< Explore study cohort articles
Study cohort – Specialist homelessness services: Clients supported in 2015–16
Introduction
Specialist homelessness agencies provide services aimed at prevention and early intervention as well as crisis assistance to support people experiencing or at risk of homelessness. A general cohort was created to examine the characteristics and service use patterns of SHS clients over time.
See Introduction to the SHS longitudinal data for details on the longitudinal analyses undertaken.
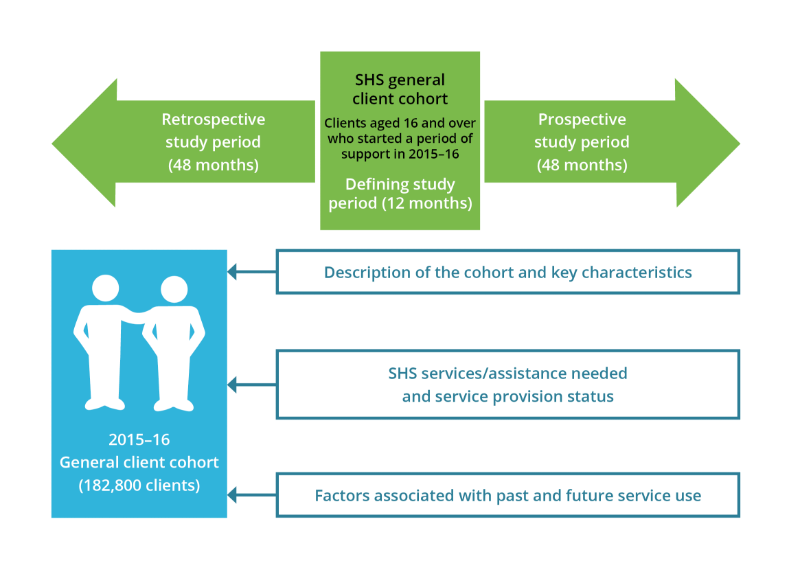
The 2015–16 general cohort was defined as clients aged 16 and over that commenced a period of support from a specialist homelessness service (SHS) at any time during 2015–16.
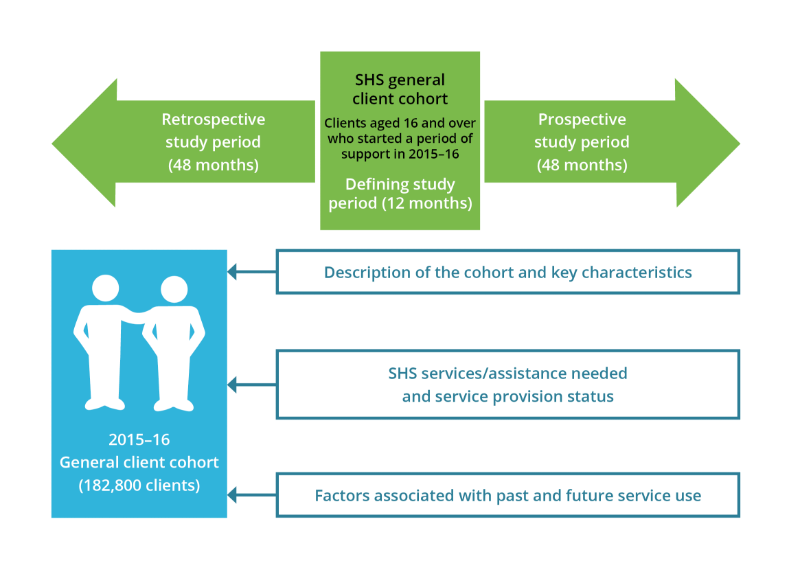
Characteristics and outcomes for the general cohort were examined using aggregated support period data for discrete study periods (Figure GENERAL.1). The defining study period covered 12 months from the first day of their first support period during 2015–16. The retrospective period for this cohort was 48 months (that is, the 48 months before the first day of the client’s first support period in 2015–16). The prospective study period for each client ranged for the 48 months after the defining period ended.
Note, support periods fall into study periods solely based on the day on which they commenced; a support period that commenced in the defining period but continued into the prospective period, for example, will be aggregated into the defining study period data only.
