Cervical cancer prevention
What is cervical cancer and how can it be prevented?
Cervical cancer affects the cells of the uterine cervix, which is the lower part (or ‘neck’) of the uterus where it joins the inner end of the vagina. Cervical cancer develops when abnormal cells in the lining of the cervix begin to multiply out of control and form precancerous lesions. If undetected, these lesions can develop into tumours and spread into the surrounding tissue (AIHW 2015).
Cervical cancer is a rare outcome of persistent infection with one or more oncogenic (cancer-causing) types of human papillomavirus (HPV) (Bosch et al. 2002; Walboomers et al. 1999). Infection with one or more of these oncogenic types of HPV (known as ‘high-risk’ HPV) is the underlying cause of almost all cases of cervical cancer (AIHW 2015).
Currently 15 high-risk types of HPV are recognised. HPV types 16, 18, and 45 are most predominantly associated with cervical cancer, with HPV types 16 and 18 detected in 70–80% of cases of cervical cancer in Australia (Brotherton 2008).
Overall, Australia has a low incidence of cervical cancer and one of the lowest mortality rates from cervical cancer in the world (AIHW 2015). In Australia, primary prevention of cervical cancer is through vaccination against high-risk HPV types 16 and 18 (National HPV Vaccination Program). Secondary prevention is through cervical screening (the National Cervical Screening Program). From 1 May 2017 a HPV test will replace the Pap test and women will be advised to commence cervical screening from age 25. Cervical cancer in women under the age of 25 is rate, and screening women under the age of 25 has not changed the number of cervical cancer amongst this age group. HPV vaccination will continue to reduce the risk of cervical cancer in young women.
Vaccinations
The National HPV Vaccination Program was introduced in 2007 and initially targeted 12–13 year old females delivered through an ongoing school-based program, with a catch up program for females aged 13–26 years in place until 2009. Males aged 12–13 years have also been included in the program since 2013, with a two-year catch-up for males aged to 14–15 years. Data on males was not available at the time of preparing this portal.
Screening
Cervical cancer is one of the few cancers that has a precancerous stage that lasts for many years prior to the development of invasive disease. The National Cervical Screening Program provides an opportunity to treat abnormalities in their precancerous stage, before any possible progression to cervical cancer. Some rare (and often aggressive) cervical cancers, however, do not have a precancerous stage, and therefore are simply unable to be detected by cervical screening.
Are vaccination and screening rates improving over time?
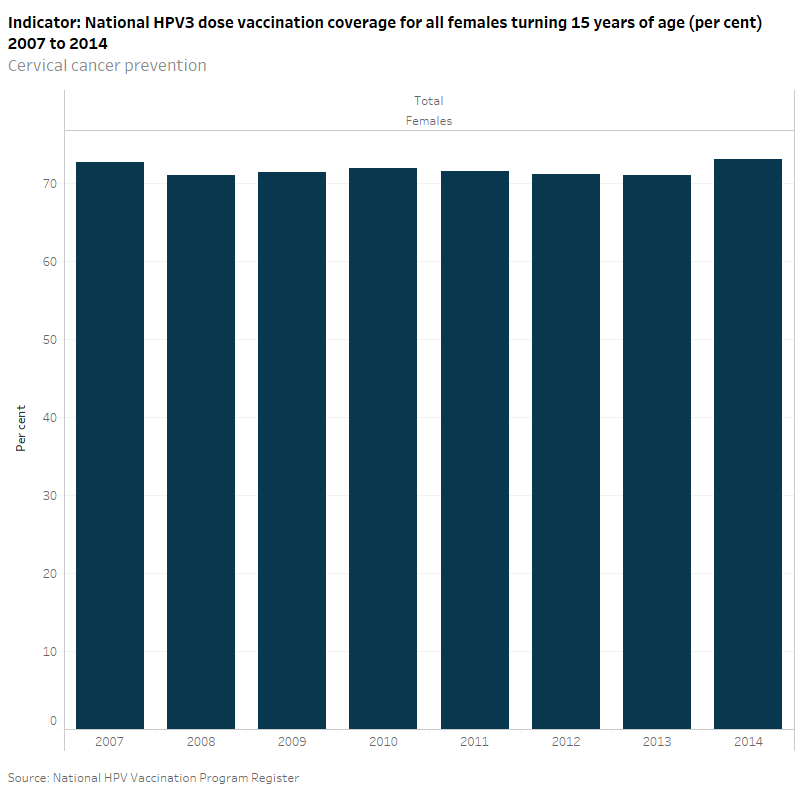
According to the National HPV Vaccination Program Register, the national HPV 3 dose vaccination coverage for all females turning 15 years of age has remained relatively stable since the introduction of the vaccination in 2007 to 2014 (around 73%).
