Mental health
Why are rates of mental disorders important?
Mental health is a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community (WHO 2014). Conversely, mental health problems and illnesses affect the perceptions, emotions, behaviour and resulting social wellbeing of individuals.
Poor mental health can impact on the potential of young people to live fulfilling and productive lives (WHO 2014). It is strongly related to other health and developmental concerns in young people, notably lower educational achievements and occupational attainment, substance use, violence and poor reproductive and sexual health (Bhatia & Bhatia 2007, Patel et al. 2007; Sawyer et al. 2007; Smart & Sanson 2005). Young people with mental disorders may also experience stigma, which often leads to isolation and discrimination (Corrigan 2005). Poor mental health among young people can be a precursor to self-harm, thoughts about suicide, and suicide.
There is strong evidence that mental disorders in childhood and adolescence predict mental disorders in adulthood (Lahey 2015). However, the causal links are less clear. Different explanations have been proposed for the predictive association. Experiencing mental health problems in childhood may increase the risk for adult psychopathology. Alternatively, some genetic and environmental factors that cause psychopathology across the lifespan may operate in childhood. Another explanation is that the predictive association between child and adult psychopathology could reflect chronic or intermittent exposures to conditions (for example chronic economic instability, a lack of stable social support) that give rise to psychopathology when encountered across a lifespan (Lahey 2015).
Mental disorders amongst 12-17 year olds
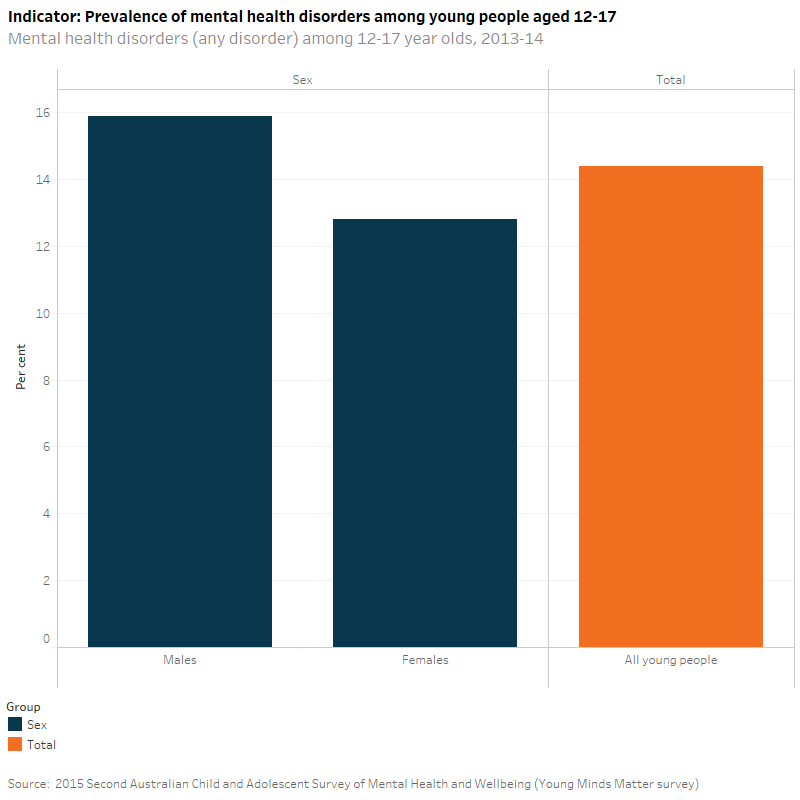
According to the 2013–14 Mental Health of Children and Adolescents survey, 14% (245,000) of young people aged 12–17 had a mental disorder in the 12 months prior to the survey. Males aged 12–17 had a higher prevalence of mental disorders (16%) than females aged 12–17 years (13%), although this difference was not statistically significant.
Anxiety disorders (for example, social phobia, separation anxiety disorder, generalised anxiety disorder and obsessive-compulsive disorder) were the most common type of disorder among 12–17 year olds, accounting for almost half of all mental disorders (7.0%) in this age group. This was followed by Attention Deficit Hyperactivity Disorder (ADHD) (6.3%) and major depressive disorder (5.0%). Conduct disorders were the least common type of mental disorder (2.1%). For 44% of 12–17 year olds with a mental disorder, the impact of the disorder was mild. However, for one in three (33%) it was moderate, and for over 1 in 5 (23%) it was severe.
Has there been a change between 1998 and 2013-14?
There were a number of significant methodological differences between the Mental Health of Children and Adolescents: Report on the Second Australian Child and Adolescent Survey of Mental Health and Wellbeing (Young Minds Matter survey) and the first child and adolescent survey conducted in 1998. However, it is possible to compare the prevalence data for three mental health disorders (major depressive disorder, ADHD and conduct disorder). Between the first (1998) and second (2013–14) national survey of the mental health and wellbeing of Australian children and adolescents, the prevalence of major depressive disorder among 12-17 year olds increased from 2.9% to 5.0%. While the prevalence of ADHD decreased from 7.1% in 1998 to 6.3% in 2013–14, the difference was not statistically significant. There was no real change in the prevalence of conduct disorders (2.2% in 1998 and 2.1% in 2013–14).
