Smoking during pregnancy
Smoking during pregnancy is an important preventable risk factor for pregnancy complications and is associated with poorer perinatal outcomes. Supporting women to stop smoking during pregnancy can reduce the risk of adverse outcomes for mothers and their babies. Support to stop smoking is widely available through antenatal clinics. For more information, see Clinical commentary.
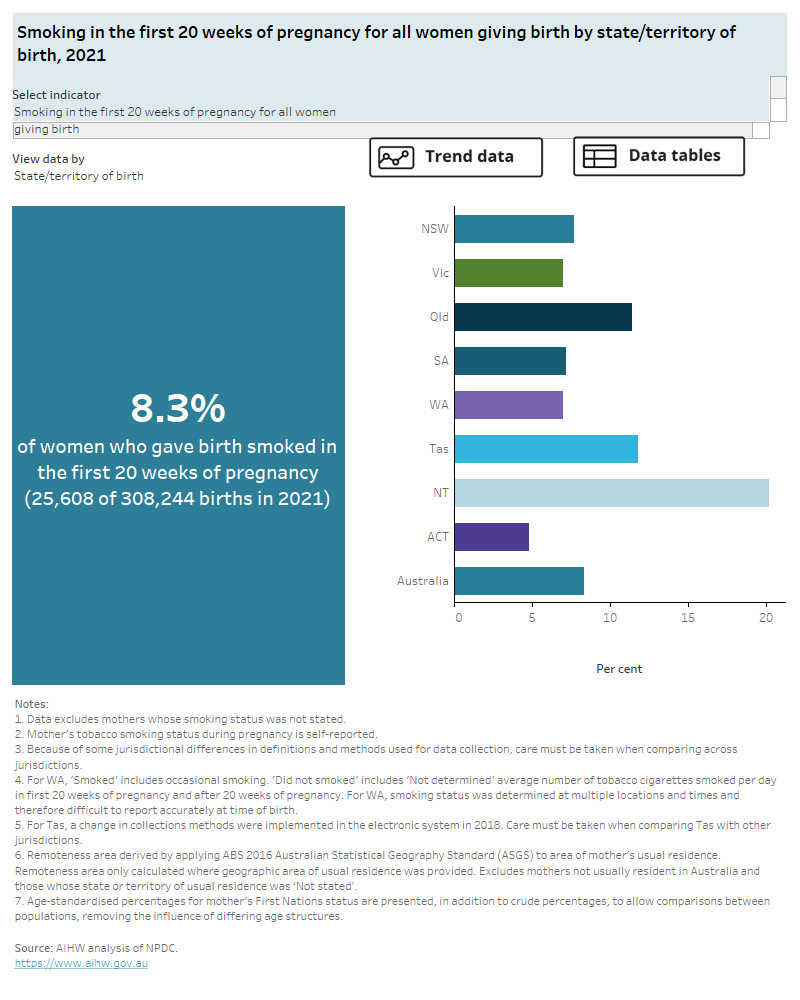
This indicator examines the number of all women who gave birth who reported smoking in the first 20 weeks of pregnancy and those who reported continuing to smoke after the first 20 weeks of pregnancy.
Key findings
- Around 1 in 12 women (8.3%) giving birth in 2021 reported smoking in the first 20 weeks of pregnancy, with almost three quarters of these women (72%) reporting continuing to smoke after the first 20 weeks of pregnancy.
- The proportion of women reporting smoking in the first 20 weeks of pregnancy declined from 13% in 2011 to 8.3% in 2021, while the proportion of women continuing to smoke after the first 20 weeks of pregnancy has slightly increased from 71% in 2011 to 72% in 2021.
The proportion of women reporting smoking in the first 20 weeks of pregnancy:
- generally declined with increasing age, with women younger than 20 having the highest smoking rates (32% in 2021)
- was highest for women living in areas of most disadvantage and lowest for women living in areas of least disadvantage
- was highest for women living in Very remote areas and lowest for women living in Major cities.
The interactive data visualisation (Figure 4) presents data on women who reported smoking in the first 20 weeks of pregnancy and for those who reported continuing smoking after the first 20 weeks, by selected maternal characteristics. Select the trend button to see how data have changed between 2011 and 2021.
