulnerabilities, including having a current mental health issue and problematic drug and/or alcohol use. The graph shows both the number of clients experiencing a single vulnerability only, as well as combinations of vulnerabilities, and presents data for each state and territory.
Service use patterns
The length of support provided to clients with problematic drug and/or alcohol use increased in 2021–22 to a median of 119 days, up from 86 days in 2017–18. The average number of support periods per client has been relatively consistent over time from an average of 2.9 support periods per client in 2018–19 to 3.0 in 2021–22.
The proportion of clients receiving accommodation has also been relatively stable at 50% in 2021–22, while the median number of nights accommodated increased from 40 in 2017–18 to 49 in 2021–22 (Supplementary table CLIENTS.46).
New or returning clients
In 2021–22 (Supplementary table CLIENTS.40):
- Clients with problematic drug and/or alcohol use were more likely to have received SHS services in the past (80% or almost 18,800 clients) than be new clients (20% or more than 4,600). That is, more clients had previously been assisted by a SHS agency at some point since the collection began in July 2011.
- Clients with problematic drug and/or alcohol use were more likely to be returning clients (80%) compared with other client groups; for example, compared with clients with a mental health issue (71%) and all SHS clients (63%). This may reflect the cyclical nature of insecure housing among people with problematic drug and/or alcohol use.
Main reasons for seeking assistance
In 2021–22, the main reasons clients with problematic drug and/or alcohol use presented to SHS agencies were (Supplementary tables SUB.5 and CLIENTS.22):
- housing crisis (19%, compared with 20% of the overall SHS population)
- inadequate/inappropriate dwelling conditions (15%, compared with 11%)
- family and domestic violence (13%, compared with 27%).
Few clients (4.1%) with problematic drug and/or alcohol use reported substance use issues as the main reason for seeking SHS assistance.
Services needed and provided
In 2021–22, the top 6 needs reported by SHS clients with problematic drug and/or alcohol use mainly related to housing and tenure (Supplementary table SUB.2).
Figure SUB.3: Clients with problematic drug and/or alcohol use, by services needed and provided, 2021–22
This interactive stacked horizontal bar graph shows the services needed by clients with problematic drug and/or alcohol use and their provision status. Advice/information was the most needed and most provided service. Long term housing was the least provided service.

Housing situation and outcomes
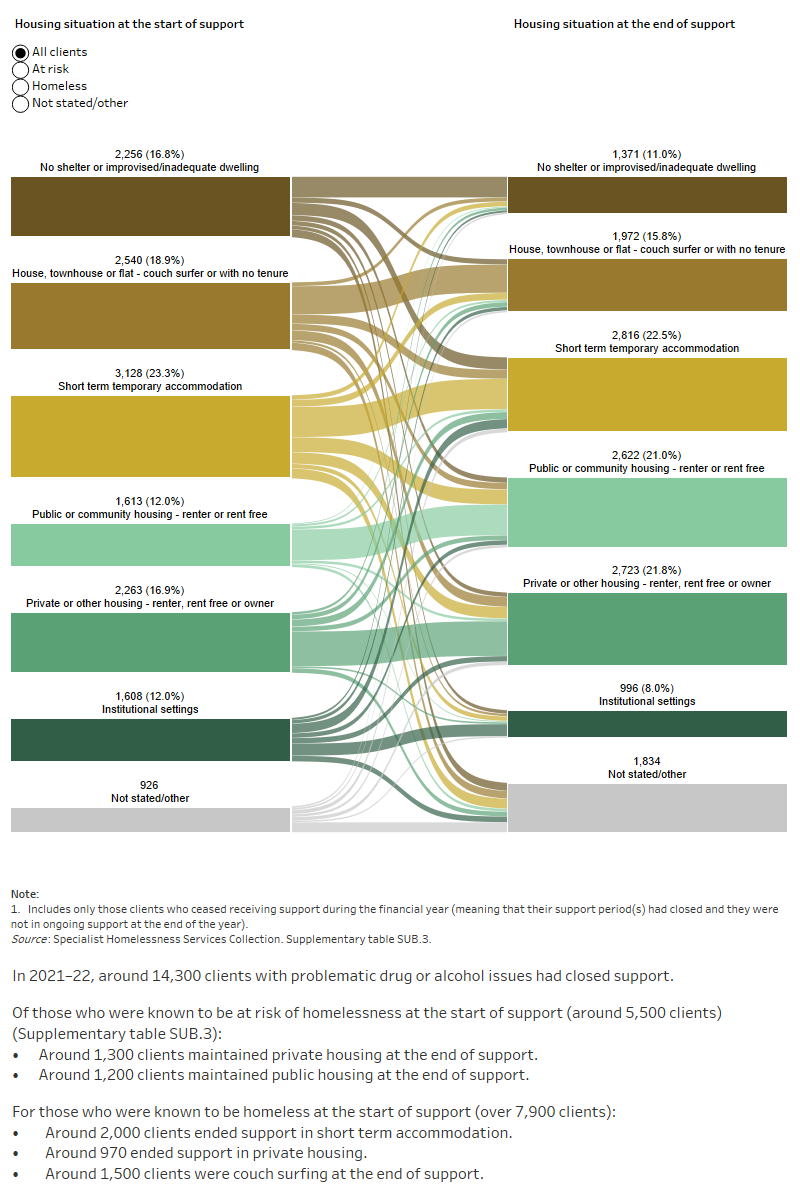