Mental disorders amongst 16-24 year olds
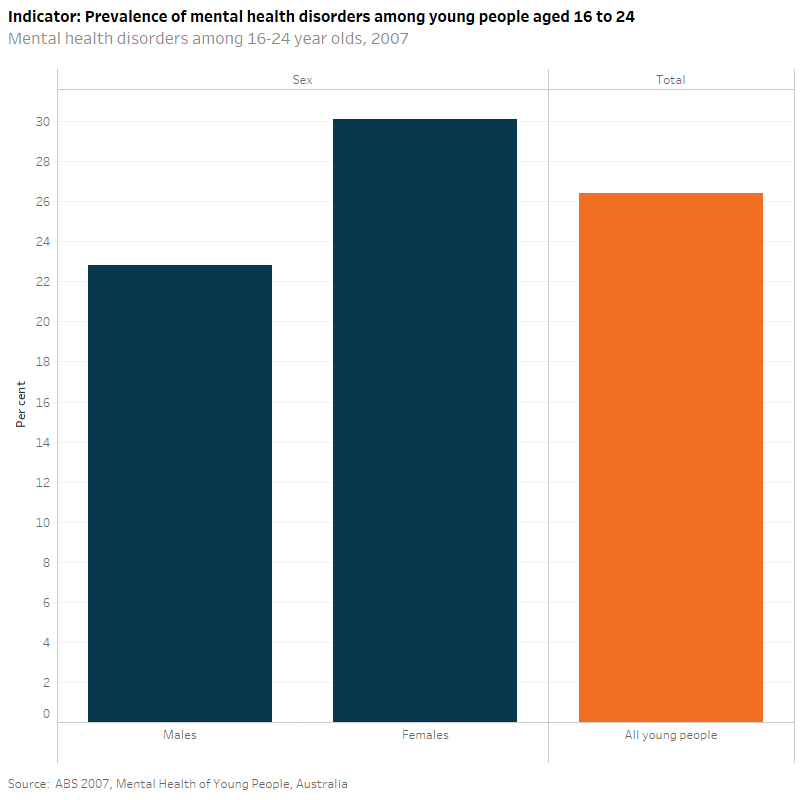
According to the 2007 ABS National Survey of Mental Health and Wellbeing around one in four young people aged 16–24 (26% or 671,100) experienced a mental disorder in the 12 months prior to the survey. This was the highest of any age group in the study which looked at 16–85 year olds. Females aged 16–24 were more likely than males to have experienced a mental disorder (30% versus 23%, respectively).
Females were also more than twice as likely to report having an anxiety disorder (22%) compared to affective (8.4%) or substance use disorders (9.8%). Anxiety disorders (for example panic disorder, agoraphobia, social phobia, generalised anxiety disorder, obsessive-compulsive disorder, and post-traumatic stress disorder) were the most common type of disorder among 16–24 year olds (15%) followed by substance use disorders (alcohol harmful use, alcohol dependence and drug use disorders) (13%). Affective disorders (depressive episodes, dysthymia and bipolar affective disorder) were the least common (6.3%). Males were most likely to report having a substance use disorder (16%), followed by anxiety disorders (9.3%) and then affective disorders (4.3%). Note, that survey participants could have experienced more than one type of disorder, and so the sum of disorder types described above does not equal the total proportion of young people with a mental health disorder (26%).
Psychological distress among young Indigenous 18–24 year olds
Psychological distress refers to an individual’s overall level of psychological strain or pain, evidenced by psychological states such as depression, anxiety and anger. The Kessler Psychological Distress Scale can be used as a proxy for mental health status (CDC 2015).
