How do Australia's females access health care?
Page highlights
- Medicare services
Australian females claimed more than 293 million services through Medicare, which equates to an average of 22.7 Medicare services per person, in 2020–21. - Cancer screening
The number of females participating in breast screens was 1.7 million in 2020–21, a 10% drop in numbers since 2018–19, which is likely due to COVID-19 restrictions. - Primary Health Care
- Almost 9 in 10 (88%) Australian females aged 15 and over visited a GP in the previous 12 months.
- Over 2 in 10 (26%) females aged 15 and over who needed to and saw a GP, waited longer than they felt acceptable to get an appointment with a GP, in 2020–21,
- Private health insurance
Three in 5 (60%) Australian females had some form of private health insurance, in 2020–21. - Hospital care
There were 4.5 million emergency department presentations among females, with rates of presentations highest in those aged 85 and over, in 2020–21.
The Australian health system provides a wide range of preventive, treatment and palliative health care services. Monitoring people’s health needs, their help-seeking behaviours, and their patterns of health service use helps government and health service providers to identify inequalities in access and predict future health care needs.
The Medicare Benefits Schedule (MBS) is a listing of the Medicare services subsidised by the Australian Government. Claims data comprise information on services that qualify for a Medicare Benefit, for which a claim has been processed (including bulk billed services). Australian females claimed more than 293 million services through Medicare in 2021–22, an increase from 245 million services in 2019–20. This equates to an average of 22.7 Medicare services per person in that year (SA 2022).
Australian females (of all ages) claimed more than 53 million General Practitioner (GP) services, in 2021–21 (SA 2022). This equates to an average of 4.1 GP services per person in that year.
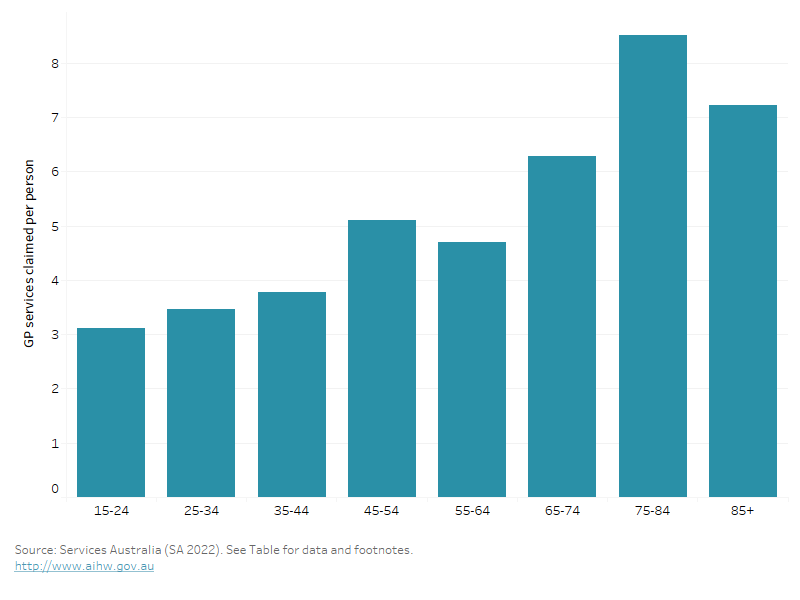
The average number of GP services claimed by females varies by age group. In 2021–22, (Figure 23) (SA 2022):
- females aged under 45 claimed 5.9 services per person
- females aged 75 and over claimed 8.1 services per person.
Figure 23: Average number of GP services per person, claimed through Medicare, by age group, females, 2021–22
This bar chart shows the average number of GP services claimed per person across age groups, with the number of services claimed increasing with age, peaking in those aged 75-84.
Population-based cancer screening involves testing for signs of cancer or conditions that cause cancer before a person has symptoms. Early detection of cancer allows for early intervention, which can improve outcomes.
Breast cancer
BreastScreen Australia aims to reduce illness and death from breast cancer using screening mammography for early detection and early treatment of unsuspected breast cancer. Australian females aged 40 and over are eligible for free mammograms every 2 years, with females aged 50–74 actively targeted to participate in the program.
In 2019–2020 the number of participating females fell slightly to almost 1.8 million and continued to fall in 2020–2021 to about 1.7 million – a 10% drop in numbers since 2018–2019, which is likely due to restrictions associated with the COVID-19 pandemic.