A general cohort was created to examine patterns of service usage for all clients.
Source: AIHW analysis of SHS longitudinal data 2011–21, Table GEN1516.1.
Key characteristics of the general cohort
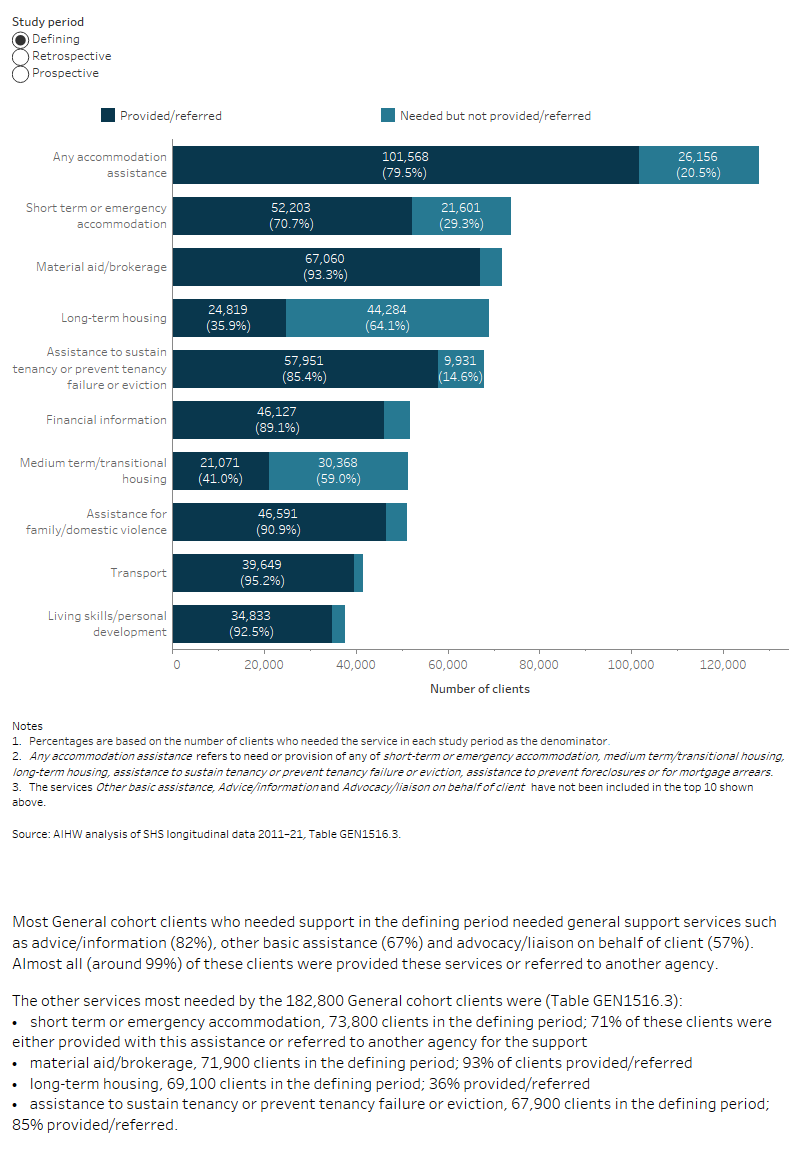
There were nearly 182,800 clients in the 2015–16 General Cohort with the following key characteristics during the 12-month defining study period (which started in 2015–16) (Table GEN1516.1):
- Most clients (69% or 126,400 clients) were aged 18 to 44 years at the time of their first support period in 2015–16.
