Injury & poisoning hospitalisations
Why are injury and poisoning hospitalisation rates important?
Injury and poisoning have a major, but largely preventable, impact on the health of young Australians. They are a leading cause of hospitalisation among young people and can leave many with serious disability or long-term conditions, such as acquired brain injury or spinal cord injury. This can severely affect their future health and wellbeing as well as their employment, educational and recreational opportunities (AIHW: Pointer 2014; NPHP 2004).
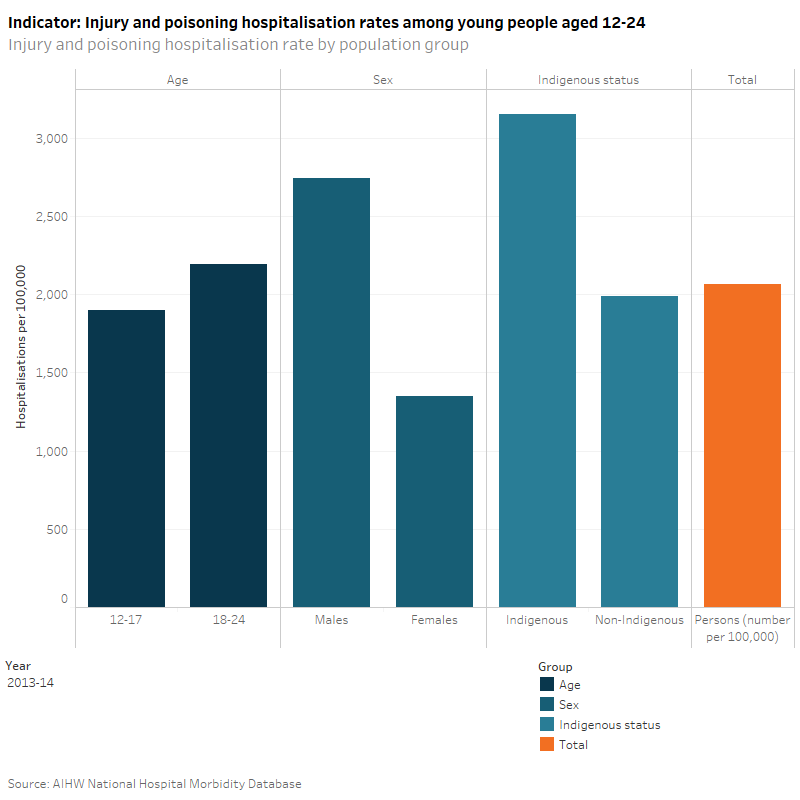
Do rates vary across population groups?
In 2013–14, the rate of hospitalisation due to injury or poisoning among all young people aged 12–24 in Australia was 2,064 per 100,000. Those in the 18–24 age group had a higher rate (2,190 per 100,000) of injury and poisoning hospitalisation than those aged 12–17 years (1,896 per 100,000). Males had a higher rate of hospitalisation than females, with 2,744 per 100,000 and 1,348 per 100,000, respectively. Indigenous young people were more likely to be hospitalised due to injury and poisoning with a rate of 3,153 per 100,000, compared to Other Australians with a rate of 1,986 per 100,000.
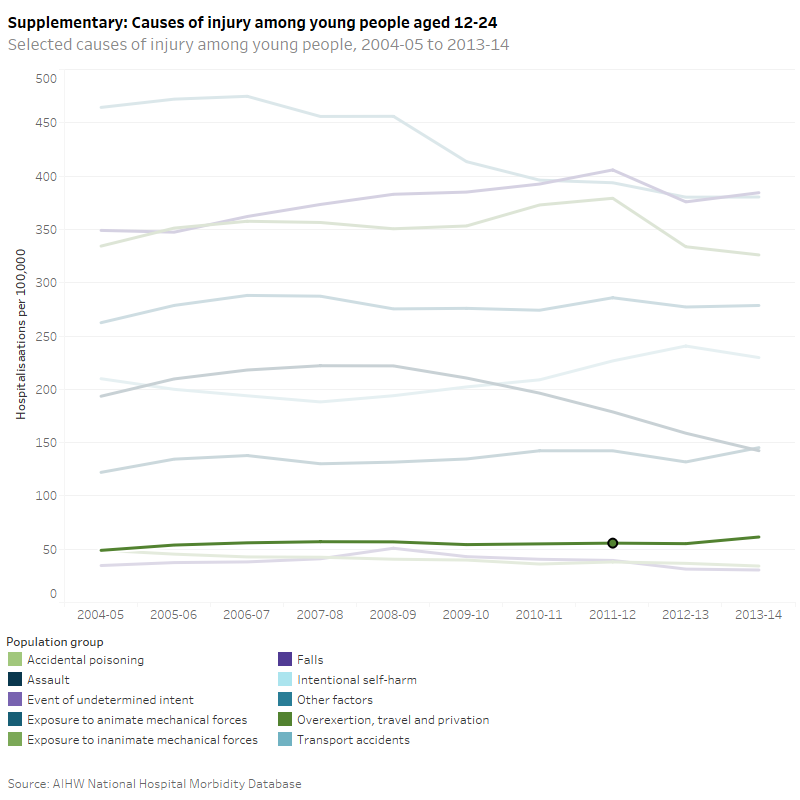
What are the leading causes of injury and poisoning hospitalisations?