In 2020–21, 48% of females aged 50–74 had a screening mammogram (AIHW 2022m). Females aged 65–69 have the highest participation rate of 52%.
For more information, see Breast cancer screening.
Bowel cancer
For the National Bowel Cancer Screening Program, participation refers to the proportion of people invited who returned a completed a screening test during a specified period and is measured over 2 calendar years to align with the 2-year recommended screening interval.
For bowel cancer screening, the 2020–2021 preliminary data show that females have a higher participation rate than males (43% compared with 39%) across the 50–74 target age group. Participation increases across female age groups from 32% among those aged 50–54 years, to 52% in the 70–74 age group (AIHW 2022o).
For more information, see Bowel cancer screening.
Cervical cancer
From 1 December 2017, the National Cervical Screening Program changed to 5-yearly cervical screening for those aged 25–74. For the period 2018–2022, 4.7 million people (defined as females and people who have a cervix) aged 25–74 had a cervical screening human papillomavirus (HPV) test, an estimated 4-year participation rate of 68% (AIHW 2022n). The National HPV Vaccination Program has been immunising adolescent girls since 2007 and was extended to boys in 2013. Immunisation against the HPV can prevent cervical and other cancers, and other HPV-related diseases. In 2021, the proportion of 15-year-olds who were fully immunised against HPV was (Hull, et al. 2022):
- 80% of girls, and 73% for Indigenous girls
- 77% of boys, and 66% for Indigenous boys.
For more information, see Cervical cancer screening.
In Australia, primary health care is usually a person’s first encounter with the health system when they have a health concern. Primary health care broadly encompasses health care not related to a hospital visit.
Among females aged 15 and over, 88% were estimated to have visited their general practitioner (GP) in the last 12 months in 2021–22. The proportion increases as age increased, with 83% of females aged 15–24 compared to 96% of females aged 65 and over having seen a GP in the last 12 months (ABS 2022q).
Barriers to accessing health services may impede the best possible health outcomes for females. In 2020–21, among females aged 15 and over (ABS 2021f):
- 26% who needed to and saw a GP waited longer than they felt acceptable to get an appointment with a GP
- 4.3% delayed seeing, or did not see, a GP when needed because of cost reasons at least once in the past 12 months
- 6.1% delayed getting, or did not get prescribed medication because of cost.
Among females aged 15 and over:
- 21% needed to and saw a mental health professional, in 2021–22
- 2.8% reported that they saw another mental health professional other than their GP, psychologist or psychiatrist (such as mental health nurse, social worker, counsellor or occupational therapist), in 2021–22 (ABS 2022p)
- 15% of females discussed the issue of reaching a healthy weight with their GP, and this was most discussed in the 55–64 age group (21%) (ABS 2022e)
- 50% of females indicated that they saw dentist or dental professional in the last 12 months, while 23% reported that the last time they had a consultation was more than 2 years ago (ABS 2022e).
For more information see Primary health care.
In Australia, private health insurance is available for those who wish to fully or partly cover the costs of being admitted to hospital as a private patient and/or the costs of other ancillary health services.
Based on the 2020–21 ABS Patient Experience Survey, 3 in 5 Australian females (60%) had some form of private health insurance (ABS 2022d):
- Around half (48%) had both hospital and extras cover.
- 6% had hospital cover only.
- 6% had extras only cover.
Hospital care
Emergency department care
Hospital emergency departments provide care for patients who present for urgent medical attention.
In 2021–22, there were about 4.5 million emergency department presentations among all Australian females, accounting for 51% of all presentations, with rates of presentations highest in those aged 85 and over (AIHW 2021g).
For females aged 15 and over, one of the most common reasons for emergency care is ‘Injury and poisoning’. Other reasons for emergency care varied across age group. For those aged 25–44, ‘pregnancy, childbirth and the puerperium’ was one of the top 3 reasons, while for those aged 45–64 and over 65, ‘Musculoskeletal system diseases’ and ‘Circulatory system diseases’ were among the top reasons, respectively (AIHW 2022b).
For more information see Emergency department care.
Admitted patient care
Admitted patient care refers to care provided by public and private hospitals to admitted patients. A hospitalisation is an episode of hospital care that starts with the formal admission process and ends with the formal separation process.
