Specialist homelessness services client pathways: Clients with mental health issues in 2015–16
Citation
AIHW
Australian Institute of Health and Welfare (2022) Specialist homelessness services client pathways: Clients with mental health issues in 2015–16, AIHW, Australian Government, accessed 22 October 2024.
APA
Australian Institute of Health and Welfare. (2022). Specialist homelessness services client pathways: Clients with mental health issues in 2015–16. Retrieved from https://www.aihw.gov.au/reports/homelessness-services/shs-mental-health-2015-16
MLA
Specialist homelessness services client pathways: Clients with mental health issues in 2015–16. Australian Institute of Health and Welfare, 07 June 2022, https://www.aihw.gov.au/reports/homelessness-services/shs-mental-health-2015-16
Vancouver
Australian Institute of Health and Welfare. Specialist homelessness services client pathways: Clients with mental health issues in 2015–16 [Internet]. Canberra: Australian Institute of Health and Welfare, 2022 [cited 2024 Oct. 22]. Available from: https://www.aihw.gov.au/reports/homelessness-services/shs-mental-health-2015-16
Harvard
Australian Institute of Health and Welfare (AIHW) 2022, Specialist homelessness services client pathways: Clients with mental health issues in 2015–16, viewed 22 October 2024, https://www.aihw.gov.au/reports/homelessness-services/shs-mental-health-2015-16
Get citations as an Endnote file: Endnote
PDF | 1017Kb
On this page:
Study cohort – Specialist homelessness services: Clients with mental health issues in 2015–16
Introduction
People experiencing both homelessness and mental health issues are a vulnerable sub-group of SHS clients (see Clients with a mental health issue).
Longitudinal analyses have been undertaken for a cohort of MH clients in 2015–16. These analyses are designed to examine SHS service usage patterns for a cohort of service users that can be tracked for a relatively similar period in the past and into the future.
See Introduction to the SHS longitudinal data for details on the longitudinal analysis undertaken.
The Mental Health (MH) 2015–16 SHS client cohort was defined as SHS clients that met any of the following conditions in any of the support periods in 2015–16 (termed MH cohort throughout this article):
- they indicated that at the beginning of a support period they were receiving services or assistance for their mental health issues or had in the previous 12 months
- their formal referral source to the specialist homelessness agency was a mental health service
- they reported ‘mental health issues’ as a reason for seeking assistance
- their dwelling type was as a psychiatric hospital or unit either a week before presenting to an agency, or when presenting to an agency
- they had been in a psychiatric hospital or unit in the previous 12 months
- at some stage during their support period, a need was identified for psychological services, psychiatric services or mental health services.
The above is consistent with the approach used in other AIHW SHS publications such as the 2020–21 SHS annual report (AIHW 2021). The above criteria include whether the client received support for mental health issues in the previous 12 months or whether the client was in a psychiatric hospital or unit in the previous 12 months. Therefore, it is possible that some clients in the mental health cohort did not have a mental health issue in the defining study period (and did not require services for mental health issues) but they had these issues only in the past.
The longitudinal analyses are limited to adult clients (aged 18 and over). This is because the longitudinal analyses focus on pathways for individual clients, whereas children accessing services may need support because of issues that are unrelated to them directly.
A comparison cohort (non-MH cohort) was also created, comprising clients aged 18 and over who did not meet the criteria for inclusion in the MH cohort. These clients did not meet any of the above conditions in any of the support periods during their defining study period (12 months from the start of their first support period in 2015–16) and were therefore considered to have not had mental health issues in the defining study period. More information on the how comparison cohorts were derived can be found in the Methodology section.
