Coronary heart disease
On this page
Coronary heart disease (CHD) occurs when there is a narrowing or blockage in the blood vessels that supply blood to the heart muscle. There are 2 major clinical forms – heart attack (also known as acute myocardial infarction) and angina (see Glossary).
CHD is largely preventable, as many of its risk factors are modifiable. These include:
- smoking
- biomedical risk factors such as high blood pressure and high blood cholesterol
- physical activity
- diet
- overweight and obesity.
CHD is the leading single cause of disease burden and death in Australia. As a result of the substantial impact of CHD on the Australian population, a National Strategic Action Plan for Heart Disease and Stroke has been developed. The action plan aims to reflect priorities and identify implementable actions to reduce the impact of CHD in the community.
How common is coronary heart disease?
In 2020–21, an estimated 571,000 Australians aged 18 and over (2.9% of the adult population) were living with CHD, based on self-reported data from the Australian Bureau of Statistics 2020–21 National Health Survey (ABS 2022). The prevalence of CHD increases rapidly with age, affecting around 1 in 9 (11%) adults aged 75 and over.
In 2020, an estimated 56,700 people aged 25 and over had an acute coronary event in the form of a heart attack or unstable angina – around 155 events every day. Of these, 6,900 (12%) were fatal.
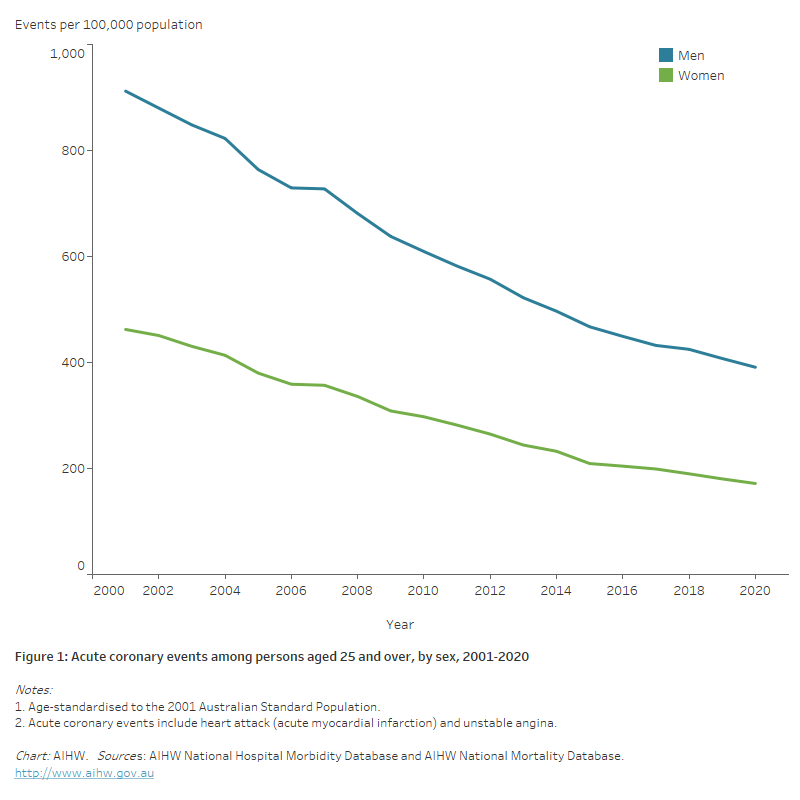
The age-standardised rate of acute coronary events fell by more than half (59%) between 2001 and 2020 (from 675 to 277 per 100,000 population). The decline was slightly higher for women (63%, from 462to 172 per 100,000 population) than men (57%, from 912 to 391 per 100,000 population) (Figure 1).
Figure 1: Acute coronary events among persons aged 25 and over, by sex, 2001–2020
The chart shows declines in the number and age-standardised rates of acute coronary events for persons aged 25 and over between 2001 and 2020. Rates fell from 912 to 391 per 100,000 population for men, and from 462 to 172 for women.
Impact
Deaths
In 2021, CHD was the leading single cause of death in Australia, accounting for 17,300 deaths (AIHW 2023c). This represents 10% of all deaths, and 41% of cardiovascular disease deaths. Thirty-eight per cent (6,500) of CHD deaths resulted from a heart attack.
