This article focuses on the use of lower prevalence illicit drugs such as ketamine and inhalants. In-depth reports are available for marijuana/cannabis, cocaine, ecstasy, methamphetamine and amphetamine, and hallucinogens, as well as non‑medical use of pain-relievers and opioids, and pharmaceutical stimulants .
Use of ketamine continued to grow in 2022–2023
While use of ketamine was stable between 2004 and 2016 (when around 70,000 people in Australia had used it in the previous 12 months), it has increased substantially since 2016 (Figure 1). In 2022–2023, 1.4% of the population (or around 300,000 people) had used ketamine in the previous 12 months, and around 900,000 people had used it in their lifetime.
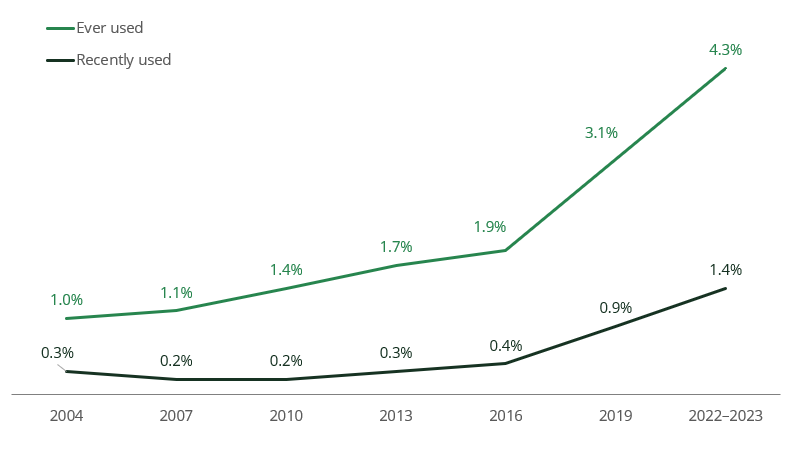
Source: NDSHS 2022–2023, Tables 5.2 and 5.6.
The increase in recent use was largely driven by people in their 30s, from *0.5% in 2019 to 2.5% in 2022–2023. However, it was people in their 20s who were most likely to have used ketamine in the previous 12 months, with 4.2% having done so.
* Estimate has a Relative Standard Error between 25% and 50% and should be interpreted with caution.
Over 1 in 20 (5.8%) gay, lesbian, and bisexual people had used ketamine in the previous 12 months. After adjusting for differences in age, gay, lesbian, and bisexual people were 3.5 times as likely as heterosexual people to have done so.
Use of inhalants stable, but fewer people inhaling petrol
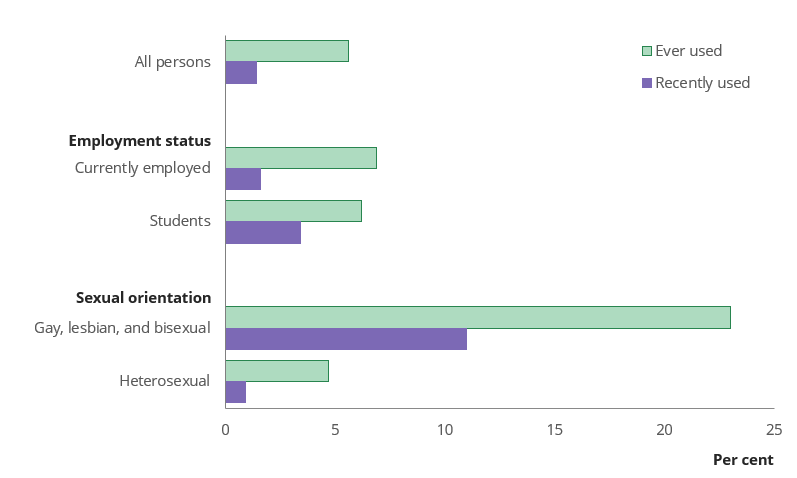
While the proportion of people who had ever used inhalants grew between 2019 (4.8%) and 2022–2023 (5.6%), a similar number of people had used inhalants in the last 12 months (300,000 people in Australia).