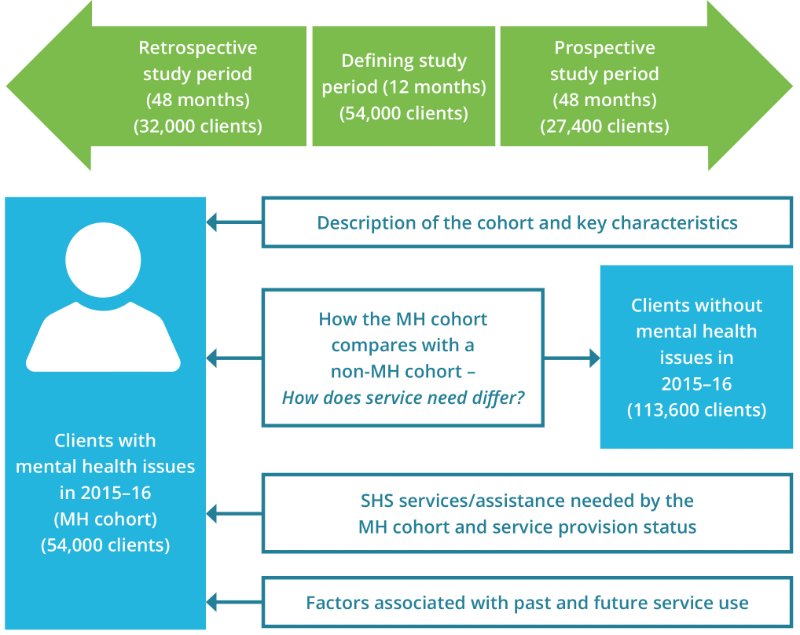
The longitudinal SHSC data for the period 2011–21 were used to (Figure MH.1):
- examine characteristics of SHS clients with a mental health issue (the MH cohort) compared with the comparison cohort (the non-MH cohort)
- examine outcomes for the MH cohort in terms of historical and future service use.
The retrospective study period for this cohort is the 48 months before the start of the defining study period (that is, the 12 months from the start of their first mental-health related support period in 2015–16). The prospective study period is the 48 months after the end of each client’s 12-month defining study period.
Figure MH.1: Clients with mental health issues cohort, longitudinal analysis overview
Key characteristics of the MH 2015–16 cohort
There were over 54,000 clients who received support from SHS agencies in the MH 2015–16 cohort with the following key characteristics (Table MH1516.1):
- The mean age of clients was 36 years with 26% (nearly 14,000 clients) aged 25–34 years and 27% (nearly 14,500 clients) aged 35 to 44 years at the time of their first MH-related support period in 2015–16.
- Around 10,800 clients (20%) were Indigenous.
- Nearly 8,600 clients (16%) were born overseas.
- Nearly half (46%, 25,000 clients) had only one support period during the defining study period and 31% (nearly 17,000) had 3 or more support periods.
- Over 59% had used services previously; that is, 32,000 clients had used services in the 48-month retrospective period that preceded the defining study period. Of these clients, 17,900 (33% of the defining cohort and 56% of clients that used services in the past) had mental health issues during a historical period of support.
- Over half (51%) of clients (27,400) continued to use services into the future; that is, they received support in the 48 months after the 12-month defining study period. Of these clients, nearly 19,500 (22% of the defining cohort, 71% of clients that continued to use services) had mental health issues during a future period of support.
Service engagement profiles
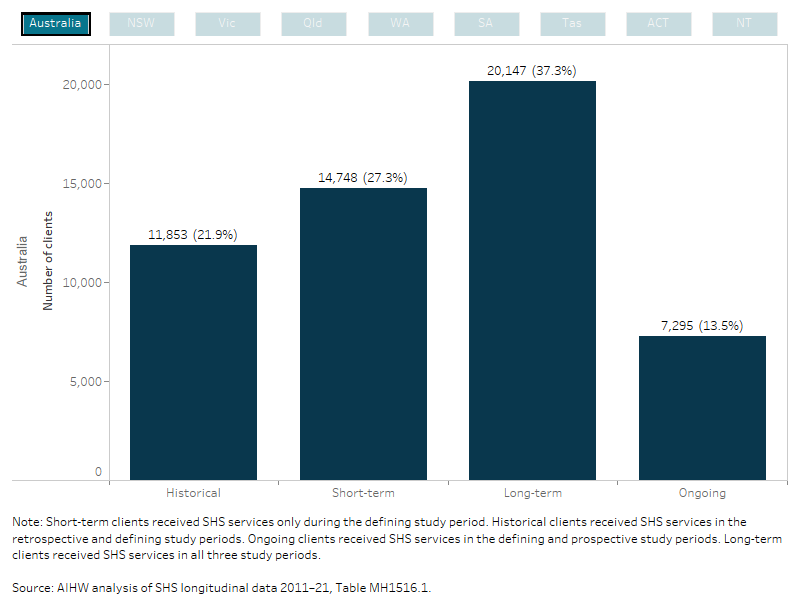
Service use patterns of the MH cohort over the entire longitudinal period (2011–21) were examined. Over a third (20,100 or 37%) of the MH cohort were long-term clients (they used services in the retrospective and prospective periods as well as the defining period) (Figure MH.2, Table MH1516.1).