In 2013–14, the leading causes of injury and poisoning hospitalisations among young people were falls (385 per 100,000), transport accidents (380 per 100,000) and injury from inanimate mechanical forces (such as being struck or cut by something, exposure to an explosion, or having a foreign body entering through the eye, skin or other orifice) (326 per 100,000).
Has there been a change over time?
From 2004–05 to 2013–14, hospitalisation rates due to injury and poisoning were relatively stable for all young people and among young people of different age groups.
The injury and poisoning hospitalisation rate for males has been declining in recent years, having reached a peak of 3,169 per 100,000 in 2007–08, before decreasing to 2,745 per 100,000 in 2013–14. In contrast, the trend in hospitalisation rate for young females was less pronounced though steadily increasing from 1,236 per 100,000 in 2004–05 to 1,348 per 100,000 in 2013–14.
From 2004–05 to 2013–14, injury hospitalisation rates for Indigenous young people have increased from 2,698 per 100,000 to 3,153 per 100,000. During the same period, injury hospitalisation rates for young Other Australians were 2,100 per 100,000.
The leading causes of injury and poisoning hospitalisations among young people have remained similar since 2004–05.
Injury from inanimate mechanical forces includes injuries sustained from striking against or being stuck by other objects, exposure to other and unspecified inanimate mechanical forces, contact with knife, sword or dagger, contact with glass window. For more detailed information, see ICD-10-AM (International statistical classification of diseases and related health problems, tenth revision, Australian Modification), codes W20-W49. In 2013-14, diagnoses and external cause injury and poisoning were recorded using the eighth edition of the ICD-10-AM. Data from 2004–05 to 2012–13 were coded to earlier editions.
Hospitalisations (referred to elsewhere as hospital separations) refer to episodes of admitted patient care which can be a total hospital stay or a portion of a hospital stay, beginning or ending in a change of type of care (for example, from acute care to rehabilitation). To reduce over-counting of injury cases, records have been omitted where the mode of admission is recorded as a transfer from another acute-care hospital.
Indigenous data is for 6 States (NSW, Vic, Qld, WA, SA and public hospitals in the NT) as these states are considered to have sufficient completeness of Indigenous identification for analysis from 2004–05 onwards. ACT and Tasmania are considered to have sufficient completeness of Indigenous identification from 2010–11 onwards; however, they are excluded for the purposes of time series analysis. Consequently, the Indigenous data may not necessarily be representative of the excluded jurisdictions.
Changes in the quality of the Indigenous identification over time may affect the time series for data presented for data by Indigenous status (i.e. categories ‘Indigenous’ and ‘Other Australians’).
‘Other Australians’ includes records for persons identified as not Indigenous as well as records where Indigenous status was not stated.
The hospitals admitted patient care data do not include non-admitted presentations to hospital (eg non-admitted patients in emergency departments).
AIHW National Hospital Morbidity Database
Data quality statement: AIHW METeOR
AIHW (Australian Institute of Health and Welfare): Pointer S 2014. Hospitalised injury in children and young people 2011–12. Injury research and statistics series no. 91. Cat. no. INJCAT 167. Canberra: AIHW.
NPHP (National Public Health Partnership) 2004. The National Injury Prevention and Safety Promotion Plan: 2004-2014. Canberra: NPHP.