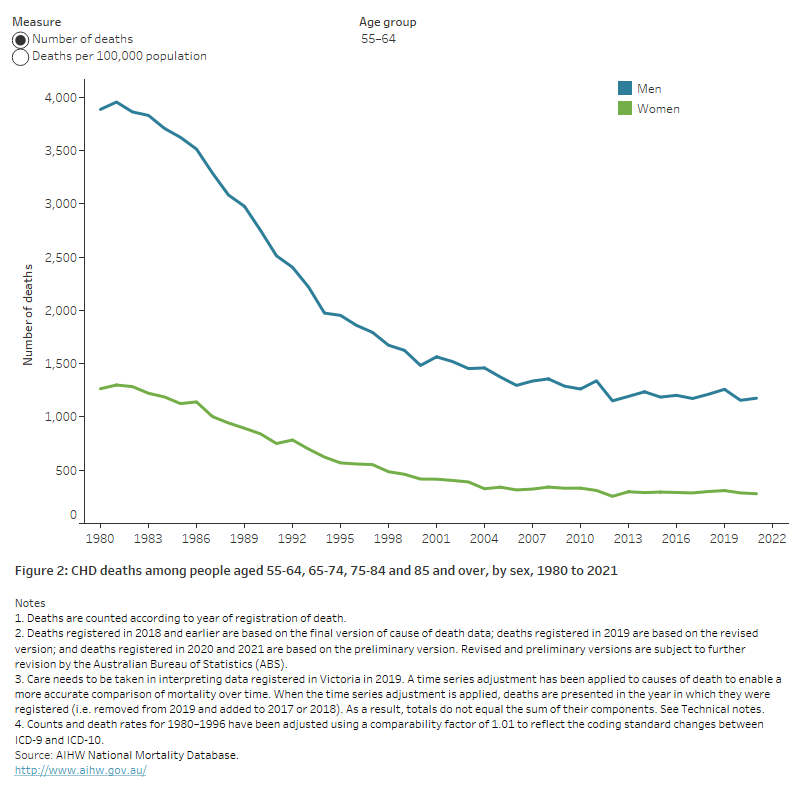
Overall, the CHD death rate has fallen by more than 80% since 1980 – from 414 to 69 deaths per 100,000 population for males, and 209 to 34 per 100,000 population for females. CHD death rates fell substantially in each age group, although the decline has slowed among younger age groups in recent decades (Figure 2).
The decline in CHD death rates has been attributed to a combination of factors, including reductions in some risk factor levels, better treatment and care, and improved secondary prevention (ABS 2018).
See ‘Chapter 4 Changing patterns of mortality in Australia since 1900’ in Australia’s health 2022: data insights.
Figure 2: CHD deaths among people aged 55–64, 65–74, 75–84 and 85 and over, by sex, 1980 to 2021
The chart shows the number and rate of deaths from CHD for males and females aged 55-64, 65-74, 75-84 and 85 and over, from 1980 to 2021. CHD death rates fell substantially in each age group – for example, from 1,500 to 163 deaths per 100,000 population for men aged 65–74, and from 640 to 50 for women aged 65–74.
Burden of disease
In 2023, CHD was the leading specific cause of burden in Australia, with 305,000 years of healthy life lost – equivalent to 11.5 DALY per 1,000 population. The burden was twice as high in males, at 206,000 DALY, as in females (99,000 DALY). It increased rapidly from age 45 onwards – from 6.5 DALY per 1,000 among people aged 45–49, to 190 per 1,000 among people aged 95–99 (AIHW 2023a).
Between 2003 and 2023, there was a 28% fall in CHD burden (from 425,100 DALY to 304,800 DALY), and after adjusting for age, the CHD DALY rate reduced by 58%, from 21 to 8.8 DALY per 1,000 population. The rate of fatal burden of CHD fell by 60%, and the non-fatal burden by 49%. The fall in the number of DALY has been attributed to a number of factors, including population growth, population ageing and a reduction in the amount of disease.
See Burden of cardiovascular disease.
Expenditure
In 2020–21, the estimated expenditure on CHD was $2.5 billion. The greatest cost was due to private hospital services and public hospital admitted patient services ($957.9 million and $915.8 million respectively). The estimated Pharmaceutical Benefits Scheme (PBS) expenditure related to CHD was $156.2 million (AIHW 2023b).
See Health expenditure.
Treatment and management
Primary care
Primary health care professionals, including general practitioners (GPs), practice nurses, nurse practitioners and First Nations health workers, are often the first point-of-care for people who have non-acute cardiovascular disease.
Common actions by primary health care professionals when managing cardiovascular problems include undertaking checks, prescribing medicines, ordering pathology or imaging tests, and referral to specialists.