Figure MH.2: MH client cohort 2015–16, service engagement profiles
This interactive bar chart shows service use patterns of the MH cohort over the entire longitudinal period (2011–21). Support information was combined from the discrete study periods into four service engagement profile groups (historical, short-term, long-term and ongoing). Engagement profiles for all states and territories and Australia can be selected and displayed. Nationally, of the 54,000 clients that made up the study period cohort, over a third (20,100 or 37%) of the MH cohort were long-term clients (they used services in the retrospective and prospective periods as well as the defining period). For NSW clients, 36% were short-term clients and had used SHS support during the defining period only.
How the MH cohort compares with a non-MH cohort
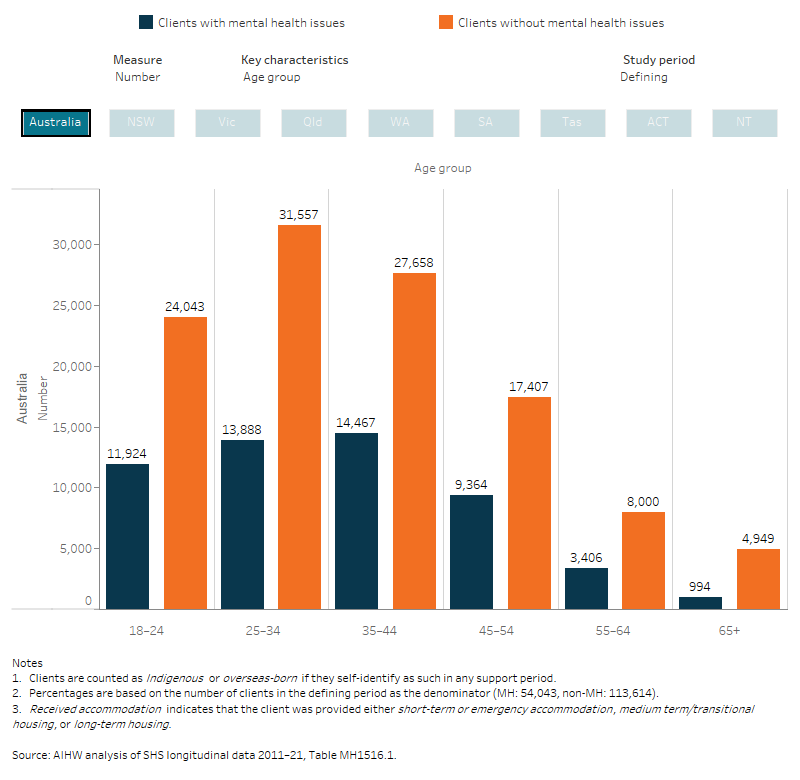
Key comparisons between the MH and non-MH clients receiving SHS support in 2015–16 include (Figure MH.3, Table MH1516.1):
- The MH cohort had a similar age profile to the non-MH cohort.
- Clients in the MH cohort were more likely to be male; 42% compared with 35% for the non-MH cohort.
- During the defining study period the MH cohort were more likely to have experienced homelessness (65% compared with 42% for the non-MH cohort) and much more likely to have had problematic drug or alcohol issues (27% compared with 6%).
- Nearly all clients in the MH cohort (93%) were not employed (that is, unemployed or not in the labour force) at some time during the defining study period compared with 73% of clients in the non-MH cohort. Also, 72% of mental health clients were never known to be employed in the defining period, compared with 60% of non-MH clients.
- The MH cohort were more likely (6.5% compared with 3.4%) to be transitioning from custody.
- MH clients were twice as likely to have had 3 or more support periods in the defining study period than the non-MH cohort (31% compared with 16%) and less likely to have had only one support period than non-MH clients (46% compared with 64%). This may be related to their overall need for support relative to non-MH clients or may be a function of the type of support these clients need (see [section of relative risk for services needed – for example, services provided to MH clients, such as counselling, may be more recurrent than other services).
- MH clients were more likely to have received accommodation (38% compared with 22%). They also received many more nights of accommodation than non-MH clients; during the defining study period MH clients received an average of 44 nights of accommodation compared with14 nights for non-MH clients.