Among people who had used inhalants, the two most common forms were amyl nitrate and other nitrates (sometimes called poppers or pearlers, 61%) and nitrous oxide (sometimes called whippits or nangs, 56%). While this pattern was similar to 2019, the proportion of people who had used petrol as an inhalant decreased between 2019 and 2022–2023.
Source: NDSHS 2022–2023, Tables 5.105, 5.106, 10.5 and 10.13.
Use of inhalants was more prevalent in some populations (Figure 2):
- After adjusting for differences in age, gay, lesbian, and bisexual people were 8.6 times as likely to have used inhalants in the previous 12 months as heterosexual people. This is likely due to the use of nitrites during sexual activity by men who have sex with men (Vaccher et al. 2020), although use was high among all gay, lesbian, and bisexual people in the survey.
- Students (3.4%) were more likely to have recently used inhalants than employed people (1.6%), but rates of lifetime use were similar.
Use of heroin and injected drugs remained low at the national level
Recent use of heroin remained low in 2022–2023, with only around *0.1% of the population (30,000 people) having used it in the last 12 months. Around 300,000 people reported having used heroin at least once in their lifetime (1.2% of the population).
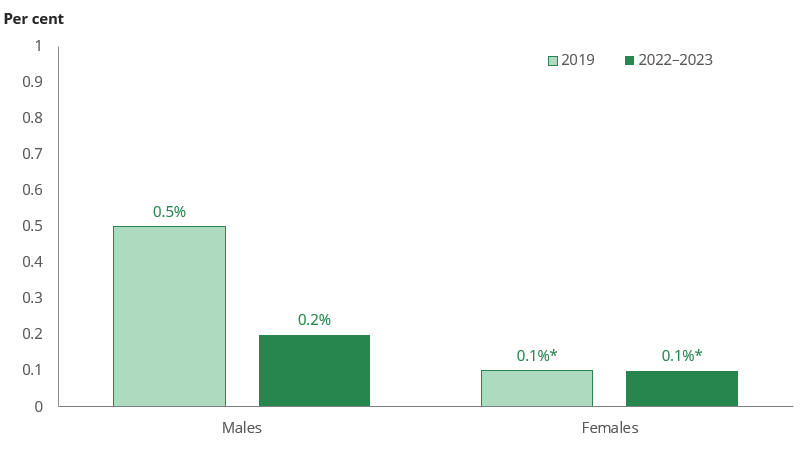
The proportion of people who had injected any illicit drug in the previous 12 months continued a long-term gradual decline, from 0.6% of people in 2001 to 0.2% in 2022–2023 (around 40,000 people).
* Estimate has a Relative Standard Error between 25% and 50% and should be interpreted with caution.
Source: NDSHS 2022–2023, Table 5.105.
While recent use of injecting drugs did not decline among females, there was a decline among males (Figure 3). Only 0.2% of males had injected any illicit drug in the previous 12 months in 2022–2023, less than half the proportion who had done so in 2019 (0.5%).
Needle and syringe programs aim to reduce the harms associated with injecting drug use by providing unused needles and syringes to those who use them (ADF 2019).
Positively, there was an increase in the proportion of people who had accessed a needle and syringe program in the last 12 months, from 42% in 2019 to 67% in 2022–2023.
Synthetic cannabinoids and other synthetic drugs extremely low
Synthetic cannabis/cannabinoids are also known as K2, spice and kronic.
Other synthetic drugs, also called emerging psychoactive substances, are drugs that often mimic the effects of more established illegal drugs. More well-known examples include mephedrone, flakka, 2C-I, NBOMe, carfentanyl and other synthetic forms of fentanyl.