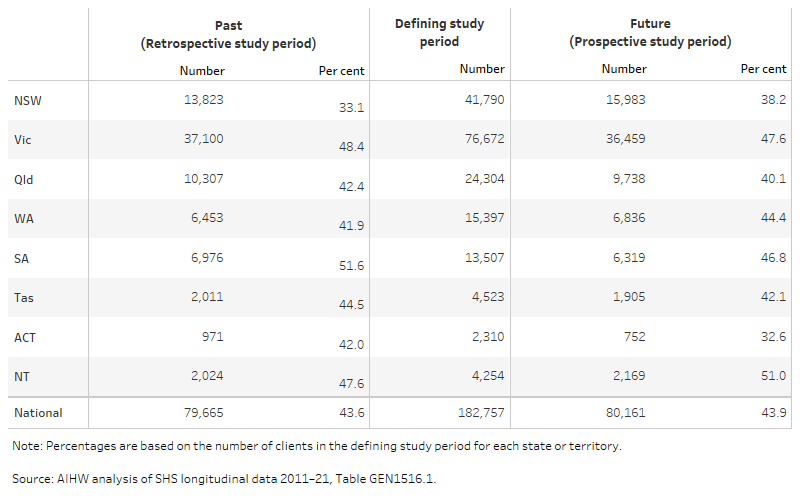
- Around 76,700 clients (42%) received their first service of 2015–16 in Victoria, nearly 41,800 (23%) in New South Wales and 13% (24,300 clients) in Queensland.
- Around 114,900 clients (63%) were female.
- Around 41,400 clients (23%) were Indigenous and about 30,800 (17%) clients were born overseas.
- Over half (55%, or almost 100,400 clients) had only one support period during the 12-month defining study period.
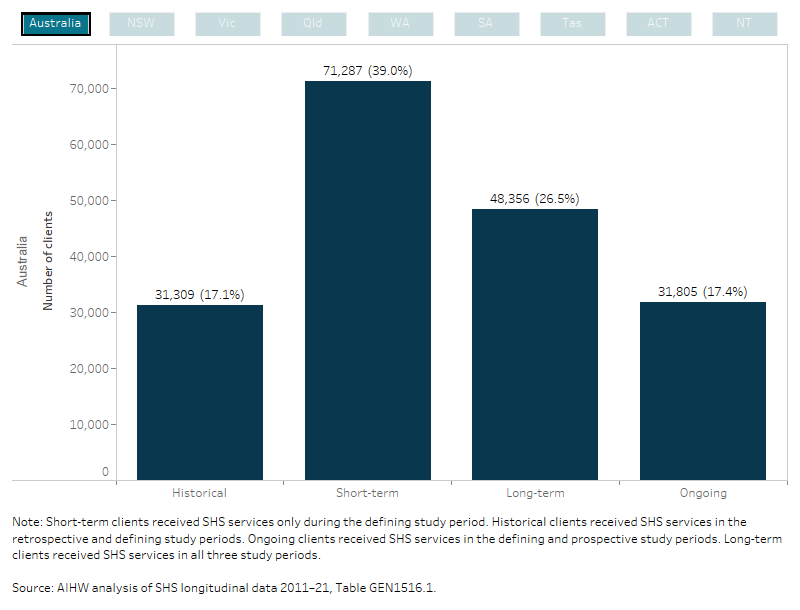
Less than half (44%) had used SHS services previously (Table GEN1516.1); that is, nearly 79,700 clients had used SHS services in the 48-month retrospective study period that preceded the first support period in the defining study period for each client. Of these:
Around 44% of clients (80,200 clients) were ongoing SHS service users, meaning they received SHS support in the 48-month prospective study period (Table GEN1516.1). Of these:
- Over 40,800 clients (22%) had a mental health issue.
- Around 10% (19,100 clients) had a drug or alcohol problem.