- MH cohort clients were much less likely to be short-term clients (27% compared with 43% of the non-MH cohort), meaning that they were less likely to have only used services in the defining study period.
- Clients in the MH cohort were more likely than the non-MH cohort (37% compared with 23%) to be long-term clients, that is, they were more likely to receive SHS support in the past and in the future.
Figure MH.3: MH and non-MH cohort, client key characteristics, by study period, 2015–16
This interactive bar chart shows a comparison between the MH and non- MH cohorts, in terms of key characteristics and across all study periods (defining, retrospective and prospective). A radio button allows selection for the individual state/territory and Australia. For Australia, the MH cohort had a similar age profile to the non-MH cohort, however clients in the MH cohort were more likely to be male; 42% compared with 35% for the non-MH cohort. Clients in the MH cohort were more likely than the non-MH cohort (37% compared with 23%) to be long-term clients, that is, they were more likely to receive SHS support in the past and in the future.
How did service needs differ?
The types of services needed by MH and non-MH cohort clients receiving SHS support were compared using relative risk, which was calculated by dividing the risk of an event occurring for one group (specifically, service need for each service type separately for MH clients) by the risk of an event occurring for another group (service need for non-MH clients).
MH clients were nearly 10 times more likely to need intellectual disability services (relative risk (RR) 9.78) during the 2015–16 defining study period than clients in the non-MH cohort (Figure MH.4; Table MH1516.2).
The diversity in the services needed demonstrates that MH clients had very broad needs that extend beyond mental health issues.
Figure MH.4: Relative risk of needing a SHS service type, MH and non-MH clients, by study period, 2015–16
The interactive risk ratio plot shows the differences in service need between MH and non- MH clients receiving SHS support in each study period, these associations are presented as relative risks. The top 6 services more likely to be needed by MH cohort clients compared with non-MH clients (that is, those with the largest relative risk) have been shown in the figure. A radio button allows selection of the services and relative risks for each of the study periods (defining, retrospective and prospective). MH clients were nearly 10 times more likely to need intellectual disability services (relative risk (RR) 9.78) during the 2015–16 defining study period than clients in the non-MH cohort.

SHS clients – MH cohort past and future service use
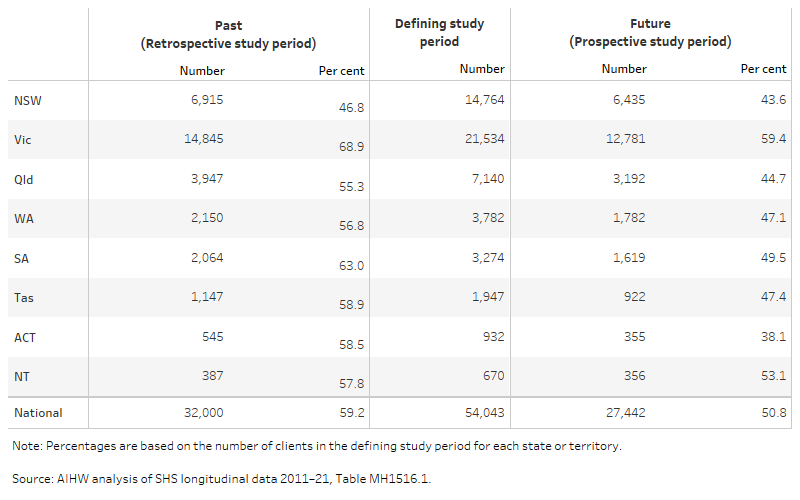
Services provided by SHS agencies was examined for the 2015–16 MH cohort in each study period (Table MH.1). Nearly 40% (over 21,500 clients) of the clients received their first mental-health related support from agencies in Victoria in the defining period, followed by 27% in New South Wales and 13% in Queensland.
Clients in Victoria were most likely to have received support in the past (69% of the cohort, nearly 14,900 clients) followed by SA (63% of the cohort, over 2,000 clients). Similarly, clients who received support in Victoria during the 2015–16 study period were most likely to continue to receive support into the prospective period (59% of clients), compared with clients from the ACT who were least likely (38%).