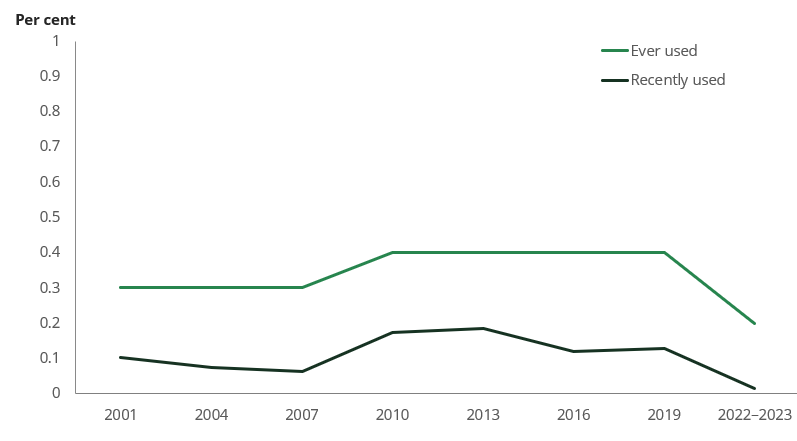
After the NDSHS first began collecting information on synthetic cannabinoids and other synthetic drugs in 2013, the proportion of people who had recently used these drugs has continued to decline (Figure 4). In 2022–2023, only around 20,000 people in Australia had used synthetic cannabinoids in the previous 12 months, and fewer than 10,000 had used other synthetic drugs.
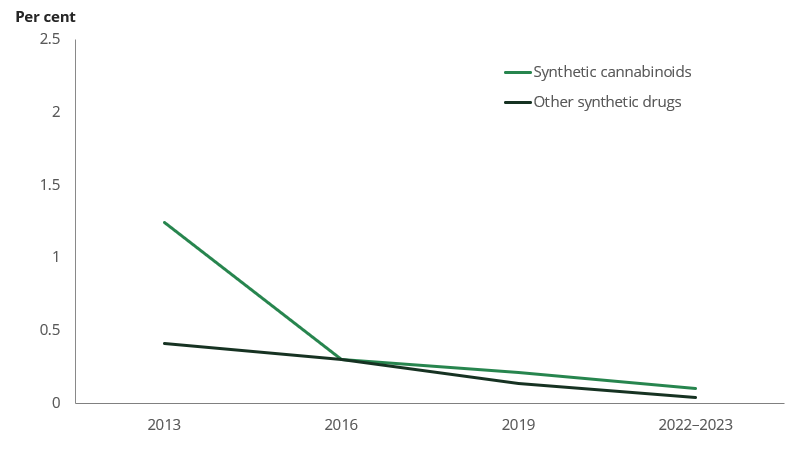
(a) Used in the previous 12 months.
Source: NDSHS 2022–2023, Table 5.6.
These changes were largely driven by reductions in lifetime and recent use of synthetic drugs among people in their 20s. People in their 30s were the most likely to have used synthetic cannabinoids (5.5%) and other synthetic drugs (1.6%) in their lifetime in 2022–2023, but recent use of both drugs was extremely low (both less than 0.2%).
Non‑medical use of methadone and buprenorphine at lowest point seen
Non‑medical use of methadone and buprenorphine
Methadone and buprenorphine are prescribed in Australia for opioid pharmacotherapy treatment. They involve replacing an opioid drug of dependence (for example, heroin or opioid pain-relievers such as oxycodone and fentanyl) with a longer-lasting, medically-prescribed opioid, and are some of the most common treatments used for opioid drug dependence in Australia (AIHW 2023a).
Methadone and buprenorphine are also commonly prescribed pain-relievers (AIHW 2023b).
The NDSHS asks people about their use of methadone and buprenorphine outside of these medical purposes. Non‑medical use includes use for recreational purposes, to induce or enhance a drug experience.
After a sharp increase in non‑medical use of methadone and buprenorphine in 2010, both lifetime use and use in the previous 12 months remained stable until 2019 (Figure 5). However, there was a substantial drop between 2019, when around 30,000 people reported having used methadone or buprenorphine for non‑medical purposes in the previous 12 months, and 2022–2023, when fewer than 10,000 people had done so.
Source: NDSHS 2022–2023, Tables 5.2 and 5.6.


