Maternal body mass index
Obesity in pregnancy contributes to increased risks of illness and death for both mother and baby. Pregnant women who are obese have an increased risk of thromboembolism, gestational diabetes, pre-eclampsia, post-partum haemorrhage (bleeding) and wound infections. They are also more likely to deliver via caesarean section. Babies of mothers who are obese have higher rates of congenital abnormality, pre-term birth, stillbirth and neonatal death than babies of mothers who are not obese (RCOG 2018).
Body mass index (BMI) is a ratio of height and weight and is calculated by dividing a person’s weight in kilograms by the square of their height in metres (kg/m2). A healthy range of BMI for non-pregnant women is 18.5 to 24.9. While increases in BMI are expected during pregnancy, a BMI of 25 to 29.9 is defined as overweight in pregnancy and a BMI of 30 or more is defined as obesity in pregnancy. A BMI of less than 18.5 is defined as underweight.
BMI does not necessarily reflect body fat distribution or describe the same degree of fatness in different individuals. At a population level, however, it is a practical and useful measure to identify overweight and obesity (AIHW 2023).
In the NPDC, maternal BMI refers to pre-pregnancy BMI. However, source data and methods used for data collection are not uniform nationally. For example, BMI can be calculated based on self-reported height and weight or on those measured at the first antenatal visit.
Data on maternal BMI were available for mothers in all states and territories for the first time in 2016. Due to the variation in data collection methods between jurisdictions, care must be taken when making comparisons.
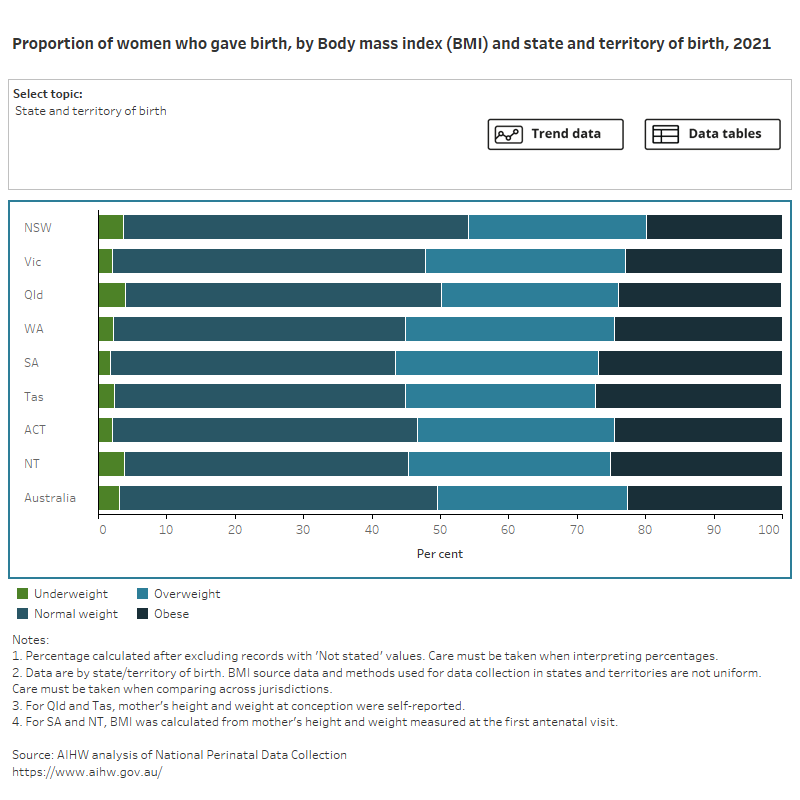
Figure 1 presents data on the BMI of women who gave birth, by selected maternal characteristics, for 2021. Select the trend button to see how data has changed over a 10-year period.
Figure 1: Proportion of women who gave birth, by body mass index (BMI) and selected topic
Bar chart shows body mass index (BMI) by selected topics and a line graph shows topic trends between 2012 and 2021.
In 2021, 28% of mothers were overweight and 23% were obese.
The proportion of mothers who were obese was highest amongst:
- women with a parity of 3 (36%) or 4 or more (42%)
- women who lived in Very remote areas (30%)
- women who lived in the most disadvantaged areas (31%)
- who had a caesarean section birth (29%).
In 2021, 2.7% of mothers were underweight. The proportion was highest amongst teenage mothers (aged under 20) (10%), women who lived in Very remote areas (4.0%) and First Nations mothers (5.7%).
For more information on Body mass index see National Perinatal Data Collection annual update data table 2.19.
References
AIHW (Australian Institute of Health and Welfare) (2023) Overweight and obesity, AIHW, Australian Government, accessed 8 June 2023.
RCOG (Royal College of Obstetricians and Gynaecologists) (2018) Care of women with obesity in pregnancy, green-top guideline number 72, RCOG, accessed 18 January 2021.