Table MH.1: MH clients 2015–16, by past (retrospective) and future (prospective) service use and state/territory
The table shows the number and per cent of MH cohort clients within each study period for each state and territory and Australia. Nearly 40% (over 21,500 clients) of the clients received their first mental-health related support from agencies in Victoria in the defining period, followed by 27% in New South Wales and 13% in Queensland. Clients in Victoria were most likely to have received support in the past (69% of the cohort, nearly 14,900 clients) and future periods (59% of clients).
SHS services needed by MH cohort clients
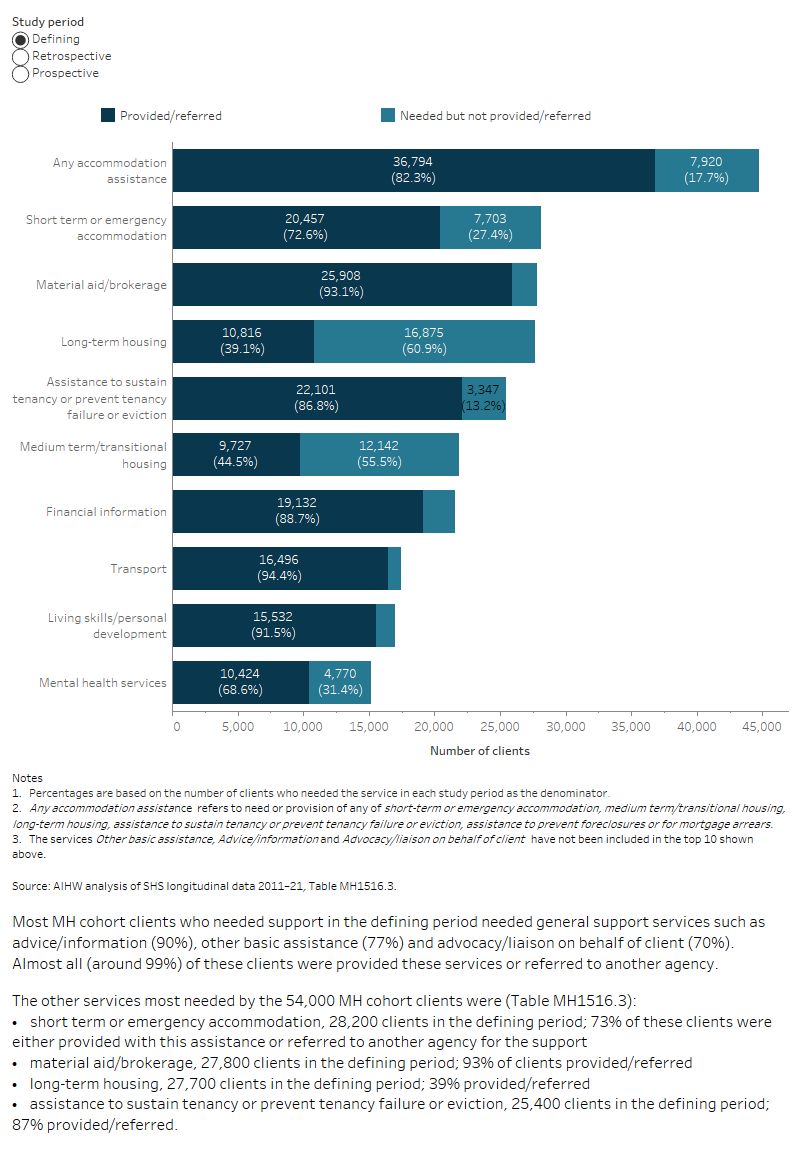
The need for, and provision/referral of, SHS services was examined for the MH cohort clients in the retrospective, defining and prospective study periods; aggregation is based on services needed or provided/referred in support periods that commenced within each study period only.
Patterns of service need were generally similar for the MH cohort clients across the 3 study periods (Figure MH.5, Table MH1516.1, Table MH1516.3). Some specific types of accommodation assistance were more prominent in the prospective period, such as a need for long-term housing (increasing from 55% of clients in the retrospective period and 51% in the defining period to 60% in the prospective period) and assistance to sustain tenancy or prevent eviction (53%, 47%, 58% respectively).
Intellectual disability services, which were 10 times more prominent among the services needed by MH clients relative to non-MH clients (Table MH1516.3), were needed by relatively few MH cohort clients (1.9% in the retrospective and defining periods) but proportionally more so among ongoing clients (2.5%).