Early data on cervical abnormalities, genital warts and HPV prevalence in cervical specimens suggest the impact of this program has been rapid and substantial, and that it also provided some indirect protection for young unvaccinated females and young males (National HPV Vaccination Program 2015).
According to the State and Territory Cervical Cytology Register, the rate of participation among young women aged 20–24 in the National Cervical Cancer Screening Program rose from 50% in 1996–97 to its highest point in 1998–99 at 54%. In the last 3 reporting periods (2010–11 to 2012–13) the rate has remained relatively stable at around 43%. In 2012–13 cervical screening rates were lower among 20–24 year olds (43%) than older age groups (AIHW 2015).
What is the level of awareness of HPV among young people?
Based on data from the Fifth National Survey of Secondary Students and Sexual Health (2013), HPV knowledge among young people in Years 10, 11 and 12 is very poor. In most cases more than half the sample reported that they were ‘unsure’ of the correct answer to questions about HPV knowledge. On most of the items relating to HPV knowledge, young women had higher rates of knowledge than young men. This has been attributed to the vaccine having been offered to young women for a longer period of time than to young men (Mitchell et al. 2014).
Consistent with the World Health Organisation recommendations the age used to report on HPV coverage in Australia is 15 years (which allows time for all doses to be administered and to account for different age at entry to high school in different states and territories) (National HPV Vaccination Program Register 2015).
Since 2013, males aged 12–13 years have also been included in the National HPV Vaccination Program, with a two-year catch-up for males aged to 14–15 years. At the time of preparing this portal, comprehensive data on males was not yet available.
National Indigenous data is not available for HPV vaccination coverage, with the only states reporting by Indigenous status with sufficient accuracy for publication being NT and Qld.
Not all women are sexually active and therefore at risk of cervical cancer. However, as there are no data on the group at risk (that is, those that are sexually active) screening rates are calculated using the ABS estimated resident population.
National participation rates in cervical screening for Aboriginal and Torres Strait Islander women are not available due to Indigenous status information not being collected on pathology forms in all jurisdictions, although there is evidence that this population group is under-screened (AIHW 2015).
For more information, see the National HPV Vaccination Program Register 2015, and Cervical screening in Australia 2012–13.
National HPV Vaccination Program Register
State and Territory Cervical Cytology Register
National Survey of Australian Secondary Students and Sexual Health 2008
National Survey of Australian Secondary Students and Sexual Health 2013
Data quality statements: Please see the published sources (above) for further information
Australian Institute of Health and Welfare (AIHW) 2015. Cervical screening in Australia 2012–2013. Cancer series no. 93. Cat. no. CAN 91. Canberra: AIHW.
Bosch FX, Lorincz A, Muñoz N, Meijer CJ & Shah KV 2002. The causal relation between human papillomavirus and cervical cancer. Journal of Clinical Pathology 55(4):244–65.
Brotherton JM 2008. How much cervical cancer in Australia is vaccine preventable? A meta-analysis. Vaccine 26(2): 250-56.
Mitchell A, Patrick K, Heywood W, Blackman P, Pitts M 2014. 5th National Survey of Australian Secondary Students and Sexual Health 2013 (ARCSHS Monograph Series No. 97), Australian Research Centre in Sex, Health and Society, La Trobe University, Melbourne, Australia.
National HPV Vaccination Program Register 2015. Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV et al. 1999. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. Journal of Pathology 189(1):12–19.


