Non-instrumental vaginal birth
Women who have a vaginal birth without intervention tend to have fewer postnatal complications and are more physically able in the short-term to care for their new babies (Rowland and Redshaw 2012). For more information, see Clinical commentary.
This indicator looks at non-instrumental vaginal births for selected women giving birth for the first time.
Key findings
Around 2 in 5 (42%) selected women giving birth for the first time in 2021 had a non‑instrumental vaginal birth.
The proportion of selected women giving birth for the first time having a non-instrumental vaginal birth:
- decreased from 53% in 2004 to 42% in 2021
- was higher in public hospitals than in private hospitals (46% compared with 30% in 2021)
- was higher for women living in areas of most disadvantage (46%) compared with women living in areas of least disadvantage (38%) in 2021
- was lowest for women living in Major cities (41% in 2021) compared with other remoteness areas.
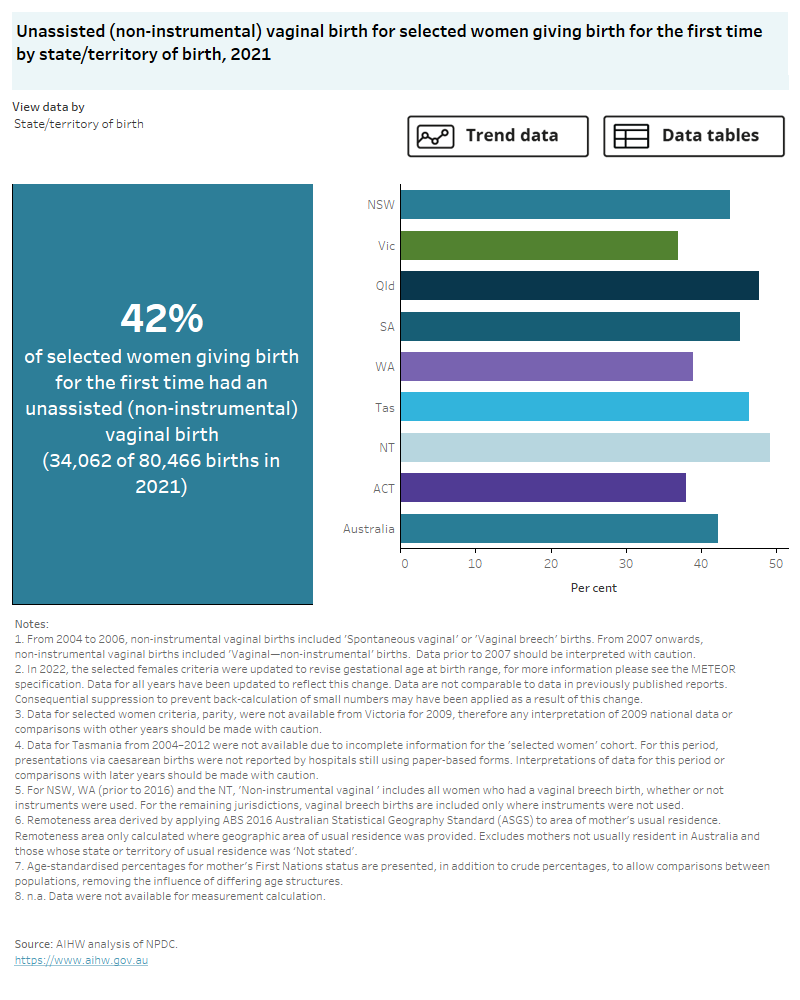
The interactive data visualisation (Figure 8) presents data on unassisted vaginal birth for selected women giving birth for the first time by selected maternal characteristics. Select the trend button to see how data have changed between 2004 and 2021.
Figure 8: Non-instrumental vaginal birth
Non-instrumental vaginal birth for selected women giving birth for the first time, 2004 to 2021.
This chart shows the proportion of women having a non-instrumental vaginal birth for selected women giving birth for the first time, for the current data 2021 and trend data from 2004 to 2021. The proportion for selected women having a non-instrumental vaginal birth for selected women giving birth for the first time decreased from 53% in 2004 to 42% in 2021.
Clinical commentary
A vaginal birth may be the safest option for women with uncomplicated pregnancy or labour. A vaginal birth can result in shorter hospital stays and a faster recovery for birthing mothers (Raising Children Network 2023). Maternal risks associated with vaginal birth may include perineal tears, damage to the pelvic floor, pelvic organ prolapse, and persistent perineal or vulvar pain (Raising Children Network 2023, van Roosmalen and Meguid 2014). Potential neonatal risks related to vaginal births include shoulder dystocia, hypoxia during labour and birth injuries (Raising Children Network 2023, Hannah et al. 2000).
Indicator specifications and data
Excel source data tables are available from Data.
For more information refer to Specifications and notes for analysis in the technical notes.
Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S and Willan AR (2000) ‘Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group’, Lancet 356:1375–1383, doi:10.1016/s0140-6736(00)02840-3.
Raising Children Network (Australia) (2023) Vaginal birth: guide for birthing mothers, Raising Children Network, accessed 20 March 2023.
Rowland I and Redshaw M (2012) ‘Mode of birth and women’s psychological and physical wellbeing in the postnatal period’, BMC Pregnancy and Childbirth, 12:138, doi:10.1186/1471-2393-12-138.
van Roosmalen J and Meguid T (2014) ‘The dilemma of vaginal breech delivery worldwide’, Lancet, 383:1863–1864, doi:10.1016/S0140-6736(14)60618-8.