Although a need for psychological services, psychiatric services or mental health services is one of the possible criteria for clients being included in the mental health cohort, only a small proportion of the MH cohort needed these services from SHS agencies; either self-requested or as determined by the agency worker. Around 10% of the MH cohort in each study period required psychological services, with most (57% to 70%, depending on the study period) receiving them. Around 8% of clients required psychiatric services (in any of the study periods); 74% of the clients in the retrospective study period that required these services received them, compared with 60% of clients in the prospective period and 61% in the defining study period. Mental health services were required by 28% of clients in the defining period (25% in the prospective period, 23% in the retrospective period) and most clients received these services (69% in the defining period, 80% in the retrospective period, 71% in the prospective period).
Figure MH.5: MH clients 2015–16, select top 10 services and assistance needed and service provision status by study period
The interactive stacked horizontal bar graph shows the select top 10 services needed and the provision/referral status for the MH cohort clients (54,000 clients) that used services in the retrospective, defining and prospective study periods. Patterns of service need were generally similar for the MH cohort clients across the three study periods. Some specific types of accommodation assistance were more prominent in the prospective period, such as a need for long-term housing (increasing from 55% of clients in the retrospective period and 51% in the defining period to 60% in the prospective period) and assistance to sustain tenancy or prevent eviction (53%, 47%, 58% respectively). Intellectual disability services, which were 10 times more prominent among the services needed by MH clients relative to non-MH clients, were needed by relatively few MH cohort clients (1.9% in the retrospective and defining periods) but proportionally more so among ongoing clients (2.5%).
Factors associated with past and future SHS service use
Descriptive regression models were used to examine whether client characteristics or support experiences in the defining period were associated with receipt of SHS support in the prospective study period (ongoing service use) or, separately, in the retrospective period (historical service use). Information on interpreting regression models can be found in the section Understanding factors associated with past and future support.
Some bias is present in this outcome measure because some clients who required services in the future may not have been able to receive them (see the section on Bias within the SHSC longitudinal data).
What client characteristics are associated with using SHS services in the retrospective study period?
Some client characteristics or circumstances are associated with SHS support in the past (relative to the defining study period). However, variations in state-territory specific policy and service deliver models mean that the likelihood of a client using services in the future varies among states or territories. Therefore, in addition to a national model, separate regression models were created for each state or territory where there was sufficient sample size. The models are descriptive, that is, they are intended to describe the client variables that are associated with past or future service use without proposing or testing specific causal pathways.
The outcome variable (receipt of SHS support) was a binary measure (yes or no) and did not distinguish between clients that needed SHS services only once in the retrospective study period and clients that required frequent support.
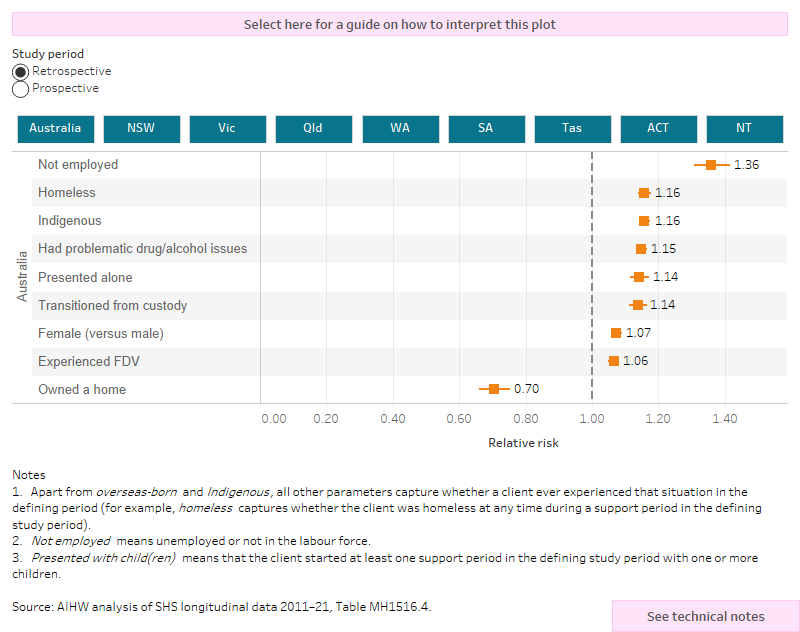
Risk ratios were created to measure the association between the use of SHS services and a set of client characteristics (see Glossary entry on Relative risk for how to interpret the results).