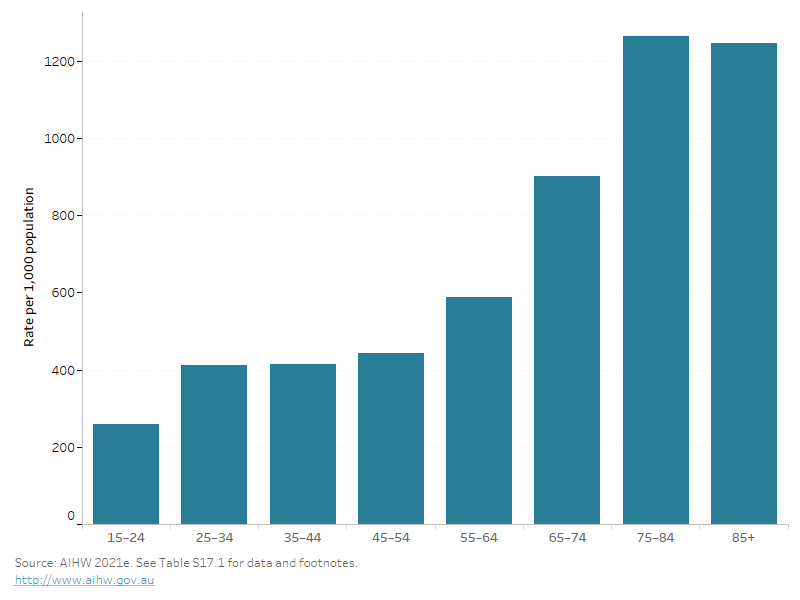
In 2020–21, there were 6.2 million hospitalisations among Australian females, accounting for 52% of all hospitalisations (AIHW 2021f). Hospitalisation rates generally increase with age and are highest among females aged 75 and over (Figure 24) (AIHW 2021e).
The reasons for hospitalisation vary by age and sex as females experience different health issues throughout different times of their lives. For females aged 15–44, the top reason was ‘Pregnancy, childbirth and the puerperium’; For females aged 5–14, the top reasons included ‘Perinatal period conditions’, ‘Respiratory system diseases’ and ‘Injury and poisoning.’ For all other age groups (45–64 and 65 and over), ‘Digestive system diseases’ and ‘Musculoskeletal system diseases’ were among the top reasons for hospitalisation (AIHW 2022b).
Figure 24: Hospitalisations per 1,000 population by age group, females, 2020–21
This bar chart shows the rate of hospital admissions across age groups, with the prevalence increasing with age and highest in those aged 75 and over.
For more information see Admitted patient care.
ABS (2021f) Patient Experiences, [Table 5.3: experience of GP services], abs.gov.au, accessed 17 May 2022.
ABS (2022d) Health Conditions Prevalence 2020-21, [Table 2.3: Long-term health conditions, by age and sex], abs.gov.au, accessed 30 September 2022.
ABS (2022e) Health Conditions Prevalence: Health service usage and type of health professional consulted by age, [Table 15.3: experience of GP services], abs.gov.au, accessed 17 May 2022.
ABS (2022p) Patient Experiences, [Table 27.3 Experience of mental health services], abs.gov.au, accessed 18 May 2022.
ABS (2022q) Patient Experiences, [Table 2.3 Experience of health services in the last 12 months], abs.gov.au, accessed 3 May 2023.
AIHW (2021e) Hospital activity, AIHW website, accessed 27 October 2022.
AIHW (2021f) Hospitals: Admitted patients, AIHW website, accessed 27 October 2022.
AIHW (2021g) Hospitals: Emergency department care 2021–22 [Table 3.1: Emergency department presentations by age and sex], AIHW website, accessed 17 December 2022, AIHW website, accessed 27 October 2022.
AIHW (2022b) Australia's hospitals at a glance, Hospital activity, AIHW website, accessed 8 February 2023.
AIHW (2022m) Cancer screening programs: quarterly data: BreastScreen Australia, AIHW website, accessed 7 October 2022.
AIHW (2022n) Cancer screening programs: quarterly data: Cervical screening participation, AIHW website, accessed 7 October 2022.
AIHW (2022o) Cancer screening programs: quarterly data: National Bowel Cancer Screening Program, AIHW website, accessed 7 October 2022.
Hull B, Hendry A, Dey A, Brotherton J, Macartney K and Beard F (2022) 'Annual Immunisation Coverage Report 2021', National Centre for Immunisation Research and Surveillance Australia.
SA (Services Australia) (2022) Medicare, servicesaustralia.gov.au, accessed 23 November 2022.