- In a 2019–20 survey of GP practices, high blood pressure was the single most common chronic condition newly recorded for patients (5.9% of patients) (NPS MedicineWise 2021). Abnormal blood lipids were newly recorded for 3.1% of patients, and cardiovascular disease conditions (including coronary heart disease) for 1.2% of patients.
- In 2021–22, over 112,000 Heart Health Checks (males 55,600, females 57,000) were processed by Medicare. Checks were most commonly conducted among people aged 55–64 (36,600) and 65–74 (33,400) (Services Australia 2022).
See Primary health care.
Medicines
Almost 116 million PBS prescriptions for cardiovascular system medicines were supplied to the Australian community in 2021–22. These comprised more than one-third (37%) of total PBS prescriptions (Department of Health 2022).
More than three-quarters (79%) of the estimated 1.2 million Australian adults aged 18 and over who were living with heart, stroke or vascular disease in 2017–18 used a cardiovascular system medicine in the 2 weeks prior to survey (AIHW analysis of ABS 2019b).
See Medicines for cardiovascular disease.
Emergency Departments
There were 75,900 presentations to Australian public hospital Emergency Departments (EDs) with a principal diagnosis of CHD in 2020–21 – a rate of 295 presentations per 100,000 population (AIHW 2022c).
Of these, 58,200 (77%) were admitted to the hospital to which they presented, 9,600 (13%) departed without being admitted or referred, and 7,300 (10%) were referred to another hospital for admission.
Hospitalisations
In 2020–21, CHD was the principal diagnosis in about 160,000 hospitalisations (1.4% of all hospitalisations, and 27% of all CVD hospitalisations) (AIHW 2022b). Of these, 36% were for heart attack (57,100) and 22% for angina (35,300).
Hospitalisation rates with CHD as the principal diagnosis were 2.5 times as high for males as for females (740 and 293 per 100,000 population) after adjusting for age. Age-specific rates were higher among males across all age groups.
Between 2000–01 and 2020–21, the age-standardised rate of hospitalisations where CHD was the principal diagnosis declined by 39%, from 833 to 508 hospitalisations per 100,000 population. The decline in hospitalisations over this period was greater among females than among males (45% and 36% respectively).
See Hospital care and procedures.
Variation between population groups
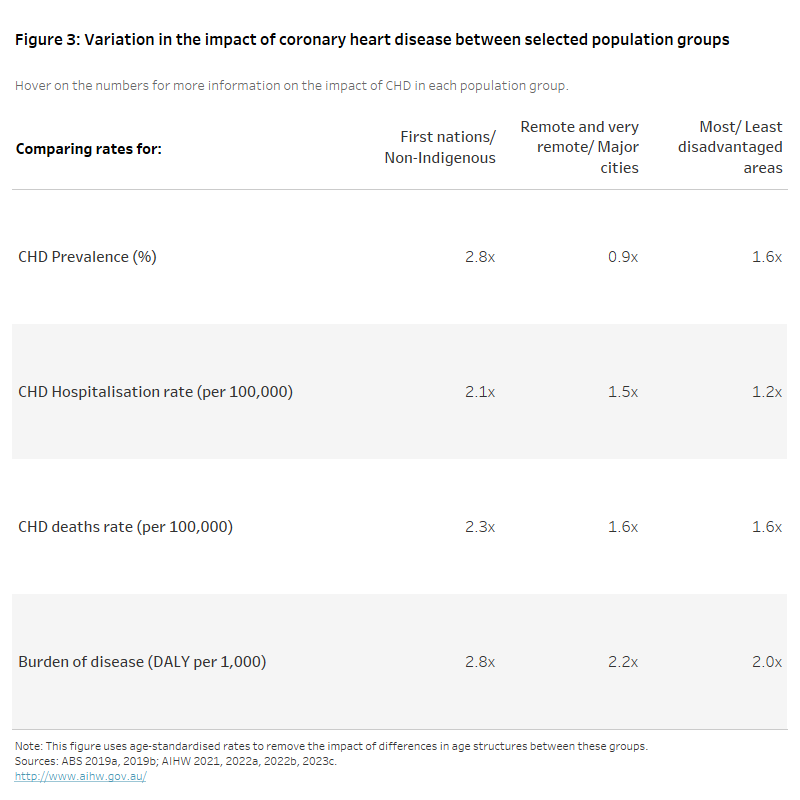
The impact of CHD varies between population groups. To account for differences in the age structures of these groups, the data presented below is based on age-standardised rates.
Age-standardised rates of CHD hospitalisation in 2020–21 were 1.5 times as high in Remote and very remote areas as in Major cities, and 1.2 times as high in the lowest socioeconomic areas as in the highest (Figure 3).