Model results are shown in Figure MH.6, which shows relative risk for having received SHS support in the past and, separately, in the future for chosen client variables. Separate models were created for each state or territory, as well as a national model. Results should be used with caution for states or territories where there were too few clients (less than 3,500) in the cohort for a meaningful model (Table MH.1). Data from these states or territories have been included in the national results, though it is important to recognise that the national data are mostly a reflection of the associations in the largest states. Therefore, while the national data are comprehensive and reflect the pathways of all clients in Australia, they are strongly influenced by the New South Wales and Victorian experience (which together account for 67% of clients) and insensitive to the situation in the smaller states or territories.
Although associations vary in magnitude between states and or territories, having owned a home was associated with reduced likelihood of having a history of SHS support (30% lower likelihood in the national data; Figure MH.6, Table MH1516.4.
Being an Indigenous Australian also had a strong association (16% greater likelihood) with past SHS support. This is partly due to the social and economic disadvantages faced by Indigenous Australians and a higher prevalence of health risk factors (POA 2014, AIHW 2020).
Most other factors, and especially not being employed (36% greater likelihood), having been homeless (16% greater likelihood), transitioning from custody or presenting for support alone at some time (14% greater likelihood), having problematic drug or alcohol issues (15%) or being female (7%) were associated with an increased likelihood of having a history of SHS support.
Figure MH.6: MH clients 2015–16, relative risk for use of SHS services in the retrospective and prospective study periods
The interactive risk ratio plot shows the characteristics or circumstances that are associated with the MH cohort clients use of SHS services in the past (retrospective) or future (prospective period), these associations are presented as relative risks. Relative risks for all states and territories and Australia can be selected and displayed. At the national level, having owned a home was associated with a reduced likelihood of having a history and ongoing use of SHS support. Being an Indigenous Australian also had a strong association, 16% greater likelihood of past support and a 31% greater likelihood of future support.
What client characteristics are associated with using SHS services in the prospective study period?
Descriptive regression models were used to examine the association between client characteristics and clients receiving SHS support into the future. As with the models for past SHS support, analyses were undertaken using national data and separately for states or territories with sufficient sample sizes (at least 3,500 clients; Figure MH.6, Table MH1516.4).
The results largely mirror those for associations with past SHS support. Although different in magnitude in each state or territory, not being employed at some time in the defining study period – specifically, being unemployed or not in the labour force – had the greatest association with future SHS support. Nationally, clients that were not employed at some time were 46% more likely to receive SHS support into the future.
Other factors associated with an increased likelihood of ongoing SHS support include being an Indigenous Australian (30% greater likelihood in the national data). Transitioning from custody in at least one support period (22%), being homeless at some time (20%) and having problematic drug or alcohol issues (19%) were also associated with ongoing SHS support.
Conversely, owning a home at some time in the defining study period was associated with a reduced likelihood of ongoing SHS use (21% reduction).
Summary
Over 54,000 clients aged 18 and over had mental health issues either during their support in 2015–16 or within the preceding 12 months.
Compared with clients without mental health issues, clients with mental health issues in the defining period were more likely to be male, have experienced homelessness and have had drug or alcohol issues. They received more episodes of support than non-mental health clients, were more likely to receive accommodation support, and were more likely to be long-term clients (needed SHS support over the 10-year period).
They were more likely to use services overall, particularly intellectual disability support and counselling for drug/alcohol issues or problem gambling.
One-third of the mental health cohort (33%) had mental health issues when they received support in the past, and over one-third (36%) of clients had mental health issues during future use of services.
Client traits or experiences such as, being not in the labour force or unemployed at some time, being an Indigenous Australian, being homeless or having transitioned from custody were associated with SHS support in the past or future. Having owned a home reduced the likelihood of clients being a historic, ongoing or long-term client.
ABS (Australian Bureau of Statistics) (2016) National Mental Health and Wellbeing: Summary of Results, Australian Bureau of Statistics: Canberra.
AIHW (2020) Health risk factors among Indigenous Australians. Australia's health 2020: snapshots. Australia’s health series no. 17 Cat. no. AUS 232. Canberra: AIHW.
AIHW (2021) Specialist homelessness services annual report, AIHW Cat. no. HOU 322. Australian Institute of Health and Welfare: Canberra.