Vulnerability pathways
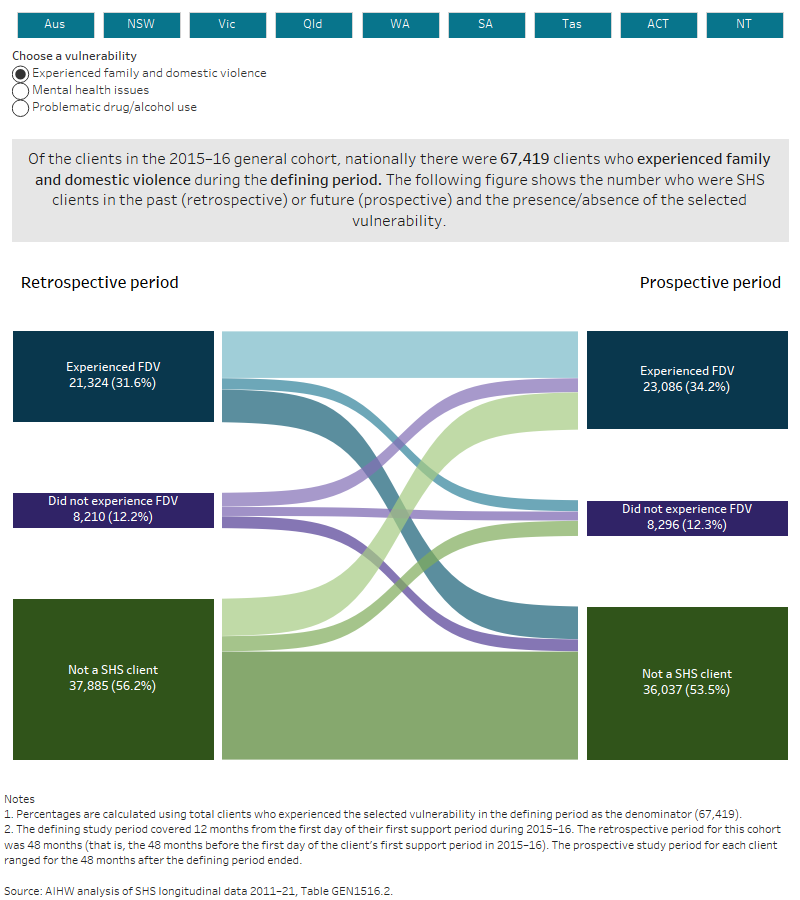
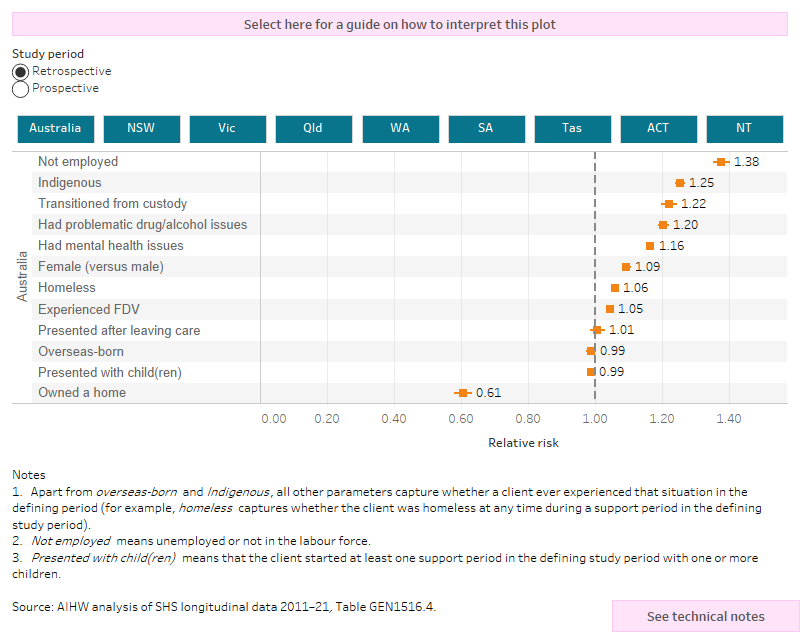
Using data for the entire longitudinal period, SHS clients were assessed for the presence of vulnerabilities including mental health issues, drug and/or alcohol problems, and experience of family and domestic violence (FDV) issues within each of the 3 study periods – the retrospective, defining and prospective periods (Figure GENERAL.2, Table GEN1516.1, Table GEN1516.2). For more information on the derivation of these vulnerabilities, see Methodology.
Around one-third of clients (63,000) had mental health issues in the defining period. Of these, nearly 11,000 (17% of clients with mental health issues in the defining period) had mental health issues in both the retrospective and prospective periods, whereas 15% (9,100 clients) only had mental health issues in the past (retrospective period) in addition to the defining study period. Nearly 20% (12,400 clients) had ongoing mental health issues only (in both the defining and prospective periods).
Figure GENERAL.2 and Table GEN1516.2 show vulnerability pathways for clients experiencing FDV, clients with a mental health issue and those with problems with drugs or alcohol.