Figure 4: Smoking during pregnancy
Smoking in the first 20 weeks of pregnancy for all women giving birth, 2011 to 2021.
The chart displays the percentage of women who smoked during the first 20 weeks of pregnancy for the current data 2021 and trend data from 2011 to 2021. The overall proportion of smoking among Australian mothers decreased from 13% in 2011 to 8.3% in 2021.
The chart also displays the proportion of all women who gave birth and reported smoking during the first 20 weeks of pregnancy and reported smoking during pregnancy after twenty weeks. The percentage of mothers who reported smoking during both periods has increased from 71% in 2011 to 72% in 2021.
Clinical commentary
Women who smoke tobacco during pregnancy are more likely to experience pre-term birth, placental complications and perinatal death of their baby (WHO 2013).
Babies of mothers who smoke during pregnancy are at increased risk of poor growth during pregnancy, particularly during the phase of rapid weight gain from 34 weeks of gestation onwards (Sirvinskiene et al. 2016). Sudden infant death syndrome, childhood diabetes and childhood obesity have been linked with exposure to tobacco during fetal development (Banderali et al. 2015; Flenady et al. 2018). Maternal smoking is associated with low birthweight, which in turn is associated with poor educational outcomes in early childhood, coronary heart disease, type 2 diabetes, and being overweight in adulthood (Guthridge et al. 2015; Lumley et al. 2009).
Smoking cessation during pregnancy is key in reducing the risk of complications during pregnancy and birth as well as reducing adverse health outcomes for the baby. Cessation at later stages of pregnancy will still improve health outcomes for the baby, including improved fetal growth (AIHW 2021; Miyazaki et al. 2015).
There are clear associations between smoking in pregnancy, age of the mother, remoteness of residence and disadvantage quintile evident in the results presented. Varying sociodemographic profiles of women who give birth in public and private hospitals needs to be taken into account when considering the higher rates of smoking in pregnancy for women giving birth in public hospitals.
Indicator specifications and data
Excel source data tables are available from Data.
For more information, refer to Specifications and notes for analysis in the technical notes.
AIHW (Australian Institute of Health and Welfare) (2021) Stillbirths and neonatal deaths in Australia 2017-2018, AIHW, Australian Government, accessed 9 May 2023
Banderali G, Martelli A, Landi M, Moretti F, Betti F, Radaelli G, Lassandro C and Verduci E (2015) ‘Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review’, Journal of Translational Medicine, 13:327, doi:10.1186/s12967-015-0690-y.
Flenady V, Wojiezek AM and Middleton P (2018) ‘Stillbirths: recall to action in high-income countries’, Lancet, 387(10019):691–702, doi:10.1016/S0140-6736(15)01020-X.
Guthridge S, Li L, Silburn S, Li SQ, McKenzie J and Lynch J (2015) ‘Impact of perinatal health and socio-demographic factors on school education outcomes: A population study of Indigenous and non-Indigenous children in the Northern Territory’ Journal of Paediatrics and Child Health, 51(8):778–86, doi:10.1111/jpc.12852.
Lumley J, Chamberlain C, Dowsell T, Oliver S, Oakley L and Watson L (2009) ‘Interventions for promoting smoking cessation during pregnancy’ Cochrane Database of Systematic Reviews, (3):CD001055, doi:10.1002/14651858.CD001055.pub3.
Miyazaki Y, Hayashi K and Imazeki S (2015) ‘Smoking cessation in pregnancy: psychosocial interventions and patient focused perspectives’ International Journal of Women’s Health, 7:415–427, doi:10.2147/IJWH.S54599.
Sirvinskiene G, Zemaitiene N, Jusiene R, Smigelskas K, Veryga A and Markuniene E (2016) ‘Smoking during pregnancy in association with maternal emotional well-being’ Medicina, 52(2):132–138, doi:10.1016/j.medici.2016.02.003.
WHO (World Health Organization) (2013) WHO recommendations for the prevention and management of tobacco use and second-hand smoke exposure in pregnancy, accessed 30 September 2021.