Ayano G, Tesfaw G and Shumet S (2019) The prevalence of schizophrenia and other psychotic disorders among homeless people: a systematic review and meta-analysis, BMC Psychiatry, 19(370):1-14.
Bentley R, Baker E, Mason K, Subramanian SV and Kavanagh AM (2011) Association between housing affordability and mental health: a longitudinal analysis of a nationally representative household survey in Australia, American Journal of Epidemiology, 1(174):753-60.
Brackertz N, Borrowman K and Roggenbuck C (2020) Trajectories: the interplay between housing and mental health pathways, Australian Housing and Urban Research Institute Limited and Mind Australia (AHURI), Melbourne.
Flatau P, Lester L, Seivwright A, Teal R, Dobrovic J, Vallesi S, Hartley C and Callis Z (2022) Ending Homelessness in Australia: an evidence and policy deep dive, Centre for Social Impact, Crawley.
Gutwinski S, Schreiter S, Deutscher J and Fazel S (2021) ‘The prevalence of mental disorders among homeless people in high-income countries: An updated systematic review and meta-regression analysis’, PLoS medicine, 18(8):e1003750.
Honey A, Nugent A, Hancock N and Scanlan J (2017) It’s hard work, believe me!”: active efforts to optimise housing by people who live with mental illness and access housing assistance, Australian Journal of Social Issues, 52(4):347-366.
Holland JM (2018) Challenges and Considerations for Housing in the Future, Family and Consumer Sciences Research Journal, 47(2):124-129.
Johnson G and Chamberlain C (2011) Are the Homeless Mentally Ill?, Australian Journal of Social Sciences, 46(1):29-48.
Johnson G, Scutella R, Tseng YP. and Wood G (2015) Examining the relationship between structural factors, individual characteristics, and homelessness, AHURI, Melbourne.
Johnstone M, Parsell C, Jetten J, Dingle G and Walter Z (2016) Breaking the cycle of homelessness: Housing stability and social support as predictors of long-term well-being, Housing Studies, 31(4):410-426.
Kaleveld L, Seivwright A, Box E, Callis Z & Flatau P (2018) Homelessness in Western Australia: A review of the research and statistical evidence, Government of Western Australia, Department of Communities, Perth.
Maslow AH (2013) A Theory of Human Motivation, Wilder Publications, Radford.
Moore G, Manias E and Gerdtz MF (2011) Complex health service needs for people who are homeless, Australian Health Review, 35(4):480-485.
Nilsson SF, Nordentoft M, Hjorthøj C (2019) Individual level predictors for becoming homeless and exiting homelessness: A systematic review and meta-analysis, Journal of Urban Health, 96(5):741-50.
NMHC (National Mental Health Commission) (2017) Housing, Homelessness and Mental Health: Outcomes from the National Mental Health Commission’s consultation in 2017. Canberra: National Mental Health Commission, Canberra.
NMHC (2020) ‘Vision 2030: Blueprint for Mental Health and Suicide Prevention’, National Mental Health Commission, Canberra.
Nower L, Eyrich-Garg KM, Pollio DE. and North CS (2015) Problem gambling and homelessness: Results from an epidemiologic study, Journal of Gambling Studies, 31(2): 533-545.
POA (Parliament of Australia) (2004) A hand up not a hand out: Renewing the fight against poverty. Report on Poverty and Financial Hardship. Canberra: Senate Community Affairs Reference Committee.
Productivity Commission (2020) Mental Health, Report no. 95, Productivity Commission, Canberra.
Scutella R, Chigavazira A, Killackey E, Herault N, Johnson G, Moschion J and Wooden (2014) Journeys Home Research Report No. 4, Melbourne Institute, Melbourne.
State of Victoria (2021) Royal Commission into Victoria’s Mental Health System, Final Report, Parl Paper No. 202, Session 2018–21, Government of Victoria, Melbourne, accessed 11 February 2022.
Whittaker E, Dobbins T, Swift W, Flatau P and Burns L (2017) First examination of varying health outcomes of the chronically homeless according to Housing First configuration, Australian and New Zealand journal of public health, 41(3): 306-308.
Van der Laan J, Boersma SN, al Shamma S, Akkermans R, van Straaten B, Rodenburg G, van de Mheen D and Wolf JRLM (2020) Differences in housing transitions and changes in health and self-determination between formerly homeless individuals, European Journal of Public Health, 30(5): 900–905.