Outcomes presented here highlight the changes in clients’ housing situation at the start and end of support. That is, the place they were residing before and after they were supported by a SHS agency. The information presented is limited only to clients who have stopped receiving support during the financial year, and who were no longer receiving ongoing support from a SHS agency. In particular, information on client housing situations at the start of their first period of support during 2021–22 is compared with the end of their last period of support in 2021–22. As such, this information does not cover any changes to their housing situation during their support period.
While overall housing outcomes generally reflect trends towards more favourable housing, experiences of homelessness, particularly rough sleeping, were more common for clients with problematic drug and/or alcohol use both at the start and end of SHS support compared with other client groups.
For people with problematic drug and/or alcohol use in 2021–22, over half (59% or 7,900 clients) were experiencing homelessness at the start of support; nearly 2,300 (17%) had no shelter or were in an improvised/inadequate dwelling. By the end of support, 51% of clients were housed (Supplementary table SUB.3).
Figure SUB.4: Housing situation for clients with problematic drug or alcohol issues with closed support, 2021–22
This interactive Sankey diagram shows the housing situation (including rough sleeping, couch surfing, short term accommodation, public/community housing, private housing and Institutional settings) of clients with problematic drug and/or alcohol use with closed support periods at first presentation and at the end of support. The diagram shows clients’ housing situation journey from start to end of support. Most started and ended support experiencing homelessness, in short term accommodation.
Australian Institute of Health and Welfare (2022) Alcohol, tobacco & other drugs in Australia AIHW website, accessed 29 September 2022.
Johnson C and Chamberlain G (2008) Homelessness and substance abuse: which comes first?,Australian Social Work, 61(4), accessed 1 February 2018.
Lalor E (2020) Inquiry into Homelessness in Victoria: Submission to Legal and Social Issues Committee Legislative Council Parliament of Victoria North Melbourne, Vic: Alcohol and Drug Foundation.
Robinson C (2014) ‘Trauma: A cause and consequence of homelessness’, in Chamberlain C, Johnson G and Robinson C (eds.) Homelessness in Australia, NewSouth Publishing, Sydney, NSW.
Scutella R, Chigavazira A, Killackey E, Herault N, Johnson G, Moshcion J and Wooden M (2014) Findings from Waves 1 to 4: Special Topics, Journeys Home Research Report No. 4, report to the Australian Government Department of Social Services, Melbourne Institute of Applied Economic and Social Research, Melbourne.