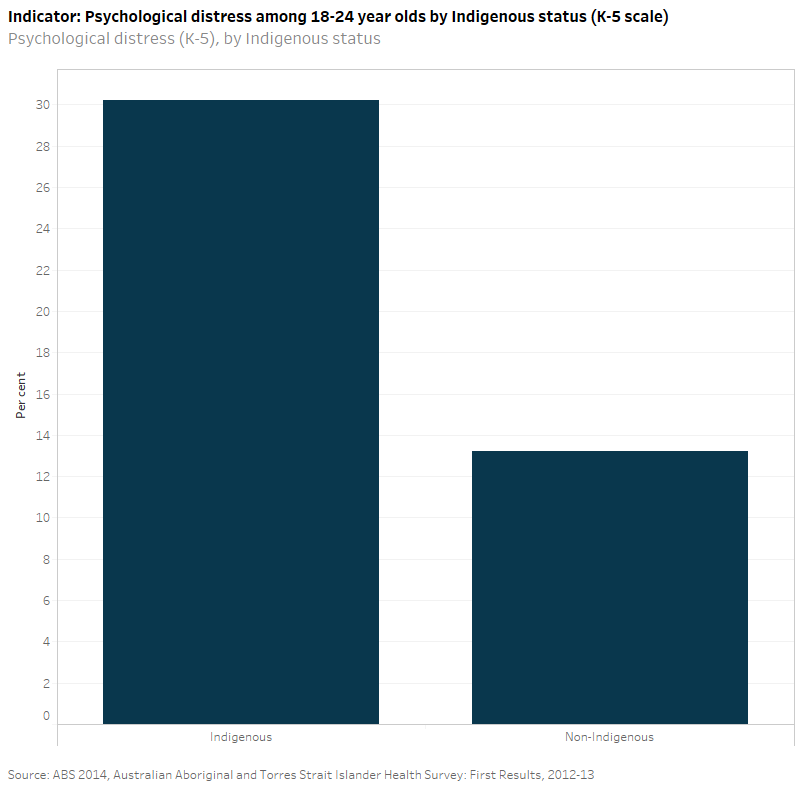
According to the 2012–13 ABS Aboriginal and Torres Strait Islander Health Survey, based on the Kessler 5 (see below for further information), the proportion of Indigenous young adults (aged 18–24) experiencing high or very high levels of psychological distress (30%) in the 4 weeks prior to the survey was more than double the proportion of non-Indigenous young adults (13%).
Data on psychological distress for Indigenous young people is available from the 2008 ABS National Aboriginal and Torres Strait Islander Social Survey and the 2012–13 ABS Australian Aboriginal and Torres Strait Islander Health Survey. The proportion of Indigenous young people experiencing high or very high levels of psychological distress appears to have decreased slightly from 33% in 2008 to 30% in 2012–13, however this difference is not statistically significant. Prevalence of high/very high psychological distress among non-Indigenous young people remained the same (13.3% and 13.2% respectively).
Significance testing: this report is based on survey data; relative standard errors and 95% confidence intervals are provided in the Source data tables: NYIF indicators.
Significance testing was undertaken on values cited in the text; unless otherwise stated, differences were found to be statistically significant.
Mental disorder status were assessed based on meeting the criteria of the Diagnostic and Statistical Manual of Mental Disorders Version IV (DSM-IV) within the 12 months prior to the survey. For more information, see 2015 Second Australian Child and Adolescent Survey of Mental Health and Wellbeing
Psychological distress in the 2012–13 ABS Australian Aboriginal and Torres Strait Islander Health Survey was based on the ‘Kessler-5’ scale. This scale, which consists of 5 questions from the Kessler Psychological Distress Scale, measures levels of negative emotional states experienced by respondents in the 4 weeks prior to interview. A high score may be associated with the person having feelings of anxiety or depression regularly, whereas a low score indicates that the person has these feelings less often or not at all.
ABS 2007 Australian Survey of Mental Health and Wellbeing
ABS 2008. National Aboriginal and Torres Strait Islander Social Survey
ABS 2012–13 Australian Aboriginal and Torres Strait Islander Health Survey
2013–14 Second Australian Child and Adolescent Survey of Mental Health and Wellbeing (Young Minds Matter survey).
Data Quality Statements: Please refer to the published sources (above) for further information.
ABS (Australian Bureau of Statistics) 2007. Mental Health of Young People, Australia. ABS cat. no. 4840.0.55.001. Canberra: ABS.
Bhatia SK & Bhatia SC 2007. Childhood and adolescent depression. American Family Physician 75(1):73–80.
CDC (Centers for Disease Control and Prevention) 2015. Mental Health: Non-specific Psychological Distress Surveillance Data Sources.
Corrigan PW, Editor 2005. On the stigma of mental illness: practical strategies for research and social change. Washington, DC: American Psychological Association.
Lahey BB 2015. Editorial: Why are children who exibit psychopathology at high risk for psychopathology and dysfunction in adulthood. JAMA Psychiatry, July 15, 2015.
Lawrence D, Johnson S, Hafekost J, Boterhoven de Haan K, Sawyer M, Ainley J, Zubrick S 2015. The mental health of children and adolescents: report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Department of Health, Canberra. Viewed on 11 August 2015.
Patel V, Flischer AJ, Hetrick S, & McGorry P 2007. Mental health of young people: a global public-health challenge. The Lancet 369(9569):1302–1313.
Sawyer MG, Miller-Lewis LR and Clark JJ 2007. The mental health of 13-17-year-olds in Australia: findings from the National Survey of Mental Health and Wellbeing. Journal of Youth Adolescence 36:185-94.
Smart D & Sanson A 2005. What is life like for young Australians and how well are they faring? Family Matters 70:46-53.
WHO (World Health Organization) 2014. Mental Health: a state of well-being.