The age-standardised rate of hospitalisations, deaths and total burden due to CHD were more than twice as high among First Nations people as among non-Indigenous Australians.
The figure shows the rate ratio of CHD prevalence (2017–18), hospitalisation (2020–21), death (2021) and burden of disease (2018) among selected population groups.
Rates of CHD prevalence, hospitalisations, deaths and burden of disease were more than twice as high among First Nations persons when compared with non-Indigenous Australians.
Rates of hospitalisations and deaths due to CHD were 1.5 and 1.6 times as high among those living in Remote and very remote areas compared to those living in Major cities and were 1.2 and 1.7 times as high among those living in the most disadvantaged areas when compared to those living in the least disadvantaged areas.
COVID-19 and coronary heart disease
People with pre-existing chronic conditions such as CHD are at higher risk of contracting COVID-19 and experiencing complications or more severe illnesses as a result.
In 2020–21, there were over 4,700 hospitalisations in Australia that involved a COVID-19 diagnosis. The most common comorbid conditions associated with COVID-19 hospitalisations over this period were cardiovascular disease (which includes coronary heart disease and a range of other heart, stroke and vascular diseases) (20%) and Type 2 diabetes (20%) (AIHW 2022d).
The first wave of the pandemic affected hospital procedures for CHD. Coronary angiographies fell by 27% from 11,600 in March 2020 to 8,400 in April 2020. Percutaneous coronary interventions fell by 19% from 3,850 in March 2020 to 3,120 in April 2020.
Among COVID-19 deaths that occurred by 28 February 2023, chronic cardiac conditions including coronary atherosclerosis, cardiomyopathies and atrial fibrillation were the most certified comorbidities, present in 40% of deaths (ABS 2023a).
Australian Bureau of Statistics (ABS) provisional mortality statistics indicate that there were 13,700 doctor-certified deaths due to CHD during 2020, rising to 14,100 in 2021 and 14,900 in 2022 (ABS 2023b). CHD mortality continued its historical decline in 2020, the first year of the pandemic, but has since increased – the number of deaths in 2022 being 9.1% higher than the number in 2020.
Where do I go for more information?
For more information on coronary heart disease, see: Coronary heart disease.
ABS (Australian Bureau of Statistics) (2018) Changing patterns of mortality in Australia, ABS, Australian Government, accessed 15 February 2022.
ABS (2019a) Microdata: National Aboriginal and Torres Strait Islander Health Survey, 2018-19, AIHW analysis of detailed microdata, accessed 4 March 2021.
ABS (2019b) Microdata and TableBuilder: National Health Survey, AIHW analysis of detailed microdata, accessed 4 March 2021.
ABS (2022) Health conditions prevalence, ABS, Australian Government, accessed 21 March 2022.
ABS (2023a) COVID-19 mortality in Australia, ABS, Australian Government, accessed 31 March 2023.
ABS (2023b) Provisional mortality statistics, ABS, Australian Government, accessed 31 March 2023.
Australian Institute of Health and Welfare (2021) Australian Burden of Disease Study 2018: Interactive data on disease burden, AIHW, Australian Government, accessed 11 March 2022.
AIHW (2022a) Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018, AIHW, Australian Government, accessed 11 March 2022.
AIHW (2022b) National Hospital Morbidity Database, Findings based on unit record analysis, AIHW, Australian Government, accessed 1 September 2022.
AIHW (2022c) National Non-admitted Patient Emergency Department Care Database, Findings based on unit record analysis, AIHW, Australian Government, accessed 1 September 2022.
AIHW (2022d) MyHospitals. Admitted patient activity, AIHW, Australian Government, accessed 2 June 2022.
AIHW (2023a) Australian Burden of Disease Study 2023, AIHW, Australian Government, accessed 14 December 2023.
AIHW (2023b) Health system spending on disease and injury in Australia 2020-21, AIHW, Australian Government, accessed 29 November 2023.
AIHW (2023c) National Mortality Database, Findings based on unit record analysis, AIHW, Australian Government, accessed 23 March 2023.
Department of Health and Aged Care (2022) PBS expenditure and prescriptions report 1 July 2021 to 30 June 2022, Department of Health and Aged Care, Australian Government, accessed 1 March 2023.
NPS MedicineWise (2021) General Practice Insights Report July 2019–June 2020 including analyses related to the impact of COVID-19, NPS MedicineWise, Sydney, accessed 24 March 2022.
Services Australia (2022) Medicare item reports, Services Australia, Australian Government, accessed 23 November 2022.


